Chapter 5 Hepatobiliary
Rashmi Nair and Adrian Dawkins
5 Questions and Answers
Question 5.1: What structure is indicated by the arrow ?
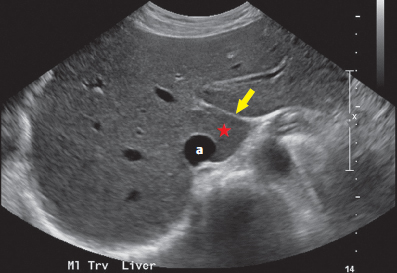
Falciform ligament.
Interlobar fissure.
Ligamentum venosum.
Gastrohepatic ligament.
Answer:
C. Correct. The arrow indicates the fissure for the ligamentum venosum. The caudate lobe is noted in close relation (star) abutting the inferior vena cava (IVC; a).
A. Incorrect. The falciform ligament runs in the plane between the medial and lateral segments of the left lobe of the liver. It is not imaged in this case.
B. Incorrect. The interlobar fissure runs in the plane between the right and left lobes of the liver. It is not imaged in this case.
D. Incorrect. The gastrohepatic ligament is not imaged. It forms part of the lesser omentum and connects the liver to the lesser curve of the stomach.
Question 5.2: What structure is indicated by the arrow ?

Gastroesophageal junction.
Cisterna chyli.
Aorta.
Lymph node.
Answer:
A. Correct. The gastroesophageal junction is often visualized on ultrasound imaging of the liver and is frequently confused with other structures. In the axial plane, it may be seen as a rounded structure to the left of the IVC (labeled a). If in doubt, the structure may be reviewed on a cine clip, allowing visualization of continuity above and below the diaphragm.
B. Incorrect. The cisterna chyli is a retrocrural structure related posteriorly and to the right of the aorta.
C. Incorrect. The aorta is not clearly imaged.
D. Incorrect. This does not have the typical reniform appearance of a lymph node.
Question 5.3: What structure is indicated by the arrow ?

Left hepatic vein.
Recanalized paraumbilical vein.
Left branch of the portal vein.
Left gastric vein.
Answer:
A. Correct. The arrow indicates the left hepatic vein. The middle and right hepatic veins are also imaged, all three draining into the IVC (star). The classic appearance has been described as the “bunny sign.”
B, C, D—Incorrect. These vessels are not imaged.
Question 5.4: What is the next appropriate step in imaging?

Perform the Valsalva maneuver.
Obtain spectral Doppler.
Proceed to computed tomography (CT) with intravenous contrast.
Proceed to magnetic resonance cholangiopancreatography with intravenous contrast.
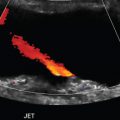
Answer:
B. Correct. The image demonstrates a polypoid solid soft-tissue lesion arising within the gallbladder lumen. The color Doppler overlay demonstrates a tiny focus of color signal within the polyp. Because of the small size, this punctate focus should be reinterrogated with spectral Doppler to confirm authentic vascular flow as opposed to artifact.
A. Incorrect. The Valsalva maneuver would not be helpful.
C. Incorrect. While further cross-sectional imaging may provide useful information regarding local anatomy and distant disease, this is not the next appropriate step.
D. Incorrect. This option is not the next appropriate step due to the above mentioned reason.
Question 5.5: Polypoid gallbladder lesions greater than what dimension should be follow-up with repeat ultrasound?
1 mm.
4 mm.
6 mm.
10 mm.
Answer:
C. Correct. Gallbladder polyps are commonly encountered incidentally in daily practice. The vast majority of these polyps are benign and indeed nonneoplastic. At a size >6 mm, there is a slightly increased risk of an underlying adenoma which theoretically could progress to an adenocarcinoma. Consequently, polyps that are >6 mm in size warrant follow-up, where as those, ≤6 mm require no follow-up imaging.
A, B—Incorrect. Polyps >6 mm should be followed-up.
D. Incorrect. Some authors advocate for cholecystectomy for polyps exceeding 10 mm but this is debatable.
Question 5.6: The sonographic image below demonstrates a gallbladder mass in a patient with a known primary malignancy. What is the most common source of gallbladder metastases?

Gastric carcinoma.
Melanoma.
Renal cell carcinoma.
Hepatocellular carcinoma.
Answer:
B. Correct. Melanoma is reported to represent 60% of all gallbladder metastases in the western medical literature.
A. Incorrect. Although gastric carcinoma is a common source of gallbladder metastases in Asia, melanoma is a more common source in the west.
C. Incorrect. This is not the most common source of gallbladder metastases.
D. Incorrect. Hepatocellular carcinoma may directly invade the gallbladder, but is less likely to result in a true metastatic deposit.
Question 5.7: What is the likely diagnosis of the finding indicated by the arrow ?

Hemangioma.
Hepatocellular carcinoma.
Focal nodular hyperplasia.
Myelolipoma.
Answer:
D. Correct. The image demonstrates a soft-tissue lesion in close relation to the right lobe of the liver. The lesion demonstrates echogenic (fatty) areas and is external to the liver parenchyma. The location and imaging features are consistent with an adrenal myelolipoma.
A, B, C—Incorrect. These options represents an intrahepatic lesion. The imaged lesion is extrahepatic.
Question 5.8: A 46-year-old male with a history of intravenous drug and alcohol abuse is admitted to the ICU with altered mental status. A sonographic image of his liver is presented below. Which of the following is the most helpful finding for the diagnosis of cirrhosis?

Diffusely increased liver echogenicity.
Heterogeneous liver parenchyma.
Liver surface nodularity.
Perihepatic fluid.
Answer:
C. Correct. Liver surface nodularity reflects the presence of regenerative nodules and fibrosis. This morphological feature is the most predictive indicator for the diagnosis of cirrhosis using conventional gray-scale ultrasound (US).
A. Incorrect. There are many pathologies that result in diffusely increased hepatic echogenicity and thus, this finding is not specific for cirrhosis. The common differential diagnoses include steatosis, cirrhosis, hepatitis, and chronic right heart failure. Diffusely increased liver echogenicity correlates more with hepatic fat content than fibrosis in cirrhosis.
B. Incorrect. There are several causes for liver parenchymal heterogeneity such as cirrhosis, infiltrating hepatocellular carcinoma (HCC), heterogeneous fatty deposition, and florid metastatic liver disease.
D. Incorrect. Perihepatic fluid is a nonspecific finding and may also be encountered in a variety of renal and cardiac diseases.
Question 5.9: The following US examination was performed on a 52-year-old male with chronic viral hepatitis. Which value should be reported?

2.15 m/s.
0.64 m/s.
1.97 m/s.
3.57 m/s.
Answer:
C. Correct. The patient is undergoing point shear wave elastography (pSWE). pSWE provides a measure of parenchymal elasticity which is used to predict the severity of hepatic fibrosis. Imaging is obtained via an intercostal approach, in a fasting patient lying supine or in the left lateral decubitus position. Ten acquisitions are obtained from the same general area avoiding large vessels and focal lesions. The median of these 10 measurements is to be reported. The obtained value correlates with the METAVIR liver biopsy score.
A. Incorrect. This value is the mean which is not the recommended value to be reported.
B. Incorrect. This is the standard deviation of the measurements and hence incorrect.
D. Incorrect. The highest obtained value is not the recommended value to be reported.
Question 5.10: What breathing instructions should patients be given during the acquisition of liver parenchymal elastography measurements?
Continue breathing gently during acquisition.
Take a deep breath and hold for acquisition.
Hold your breath for acquisition between episodes of quiet breathing.
Exhale forcefully, then hold for acquisition.
Answer:
C. Correct. A breath hold in between episodes of quiet breathing avoids wide fluctuations in hepatic venous pressure which may be encountered during deep inspiration or expiration. This in turn could influence the observed liver stiffness.
A, B, D—Incorrect. These choices could lead to erroneous measurements.
Question 5.11: All the following are indications for liver elastography except?
Chronic hepatitis C infection.
Nonalcoholic fatty liver disease (NAFLD).
Unexplained portal hypertension.
Acute hepatitis.
Answer:
D. Correct. Elastography plays no role in the workup of acute hepatitis.
A. Incorrect. Chronic hepatitis C infection is an established indication for US elastography to assess the degree of fibrosis prior to the initiation of therapy and also for subsequent monitoring of the response to therapy.
B. Incorrect. Elastography is indicated for assessing the presence of fibrosis and assessing the risk of progression to cirrhosis in NAFLD.
C. Incorrect. Elastography is indicated in the workup of unexplained portal hypertension to diagnose the presence of underlying cirrhosis.
Question 5.12: Two sonographic images are obtained in a patient with abdominal pain. What likely accounts for the echogenic lesion within the liver parenchyma?

Hemangioma.
Hepatocellular carcinoma (HCC).
Focal nodular hyperplasia.
Hepatic adenoma with hemorrhage.
Answer:
B. Correct. The images demonstrate a somewhat ill-defined echogenic lesion (arrowhead) within a somewhat heterogenous liver. Also, the adjacent image demonstrates a transjugular intrahepatic portosystemic shunt (TIPSS). These findings indicate the underlying diagnosis of cirrhosis and an associated HCC. HCC can manifest in protean ways sonographically. Any large solid mass in a cirrhotic liver is HCC until proven otherwise.
A. Incorrect. While hemangiomas are typically echogenic, hemangiomas of this size are uncommon in the cirrhotic liver, presumably “consumed” by the cirrhotic process. The interpreting radiologist is duty bound to exclude HCC when these imaging appearances arise.
C. Incorrect. Focal nodular hyperplasia is a benign lesion of the liver, frequently possessing a central scar. It demonstrates a variable appearance on ultrasound and theoretically could account for the given appearance. However, an HCC is the much more likely choice.
D. Incorrect. Hepatic adenomas may be echogenic on ultrasound due to lipid content and associated hemorrhage. However, this is a much less likely choice, based on the given appearance.
Question 5.13: A 53-year-old male with hepatitis C, cirrhosis, and ascites presents for US. The following representative image was acquired. What is the diagnosis?

Cholangiocarcinoma.
Infiltrating HCC.
Metastases.
Regenerative nodule.
Answer:
B. Correct. The image demonstrates an expanded portal vein with isoechoic thrombus (arrowhead) contiguous with and similar in echotexture to the visualized abnormal liver. The findings are consistent with infiltrating HCC and associated “tumor thrombus.” Doppler imaging may assist in demonstrating vascular flow within the thrombus, distinguishing it from bland thrombus which is commonly encountered in portal hypertension. Infiltrative HCCs account for 7 to 20% of HCCs and are seen almost exclusively in patients with established cirrhosis. This type of HCC can be very difficult to detect on imaging, especially with ultrasound. This pattern is important to recognize since ultrasound remains the primary modality for HCC surveillance.
A. Incorrect. Cholangiocarcinoma usually manifests sonographically as biliary dilation. A discrete mass is often difficult to detect.
C. Incorrect. Metastases typically tend to present as multiple lesions. It is uncommon for metastatic disease to present as an ill-defined mass with tumor thrombus.
D. Incorrect. Regenerative nodules are nonneoplastic and typically less than 2 cm.
Question 5.14: According to the American Association for Study of Liver Diseases (AASLD) guidelines, how often should patients at high risk for HCC be screened sonographically?
Every 3 months.
Every 6 months.
Annually.
Every 2 years.
Answer:
B. Correct. Patient at high risk for HCC should be screened every 6 months with US.
A, C, D—Incorrect. Screening should occur every 6 months.
Question 5.15: A 48-year-old female presents with pain and indigestion. She undergoes an US of her abdomen, representative images from which are demonstrated below. Of the options, which management strategy is most appropriate?

No follow-up required.
Follow-up with ultrasound in 6 months.
Cholecystectomy.
Hepatobiliary iminodiacetic acid (HIDA) scan.
Answer:
C. Correct. The images demonstrate a curvilinear echogenic focus arising from the wall of gallbladder with posterior acoustic shadowing. Indeed, a normal gallbladder wall is not perceived. These features are consistent with “porcelain gallbladder.” While somewhat controversial, the 2 to 3% risk of gallbladder carcinoma in the setting of porcelain gallbladder usually prompts prophylactic cholecystectomy.
A, B—Incorrect. Prophylactic cholecystectomy is the most appropriate management strategy.
D. Incorrect. A HIDA scan would be inappropriate.
Question 5.16: The patient imaged below presents with abdominal pain. What is the likely underlying diagnosis?

Porcelain gallbladder.
Emphysematous cholecystitis.
Cholelithiasis.
Pneumobilia and gallbladder luminal gas.
Answer:
C. Correct. The images demonstrate the classic wall–echo–shadow complex (WES sign). The sign is created by the gallbladder wall separated from the echo of calculi by intervening bile. The shadow is of course created by the calculi. Recognizing this sign is important as it may be mimicked by other entities such as loops of bowel or porcelain gallbladder.
A. Incorrect. Porcelain gallbladder represents calcification of the actual wall of the gallbladder.
B. Incorrect. Emphysematous cholecystitis is characterized by gas within the wall of the gallbladder.
D. Incorrect. Gas within the lumen of the gallbladder would result in the classic “dirty shadowing” appearance.
Question 5.17: A 62-year-old woman presents with right upper quadrant (RUQ) abdominal pain. A RUQ US is performed. What is the most likely diagnosis?

Inflammatory polyps.
Adenomyomatosis.
Cholesterol polyps.
Gallbladder carcinoma.
Answer:
C. Correct. A cholesterol polyp is the most common polypoid lesion encountered within the gallbladder accounting for 60 to 70% of lesions in some studies. As in this image, they appear as well-defined, round, echogenic intraluminal lesions attached to the gallbladder wall (“ball on a wall”). These lesions are situated within the wall of the gallbladder.
A. Incorrect. Inflammatory polyps typically occur in the setting of gallstones and chronic inflammation. They are typically multiple and <10 mm in size. Imaging features are nonspecific.
B. Incorrect. Adenomyomatosis typically presents as a focus of “comet tail” artifact arising from the gallbladder fundus. It represents cholesterol crystals with tiny intraluminal spaces (Rokitansky–Aschoff sinuses).
D. Incorrect. Gallbladder carcinoma is unlikely given the very small size and multitude of the lesions in this case.
Question 5.18: An ultrasound of the abdomen was performed in a 4-day-old neonate with vomiting and diarrhea. What is the most likely diagnosis in this child?

Necrotizing enterocolitis.
Portal vein thrombosis.
Budd–Chiari syndrome.
Acute hepatitis.
Answer:
A. Correct. The green arrow demonstrates echogenic foci with the portal vein, consistent with gas. This results in the bidirectional spikes seen on the Doppler spectral trace (yellow arrow). Portal venous gas is a key finding in necrotizing enterocolitis.
B. Incorrect. Flow is clearly demonstrated within the portal vein on color and spectral Doppler.
C. Incorrect. There are no presented findings in this case to support the diagnosis of Budd–Chiari syndrome, such as hypertrophy of the caudate lobe or occlusion of the hepatic veins.
D. Incorrect. There are no presented findings in this case to support the diagnosis of acute hepatitis, such as a swollen hypoechoic liver with echogenic portal triads (starry-sky pattern).
Question 5.19: A 54-year-old female with acute kidney injury undergoes a renal ultrasound. An incidental liver lesion is observed. What is the most likely diagnosis?

Abscess.
Focal nodular hyperplasia.
Hemangioma.
Metastasis.
Answer:
D. Correct. The sonographic image demonstrates a large isoechoic liver lesion with a surrounding hypoechoic rim. This represents the classic “halo sign” a frequently encountered feature of liver metastasis.
A. Incorrect. An abscess would present as a well-defined complex fluid collection possibly containing foci of gas and demonstrating peripheral hyperemia.
B. Incorrect. The halo sign is not typically associated with focal nodular hyperplasia.
C. Incorrect. Hemangiomas are typically hyperechoic with respect to normal liver parenchyma. Hemangiomas are not typically associated with the halo sign.
Question 5.20: The sonographic image below is obtained in a 64-year-old patient with abdominal pain. What other clinical sign or symptom is likely present?

Absent or diminished bowel sound.
Jaundice.
Easy bruising.
Abdominal bruit on auscultation.
Answer:
B. Correct. This transverse view of the upper abdomen reveals a punctate echogenic finding with posterior shadowing within the vicinity of the pancreatic head (arrow). This represents a calculus within the distal common bile duct.
A, C—Incorrect. These symptoms are not typically related to the finding.
D. Incorrect. An abdominal bruit may be encountered in the setting of an abdominal aortic aneurysm, however the imaged aorta (a) is of normal caliber.
Question 5.21: A 44-year-old female with abnormal liver enzymes presents for routine RUQ ultrasound. A lesion is detected within the liver (arrow). Which statement is correct?

No further workup required as this finding likely represents fatty sparing in the setting of steatosis.
A targeted biopsy should be performed since malignancy is highly likely, given the appearances.
This lesion is unlikely to be a hemangioma given its hypoechoic appearance.
None of the above.
Answer:
D. Correct. Hemangiomas are typically well-defined and hyperechoic with respect to normal liver parenchyma on sonographic evaluation. However, in the setting of background hepatic steatosis, a hemangioma is frequently noted to be relatively hypoechoic.
A. Incorrect. Further imaging is required to help provide definitive characterization. Focal fatty sparing may present as hypoechoic areas within an otherwise echogenic liver, typically along the gallbladder fossa. However, the rounded appearance of this lesion as well as the location make focal fatty sparing less likely.
B. Incorrect. Definitive characterization should be attempted with magnetic resonance imaging (MRI) or CT with intravenous contrast prior to an invasive biopsy. This lesion was confirmed to be a hemangioma with MRI.
C. Incorrect. This option is not correct because of the reason mentioned above.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree