Chapter 3 Pediatrics
Edward Richer
3 Questions and Answers
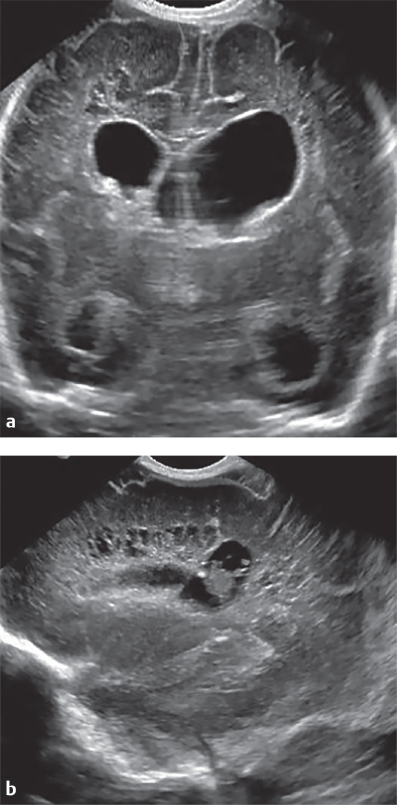
Question 3.1: Which is true regarding the key finding in image (a) ?
It is most commonly the sequela of prematurity.
It is commonly associated with other structural abnormalities, including Chiari I and II.
Frequent cause of hydrocephalus.
Occurs due to an abnormality of posterior to anterior development.
Answer:
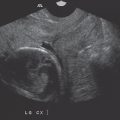
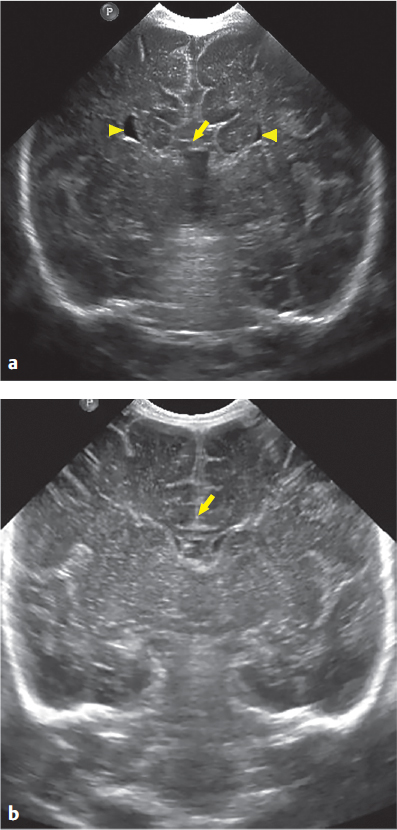
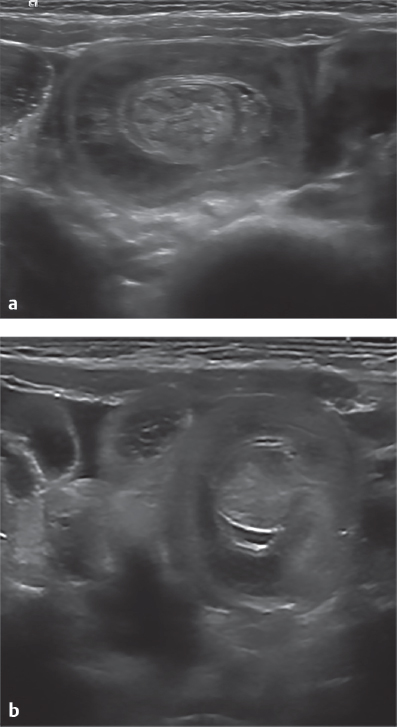
B. Correct. This coronal image from a cranial ultrasound demonstrates agenesis of the corpus callosum (ACC), which is commonly associated with other structural brain anomalies, including Chiari malformations. Note the absence of the normal thin, hypoechoic corpus in image (a, arrow), compared to the normal corpus in image (b, arrow). Also note the widely spaced lateral ventricles (arrowheads), a finding which has been termed the “Texas Longhorn” or “Bullwinkle” sign.
A. Incorrect. ACC is a developmental disorder, not related to prematurity.
C. Incorrect. ACC in and of itself does not cause hydrocephalus.
D. Incorrect. The corpus callosum develops in an anterior to posterior direction.
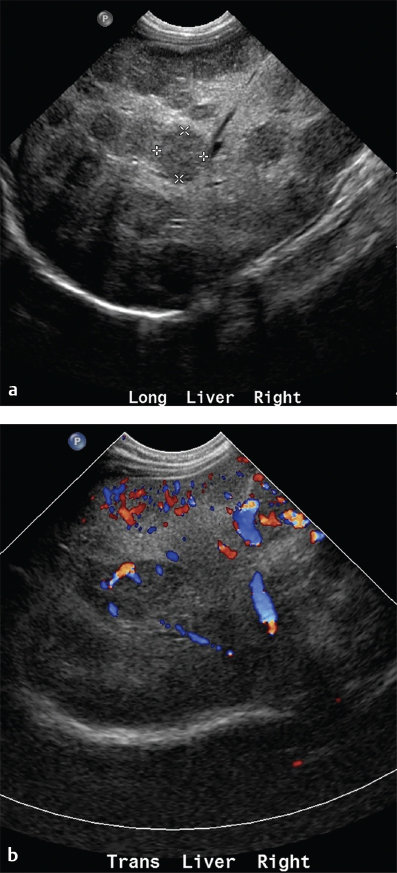
Question 3.2: What is the most reliable sonographic feature of this diagnosis?
Diameter greater than 6 mm.
Free fluid in the right lower quadrant.
Abnormal hyperemia.
Increased echotexture of adjacent fat.
Answer:
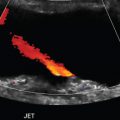
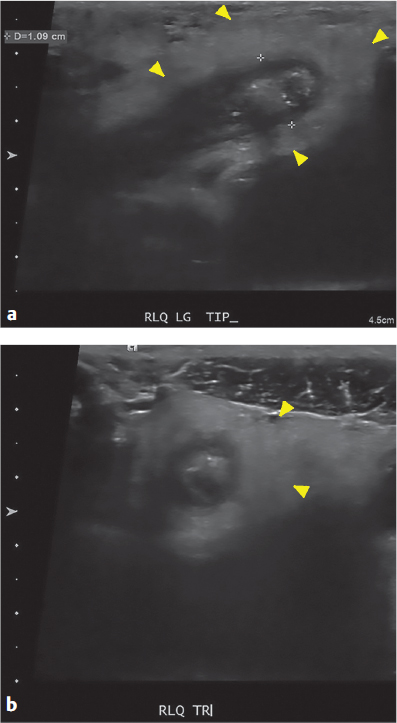
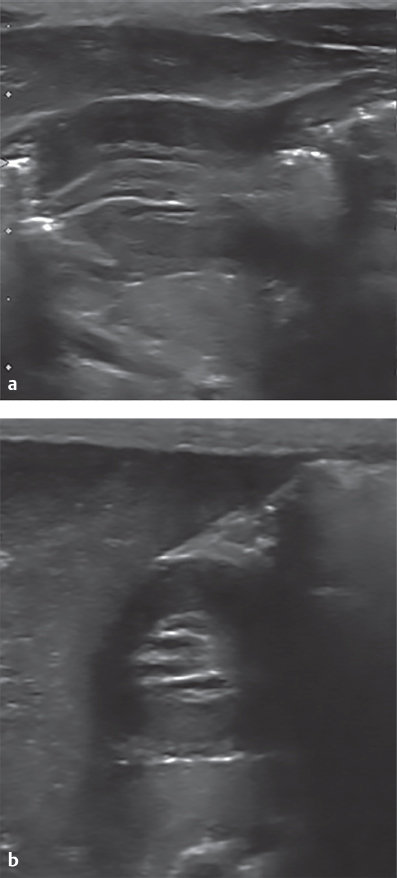
D. Correct. Longitudinal and transverse images demonstrate a dilated appendix measuring 1.1 cm with loss of normal wall echotexture, shadowing appendicolith, and increased echotexture of the periappendiceal fat (arrowheads). Multiple sonographic features are considered in the diagnosis of acute appendicitis, including diameter, presence of appendicolith, hyperemia, echogenic fat, free fluid, and presence of abscess; however, echogenic fat has been shown to have the strongest association with acute appendicitis, odds ratio 63–69.
A. Incorrect. There is overlap between abnormal and normal cases, with some normal appendices measuring over 6 mm and some abnormal cases less than 6 mm. Odds ratio 13–15.
B. Incorrect. Free fluid is nonspecific and has an odds ratio of 1.7 for appendicitis.
C. Incorrect. Abnormal hyperemia has a greater odds ratio for appendicitis than diameter (OR = 21), but not as great as echogenic fat.
Question 3.3: Which is true regarding this condition?
The patient may have presented with crampy abdominal pain and bloody stools.
The patient is typically taken immediately to surgery.
No treatment is required as this condition is usually transient and resolves spontaneously.
The patient is likely in the age range of 5 to 7 years.
Answer:
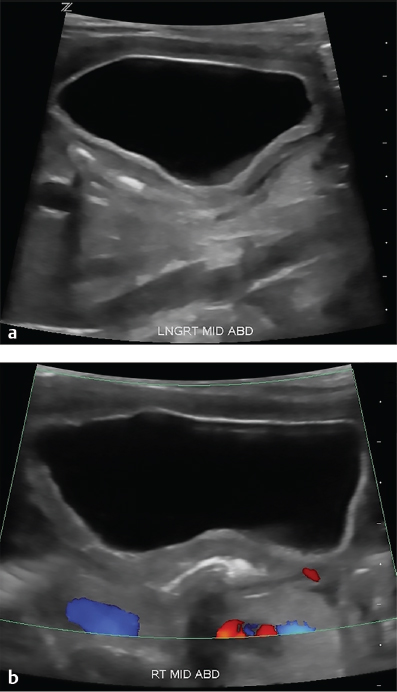
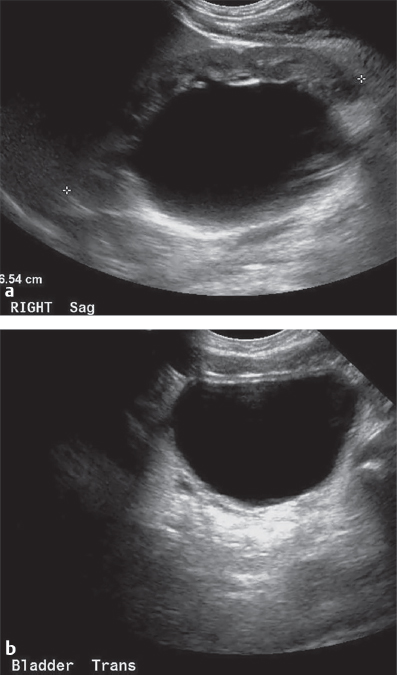
A. Correct. Transverse images demonstrate the typical targetoid appearance of an ileocolic intussusception. Patient symptoms are variable, but may include fussiness, lethargy, intermittent crampy or colicky abdominal pain, and occasionally, bloody stools. Radiographs are normal in up to 50% of cases, and for this reason, ultrasound is the first-line test for intussusception. Classic findings include the “target” sign on transverse images and the “pseudokidney” sign on longitudinal images.
B. Incorrect. Therapeutic enema in radiology is typically attempted prior to surgical intervention.
C. Incorrect. Ileocolic intussusception requires definitive treatment with enema or surgery to prevent bowel ischemia. Enteroenteric intussusceptions are smaller and are generally transient in nature.
D. Incorrect. The typical age range for idiopathic ileocolic intussusception is 3 months to 3 years. An older patient with intussusception raises the possibility of a pathologic lead point.
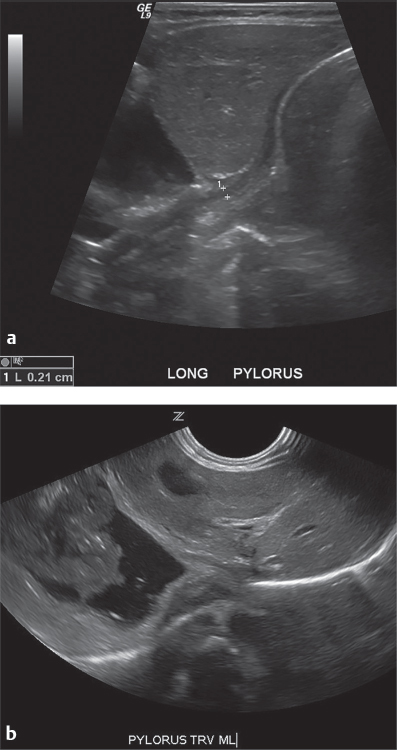
Question 3.4: Technical factors which could obscure the area of interest and prevent accurate diagnosis of this condition include all but which of the following options?
Overdistention of the stomach, displacing the pylorus posteriorly.
Patient in right anterior oblique (RAO) position, causing shadowing gas to collect in the gastric antrum and pylorus.
Imaging the patient while actively feeding from a bottle.
Imaging for a short duration, 1 to 2 minutes.
Answer:
C. Correct. Longitudinal and transverse images through the pylorus show an abnormally thick-walled and elongated pylorus consistent with hypertrophic pyloric stenosis (HPS). Criteria for HPS include a muscle wall thickness ≥3 mm and a channel length ≥17 mm. Having the patient drink formula, breast milk, or sugar water is often utilized during ultrasound to partially distend the stomach and visualize gastric contents emptying through the pylorus.
A. Incorrect. An overdistended stomach causes the pylorus to be displaced posteriorly/deeper into the abdomen, which can then limit visualization.
B. Incorrect. RAO position causes gas to collect in the distal stomach and may obscure visualization. If this occurs, rolling the patient into left anterior oblique position may displace gas away from the pylorus.
D. Incorrect. Imaging for a short duration may inaccurately diagnose transient pyloric thickening from pylorospasm as true HPS.
Question 3.5: Which finding in this case is most suggestive of the correct diagnosis?
Alternating echogenic and hypoechoic layers.
Absence of vascular flow.
Location within the abdomen.
Size of the lesion.
Answer:
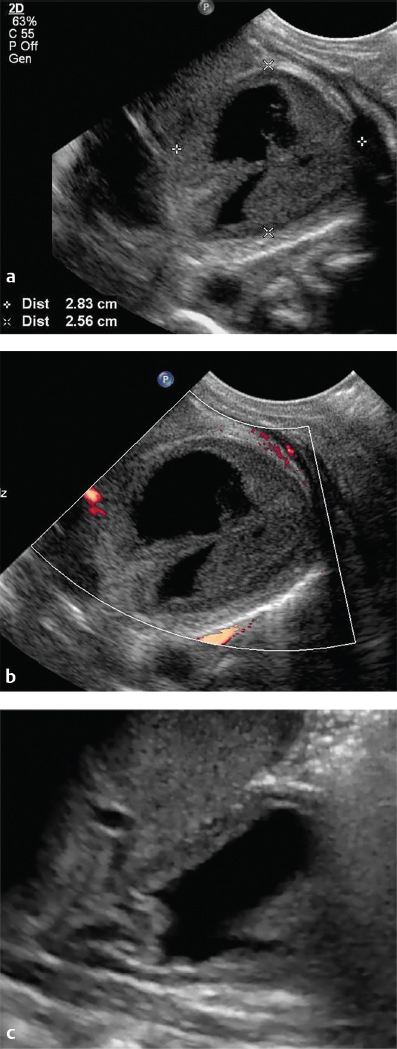
A. Correct. A cystic structure is demonstrated in the right mid abdomen with a wall consisting of alternating echogenic and hypoechoic layers, also known as “gut signature.” The inner echogenic layer represents mucosa, while the hypoechoic layer represents the muscularis layer in this gastrointestinal duplication cyst. Occasionally, the outer echogenic serosal layer can also be seen. This alternating wall echotexture strongly suggests the diagnosis of gastrointestinal duplication cyst over other abdominal cysts, such as choledochal or ovarian cysts, or meconium pseudocysts.
B. Incorrect. Absence of vascular flow does not differentiate between pediatric abdominal cysts.
C. Incorrect. Gastrointestinal duplication cysts can occur anywhere in the abdomen, and ovaries/ovarian cysts can be large or located high in the abdomen in newborn females.
D. Incorrect. The size of the lesion does not reliably differentiate pediatric abdominal cysts.
Question 3.6: Which other organ is most likely to be affected in this newborn infant?
Pancreas.
Adrenals.
Spleen.
Liver.
Answer:
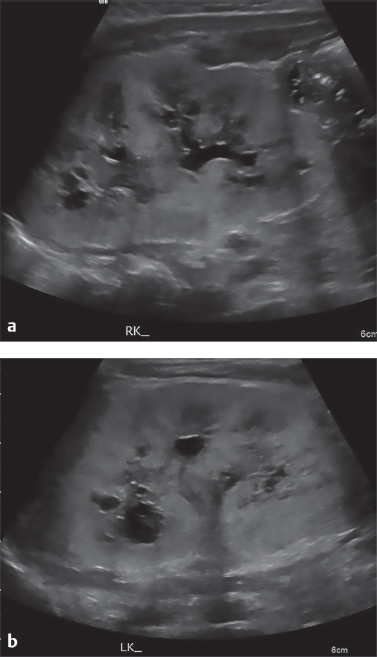
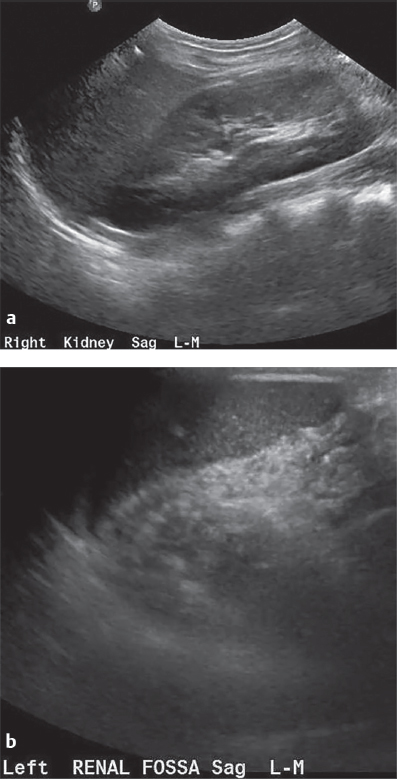
D. Correct. Sagittal images of both kidneys in this newborn infant demonstrate bilateral enlarged, echogenic kidneys with numerous small cysts consistent with autosomal recessive polycystic kidney disease (ARPKD). Infants with ARPKD classically present with Potter sequence sequelae and pulmonary hypoplasia due oligohydramnios in utero. The liver is also affected in ARPKD, typically inversely proportional to the severity of renal involvement. Liver fibrosis and cysts are the most commonly encountered findings.
A, B, C—Incorrect. The mentioned organs are not typically involved in ARPKD.
Question 3.7: Based on the ultrasound images, which of the following option would you recommend?
Abdominal ultrasound to evaluate for liver hemangiomas.
Chest computed tomography (CT) to evaluate for arteriovenous malformations (Osler–Weber–Rendu syndrome).
Chest radiograph to evaluate for heart failure.
Positron emission tomography (PET)-CT to evaluate for associated metastases.
Answer:
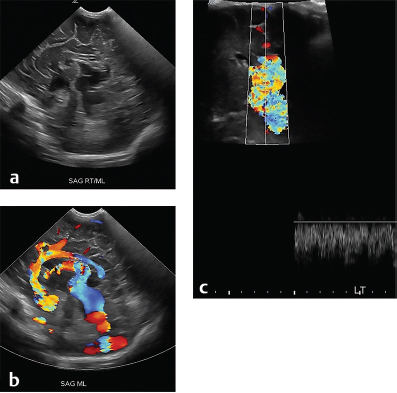
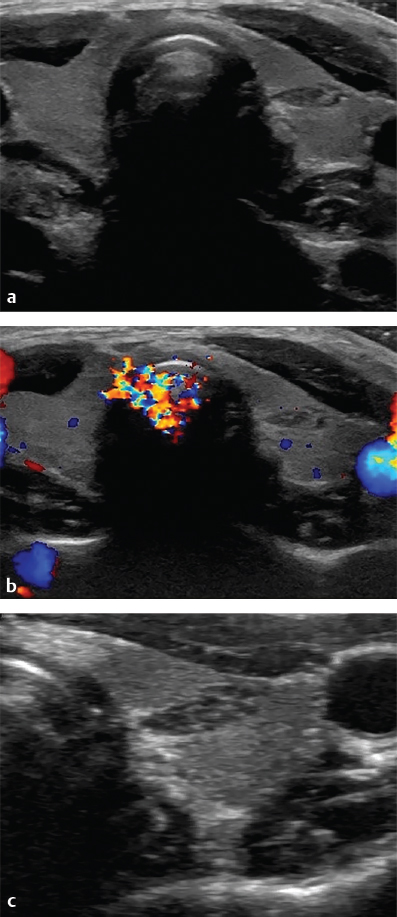
C. Correct. Sagittal images from a cranial ultrasound show an abnormal, prominent vascular structure with venous blood flow in the posterior aspect of the brain in this neonate. The location and ultrasound appearance are characteristic for vein of Galen (VOG) malformation, or median prosencephalic arteriovenous fistula. This is a rare malformation, but is classically associated with high output heart failure due to arteriovenous shunting, with up to 80% of cardiac output shunting through the lesion. A chest radiograph would help to assess for heart failure.
A, B, D—Incorrect. VOG malformation is not associated with liver hemangiomas.
Question 3.8: The Doppler examination in this infant with elevated liver enzymes is best described as which of the following?
Normal hepatic artery and portal venous flow and waveforms.
Normal hepatic artery flow and waveforms, reversed flow, and arterialized waveform in portal vein.
Parvus tardus waveform in hepatic artery indicative of arterial stenosis, normal portal vein flow.
Normal hepatic artery flow, abnormal portal vein Doppler is artifactual due to incorrect Doppler angle settings.
Answer:
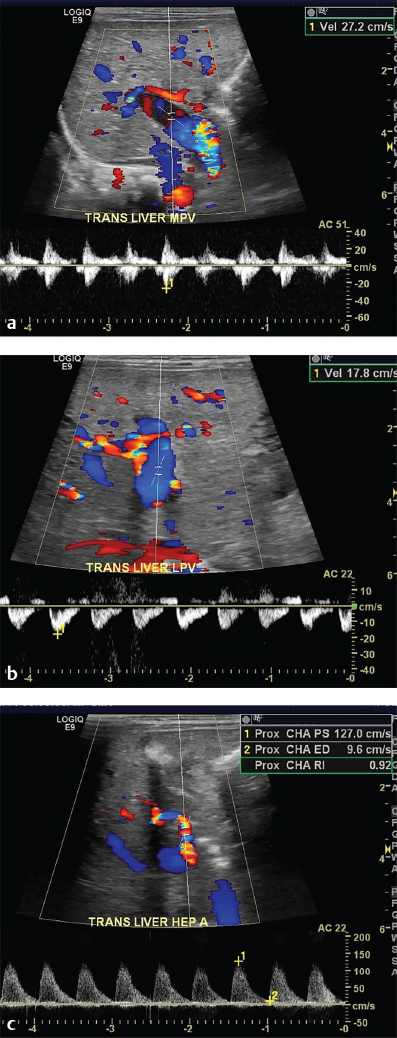
B. Correct. Doppler imaging of the liver shows abnormal reversal of blood flow in the main and left portal vein with arterialized waveforms. The hepatic artery waveforms and direction of flow are normal. Portal vein flow should be toward the transducer (hepatopetal), except in the posterior division of the right portal vein in which flow is away from the transducer due to the anatomy of the portal vein. Reversal of portal vein flow can be seen in severe portal hypertension, or in arteriovenous shunting, which was the diagnosis in this case.
A. Incorrect. The portal vein flow and waveforms are abnormal.
C. Incorrect. The arterial waveform is normal and does not show parvus tardus morphology.
D. Incorrect. The Doppler angle appears appropriately selected and would not produce an arterialized portal vein waveform even if incorrectly selected.
Question 3.9 In a patient with this condition, constant urinary incontinence or dribbling may be an indication of what finding? What imaging study could further evaluate for that finding?
Ectopic ureter inserting on the urethra or vagina; magnetic resonance urography could be performed.
Detrusor muscle instability; urodynamic study could be performed.
Severe hydronephrosis; MAG3 exam with Lasix could be performed.
Neurogenic bladder; fluoroscopy cystogram could be performed.
Answer:
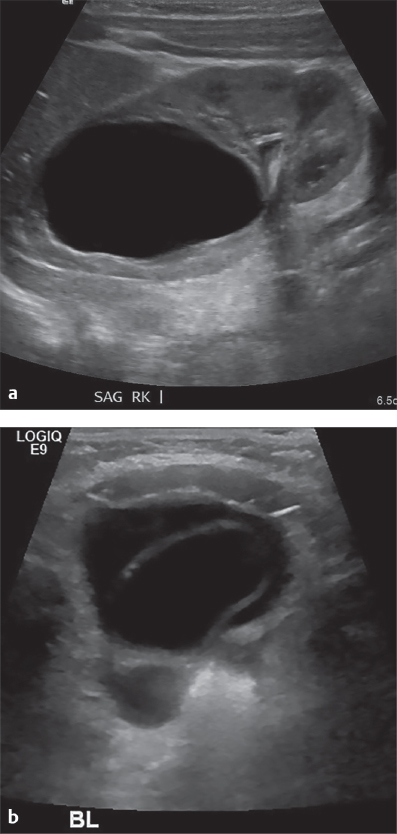
A. Correct. The images demonstrate a renal duplication, with asymmetric collecting system dilatation in the upper pole of the right kidney, and a right-sided ureterocele within the bladder. In renal duplications, the upper moiety ureter tends to insert inferomedially (Weigert-Meyer rule), and in some cases it may insert ectopically on structures other than the bladder, such as vagina, urethra, or seminal vesicles. Insertion on a structure without a sphincter mechanism, such as the vagina, can produce constant urinary dribbling and incontinence. Magnetic resonance (MR) urography would be the best choice for further imaging in children, as the ectopic insertion would be well demonstrated without exposing the patient to radiation.
B. Incorrect. Detrusor muscle instability could produce intermittent incontinence, but not constant wetness as in this patient.
C. Incorrect. Hydronephrosis would not produce incontinence.
D. Incorrect. Neurogenic bladder could produce intermittent incontinence, but not constant wetness as in this patient.
Question 3.10 Newborn infant undergoing ultrasound for hydronephrosis detected on prenatal ultrasound. A left suprarenal space lesion was incidentally discovered when imaging the left kidney, shown in the images below. What are your recommendations for management?
Urgent referral to pediatric surgeon for resection.
Abdominal MRI for further characterization.
Short-term follow-up ultrasound.
Image-guided biopsy by interventional radiology.
Answer:
C. Correct. The images show a complex solid and cystic left suprarenal mass. In a newborn infant, the main differential diagnosis is adrenal hemorrhage and neonatal neuroblastoma. The lack of blood flow on Doppler imaging is more suggestive of hemorrhage. Since neonatal neuroblastoma has a relatively good prognosis, an adrenal mass in a newborn can be safely followed by short-term ultrasound to evaluate for changes. On follow-up imaging, there was a decrease in overall size and solid components of the lesion, as expected for hemorrhage. Neuroblastoma would be expected to remain stable in size if not enlarge.
A. Incorrect. Adrenal hemorrhage does not require surgical resection. Neonatal neuroblastoma is not urgently resected either.
B. Incorrect. Ultrasound would be logistically easier and more cost effective to follow this lesion than MRI.
D. Incorrect. The findings are suggestive of hemorrhage and biopsy is not indicated.
Question 3.11: An otherwise healthy 9-year-old female undergoing renal ultrasound for urinary tract infections. Possible explanations for these findings include all but which of the following options?
Severe renal scarring and atrophy due to multiple infections (“the wasted kidney”).
Pelvic kidney.
Crossed fused ectopia.
Involuted multicystic dysplastic kidney (MCDK).
Answer:
A. Correct. Images of both renal fossae show a normal right kidney, with an empty left renal fossa other than spleen and bowel gas. No normal left renal tissue is seen. The sonographer should be directed to scan the pelvis to evaluate for pelvic kidney and closely examine the lower pole of the right kidney to look for crossed fused ectopia. If renal ectopia is not found, other explanations of an empty renal fossa include renal agenesis, involuted MCDK, or prior nephrectomy. Multiple urinary tract infections can produce renal scarring and atrophy, but not typically to the point that the kidney is no longer visualized.
B, C, D—Incorrect. This condition can produce an empty renal fossa.
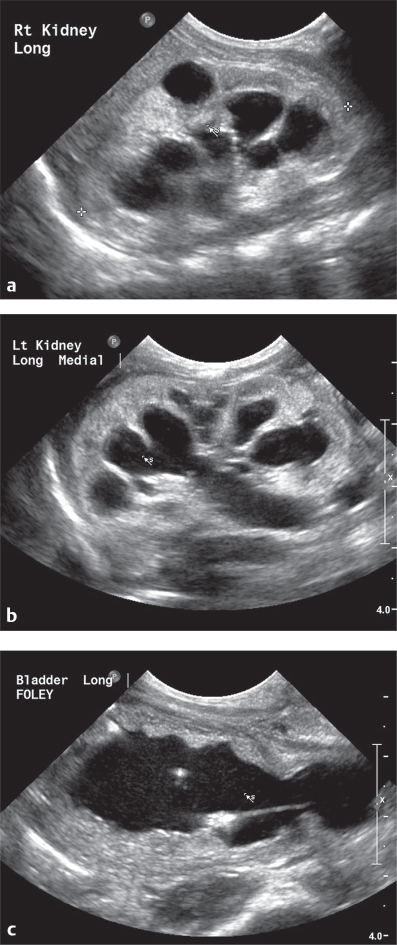
Question 3.12: Three-month-old male with hydronephrosis on prenatal ultrasound, undergoing first postnatal ultrasound. Based on the provided images, what would be the most appropriate next step in management to confirm the diagnosis?
Voiding cystourethrogram for posterior urethral valves (PUV).
Abdominal and pelvic CT for distal ureteral stone.
Referral to urology for urgent ureteral stent placement.
MAG3 scan for ureteropelvic junction obstruction (UPJO).
Answer:
D. Correct. The first image shows a markedly dilated right renal pelvis with slight calyceal dilation. The second image shows a normal smooth walled urinary bladder with no distal ureteral dilation. The combination of findings is consistent with UPJO. The cause of UPJO in children is not entirely clear, but is thought to most commonly be due to abnormal smooth muscle at the UPJ preventing normal relaxation. Another cause in some cases is due to a blood vessel crossing and compressing the UPJ. The contralateral kidney should be evaluated for associated anomalies, including duplication and MCDK. MAG3 with Lasix is the most appropriate next step in management, as the exam will confirm delayed drainage through the obstructed system.
A. Incorrect. The smooth bladder wall and lack of ureteral dilation argue against posterior urethral valves.
B. Incorrect. Obstructing renal stones are uncommon in infants and the pelvic morphology is suggestive of UPJO.
C. Incorrect. Typical surgery for UPJO is pyeloplasty rather than ureteral stent placement.
Question 3.13: Ten-year-old female with mildly elevated TSH, sent for thyroid ultrasound to exclude nodule or goiter. What next step could best confirm the diagnosis?
This is a benign colloid cyst and no further workup is needed.
Comparison ultrasound imaging of another organ.
Percutaneous ultrasound-guided fine needle aspiration (FNA), as the nodule is concerning for papillary thyroid cancer.
Neck CT with contrast for surgical planning.
Answer:
B. Correct. The initial images show an ovoid nodule in the left thyroid lobe with thin internal septations and small echogenic foci. There is no internal vascular flow, calcification, or capsule. The nodule does not have more typical spongiform appearance of a colloid nodule and there is no comet-tail artifact. Imaging of the thymus confirmed that the nodule had identical echotexture. The nodule was consistent with ectopic intrathyroidal thymic tissue. During gestation, the thymus arises from the third and fourth pharyngeal pouches and migrates caudally to its normal intrathoracic position. Ectopic thymic rests can occur anywhere along the path of descent.
A. Incorrect. The sonographic characteristics of the nodule are not suggestive of colloid cyst.
C. Incorrect. The imaging features are not suggestive of cancer, and FNA does not need to be performed to confirm ectopic thymic tissue given the appearance is identical to the thymus.
D. Incorrect. CT would not characterize this lesion better than ultrasound.
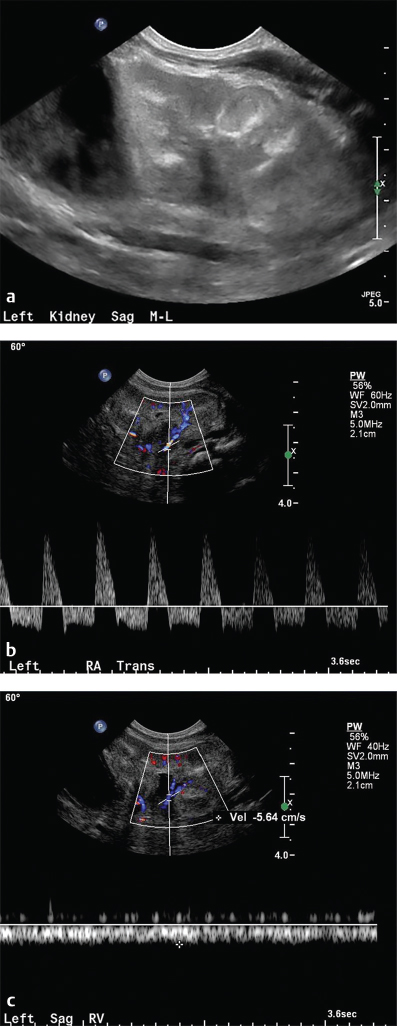
Question 3.14: Fourteen-year-old male, renal ultrasound with Doppler to evaluate hypertension refractory to two medications. A renal angiogram is also shown. Which of the following is true regarding this condition?
Grayscale images tend to show an enlarged, echogenic kidney.
A renal artery to aortic velocity ratio (RAR) over 1 is highly suggestive of the diagnosis.
A negative ultrasound excludes the diagnosis.
A potential cause in children is neurofibromatosis.
Answer:
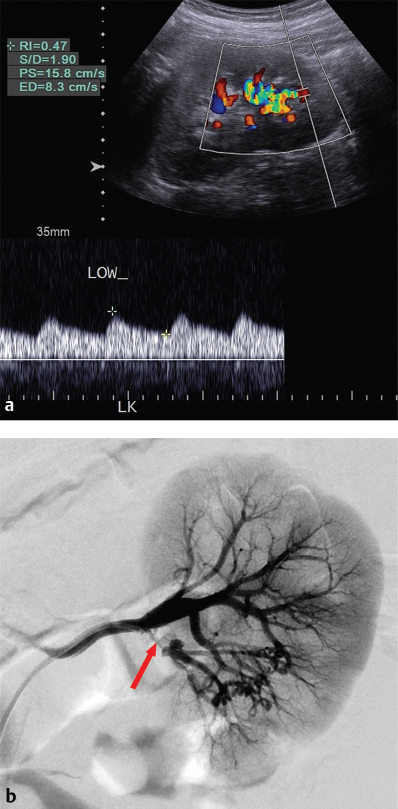
D. Correct. Multiple Doppler images of the left kidney showed normal waveforms and resistive indices within arcuate arteries in the upper and mid kidney. The waveform in the lower pole showed a prolonged systolic upstroke and a low resistive index, suggesting a proximal stenotic lesion. The patient underwent renal angiography which confirmed a segmental arterial stenosis to the lower pole (arrow) in image b. In children, fibromuscular dysplasia is the cause of renal artery stenosis in up to 70% of patients, with other etiologies including neurofibromatosis, tuberous sclerosis, and inflammatory arteritides.
A. Incorrect. Grayscale images in renal artery stenosis show an atrophic, echogenic kidney.
B. Incorrect. The RAR is considered to be abnormal at 3.5 or greater.
C. Incorrect. A normal renal ultrasound does not exclude renal artery stenosis, and further imaging with CT or MR angiography, or conventional angiography, should be performed when clinical suspicion is high.
Question 3.15: Two-month-old infant, born at 26 weeks gestation, undergoing evaluation for poor feeding and generalized hypotonia. The findings on these images are secondary to which of the following?
Prior parenchymal hemorrhage with subsequent necrosis.
In utero toxoplasmosis, other (syphilis, varicella-zoster, parvovirus B19), rubella, cytomegalovirus (CMV), and herpes (TORCH) infection.
Prior hypoxic/ischemic insult.
Postnatal cryptococcal infection (gelatinous pseudocysts).
Answer:
C. Correct. Coronal and sagittal images of the brain show multiple small cystic spaces in the periventricular white matter bilaterally, but more so on the right. Mild ventriculomegaly is present. This appearance, in conjunction with patient’s history of prematurity, is consistent with cystic periventricular leukomalacia (PVL). PVL results from an ischemic insult to a watershed zone, which in premature infants is in the periventricular white matter. Sonographic findings of PVL include abnormal increased echotexture of the white matter or frank cystic change, as in this case. PVL can be focal or diffuse, symmetric right to left, or asymmetric. Findings typically appear on ultrasounds days to weeks after the insult.
A. Incorrect. Prior parenchymal hemorrhage with necrosis would tend to form a single cystic cavity, rather than the multiple small cysts as in this case.
B. Incorrect. TORCH infections may produce periventricular and parenchymal calcifications rather than cysts.
D. Incorrect. Gelatinous pseudocysts tend to form in the basal ganglia and are seen in immunosuppressed patients.
Question 3.16: Six-month-old infant undergoing abdominal ultrasound for mildly elevated liver enzymes. How could the sonographer be directed to increase the confidence in the most likely diagnosis?
Increase the pulse repetition frequency to eliminate Doppler aliasing.
Scan the adrenal glands to evaluate for mass.
Scan the spleen to evaluate for additional lesions.
Decrease the focal zone to improve near field resolution.
Answer:
B. Correct. The images show multiple hypoechoic lesions throughout the liver with internal vascular flow. The main differential for these lesions in an infant is multiple infantile hepatic hemangiomas and metastatic disease, most commonly from neuroblastoma. The sonographer could be directed to scan the adrenal glands to evaluate for mass; if none is seen, this increases the confidence in the diagnosis of hemangiomas. Infantile hepatic hemangiomas can be single or multiple, and are most commonly treated with watchful waiting as they spontaneously involute. Symptomatic hemangiomas can result in high output heart failure or consumptive coagulopathy (Kasabach–Merritt syndrome), and may be treated with medications, embolization, or liver transplantation in extreme cases.
A. Incorrect. No significant aliasing is seen on the Doppler image, and the focal zone appears appropriate on this image.
C. Incorrect. Additional hypoechoic splenic lesions might be seen if abscesses are suspected in an immunosuppressed patient, however abscesses should not have internal blood flow.
D. Incorrect. No significant aliasing is seen on the Doppler image, and the focal zone appears appropriate on this image.
Question 3.17: Two different operators made the same mistake in two different pyloric ultrasounds. What was it?
Wrong focal zone setting.
Wrong measurement of pyloric wall thickness.
Imaging with the stomach too full.
Wrong body part.
Answer:
D. Correct. Both operators mistakenly imaged the gastroesophageal junction thinking it was the pylorus. The appearance can be quite similar to the pylorus, since there are layers of echogenic mucosa and hypoechoic muscularis which are closely apposed to each other. The key to avoiding this mistake is to identify landmarks which are not normally present when the pylorus is correctly imaged, such as the heart and the diaphragm.
A, B, C—Incorrect. These options were not the specific mistake.
Question 3.18: Six-week-old male with palpable right neck mass. Based on the provided images, what is the most appropriate neck step in management?
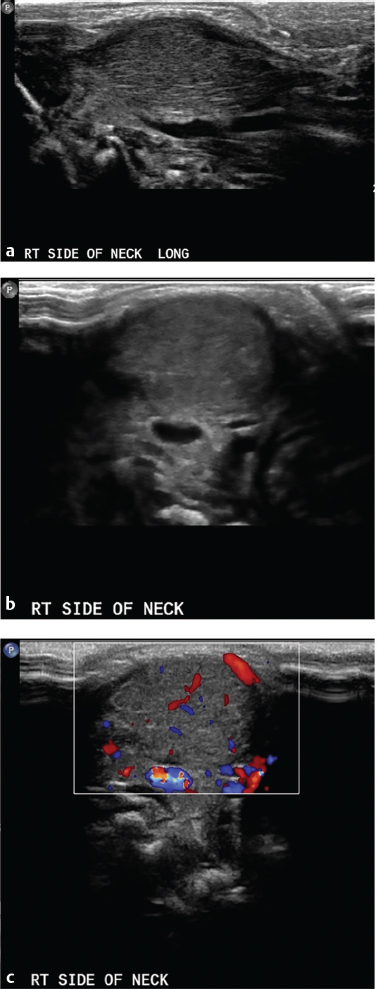
Image the contralateral neck for comparison.
CT neck with contrast to evaluate for metastatic adenopathy and for surgical planning.
MRI neck to avoid radiation in this young infant.
The mass should be biopsied by FNA prior to any additional imaging.
Answer:
A. Correct. Longitudinal and transverse images of the right neck show an ovoid, hypervascular mass. Careful inspection of the images reveals that the mass is actually fusiform enlargement of the sternocleidomastoid (SCM) muscle, as muscle fibers can be seen, especially on the longitudinal image. This is consistent with fibromatosis colli, a benign and typically self-limited proliferation of fibrous tissue within the SCM that is the most common cause of neonatal torticollis. The key to recognizing fibromatosis colli are to appreciate that the muscle itself is enlarged, and comparison imaging of the contralateral SCM showing normal muscle can help to confirm the diagnosis.
B. Incorrect. Additional imaging with CT is not indicated when the sonographic features are consistent with fibromatosis colli. If the mass did not have the typical appearance or was more aggressive, cross-sectional imaging could be indicated.
C. Incorrect. Additional imaging with MRI is not indicated when the sonographic features are consistent with fibromatosis colli. If the mass did not have the typical appearance or was more aggressive, cross-sectional imaging could be indicated.
D. Incorrect. An invasive procedure such as biopsy is certainly not indicated in this benign condition.
Question 3.19: Seven-day-old late preterm infant in NICU for mild respiratory distress, noted to have hematuria and decreasing platelet counts. In neonates, which of the following is not a potential cause of this condition?
Dehydration.
Sepsis/infection.
Maternal diabetes.
Vesicoureteral reflux.
Answer:
D. Correct. The images show an echogenic left kidney with poor corticomedullary differentiation and linear echogenic structures. The Doppler images show reversal of diastolic blood flow in the main renal artery and a dampened, monophasic waveform in the main renal vein. The imaging findings and clinical symptoms are consistent with renal vein thrombosis (RVT), albeit, non-occlusive since some dampened flow is detected with the renal vein. Causes of RVT in neonates include dehydration or hypotension from any source, including sepsis and congenital heart disease, and maternal diabetes, among others. Central lines such as peripherally inserted central catheters within the inferior vena cava can also serve as a nidus for thrombosis. Vesicoureteral reflux is not a cause of RVT.
A, B, C—Incorrect. These are known causes of RVT.
Question 3.20: Three-week-old male undergoing workup for hydronephrosis on prenatal ultrasound. What is the most appropriate next step?
MAG3 scan with Lasix.
Voiding cystourethrography (VCUG).
MR urography.
Percutaneous nephrostomy.
Answer:
B. Correct. The images show bilateral hydronephrosis, and a small volume, thick walled and irregular bladder. In a male, these findings are highly suggestive of posterior urethral valves (PUV). In fact, the finding of bilateral hydronephrosis in a male patient should prompt workup for valves. The image of the bladder shows the classic “keyhole” sign made by the bladder, bladder neck, and dilated posterior urethra. VCUG is the most appropriate next step to confirm the diagnosis, and will demonstrate a dilated posterior urethra with abrupt caliber change at the level of the valves to a small caliber anterior urethra.
A. Incorrect. MAG3 scans with Lasix are more suitable for evaluating unilateral obstructions such as ureteropelvic or ureterovesicular junction obstructions.
C. Incorrect. Quicker, easier, and less expensive test for PUV is VCUG.
D. Incorrect. Percutaneous nephrostomy will do nothing to alleviate the urethral obstruction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree