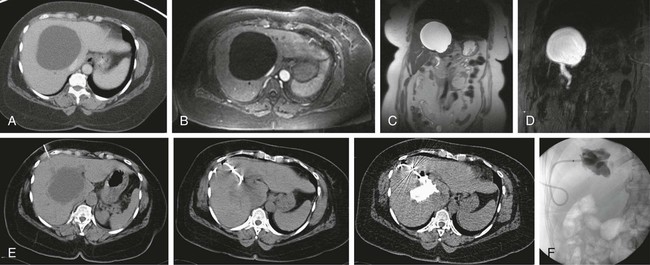
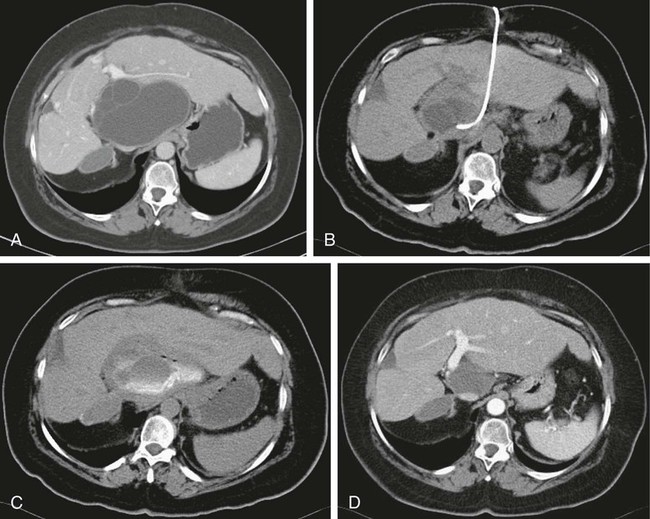
Chapter 144 Joshua L. Weintraub, Thomas J. Ward and John H. Rundback Liver cysts are common, with a prevalence of approximately 2.5% in the general population and a female predominance.1 A majority of these cysts are incidentally discovered by ultrasound or computed tomography (CT) and are clinically insignificant, so no further evaluation or treatment is necessary. For a minority of patients, larger cysts can produce symptoms that range from abdominal discomfort and nausea to compression of the biliary tree or inferior vena cava, intraperitoneal rupture, hemorrhage, torsion, or infection.2–6 The majority of symptomatic cysts occur in females older than 50, with a 9 : 1 female-to-male ratio and a predisposition for the right hepatic lobe.7 Previous attempts at percutaneous treatment of the symptomatic cyst focused on cyst aspiration. This strategy produced suboptimal results due to high rates of cyst recurrence, with reported recurrence rates between 78% and 100%.8,9 Advances in percutaneous treatment of liver cysts occurred with the introduction of ablative agents that treat the underlying pathology of the process. True simple hepatic cysts have an epithelial lining and are the result of congenitally aberrant bile ducts that are separated from the remainder of the intrahepatic biliary tract. The columnar or cuboidal epithelial cells that line the cyst produce fluid that reaccumulates after simple aspiration. With newer techniques, after cyst aspiration a variety of chemical agents (e.g., tetracycline hydrochloride, doxycycline, minocycline hydrochloride, hypertonic saline) have been injected into the cyst in an attempt to decrease previously observed recurrence rates by damaging the fluid-producing cells.10–13 The most studied chemical agent administered for this purpose is ethanol, which produces epithelial cell damage that prevents fluid secretion and results in subsequent cyst destruction. Percutaneous ethanol sclerotherapy (PES) is indicated in the setting of a hepatic cyst that produces clinically significant mass effect on adjacent structures, such as biliary obstruction or compression of the inferior vena cava, abdominal pain, or other significant symptomatology that affects the patient’s quality of life (Fig. e144-1). In the setting of abdominal pain, care must be taken to exclude other etiologies for the patient’s symptoms before proceeding with intervention, since approximately 85% of cysts are asymptomatic.2,14 Furthermore, the lesion to be treated must be definitively identified as a simple cyst and not a cystadenoma, cystadenocarcinoma, or other malignancy. In the setting of an indeterminate lesion or hemorrhage into a simple cyst, definitive identification with magnetic resonance imaging (MRI) can generally be obtained. If there is uncertainty that a discovered cyst is the cause of the patient’s pain, a trial of simple aspiration can be performed, with ethanol sclerosis performed in the setting of symptomatic cyst recurrence. Contraindications specific to hepatic cyst aspiration with PES include a cyst that communicates with the peritoneal cavity or biliary system, because irreversible sclerosing cholangitis has been reported. Irreversible coagulopathy is also a contraindication, with an international normalized ratio (INR) of less than 1.5 and an absolute platelet count greater than 50,000 shown to decrease complication rates.15 The equipment necessary to perform hepatic cyst PES includes an ultrasound machine with a 3- to 5-MHz curved-array transducer, an 18-gauge needle, a 0.035 Amplatz wire, appropriate fascial dilators and a 6F to 12F multipurpose drainage catheter. The procedure is performed with mild sedation in a fluoroscopy suite or on a CT scanner so communication between the cyst and the biliary system or peritoneum can be evaluated with administration of water-soluble contrast. Various ethanol concentrations have been used at different institutions, with concentrations ranging from 95% to 99%.16,17 At our institution, a sterile solution of 98% ethanol by volume is administered. Other required equipment includes a sterile tray and sheets. PES is performed with real-time ultrasound guidance, at which time the location, depth, and angle for the puncture site is determined. The procedure itself has not significantly changed since Bean and Rodan’s paper in the American Journal of Radiology 25 years ago.17 The procedure is performed with mild sedation and sterile technique, with prophylactic antibiotics generally not administered. Local 1% lidocaine is administered at the determined puncture site prior to gaining access to the cyst via an 18-gauge needle. Access to and characterization of the cyst is confirmed with fluid aspiration. The first 20 mL of fluid is sent for laboratory evaluation to exclude malignancy or infection. A 0.035-inch Amplatz wire is placed through the needle into the cyst, with the needle then withdrawn. The Seldinger technique is used to advance a 6F to 12F multipurpose drainage catheter with side holes into the cyst after appropriate fascial dilatation. All fluid is then aspirated from the cyst, with complete drainage confirmed via ultrasound examination. The evacuated cyst cavity is then injected with dilute water-soluble contrast and fluoroscopy, or a CT scan is performed to evaluate for a communication between the cyst and the biliary tree or peritoneal cavity. The contrast material is then removed prior to instillation of sterile ethanol. The volume of ethanol instilled is generally selected to be between 25% and 40% of the volume of cyst fluid aspirated. The drainage catheter is then capped, and the ethanol is left in place for 20 to 30 minutes, with the patient rolled into various positions to ensure treatment of all surfaces of the cyst cavity. The ethanol is then aspirated, with the volume removed generally found to be greater than the volume injected because of the release of loculated pockets of fluid or dead cells. This procedure may be repeated in the setting of large cysts (generally > 400 mL). The catheter is then removed and the skin bandaged. A study that compared single-session ethanol sclerotherapy to prolonged catheter drainage with negative pressure demonstrated similar results between the two methods, with statistically insignificant differences in regard to average cyst volume reduction, final cyst volume, or cyst disappearance rates.18 A variety of options are available for surgical management. Prior to widespread use of laparoscopic surgeries, open cystectomy, hepatic wedge resections, and lobectomies were performed, with significant rates of morbidity and mortality. In comparison, laparoscopic “de-roofing” has significantly lowered adverse events, cost, and length of stay, with low rates of recurrence.19–21 No prospective randomized control studies have been performed that compare percutaneous to laparoscopic treatment. As such, the expertise of the physicians at the performing institution generally guides treatment decisions. PES is effective at reducing cyst volume and relieving the symptoms for which the procedure is performed. A review of the literature performed by Drenth et al. of 34 articles that involved 292 patients with solitary or multiple hepatic cysts demonstrated an at-least-partial recurrence rate of 21% during follow-up, with the majority being asymptomatic and reintervention rarely performed.22 The largest study examined cyst size reduction and symptom relief in 25 patients with 59 symptomatic hepatic cysts, with 11 patients having a single cyst. Overall, 8 cysts resolved completely, and mean diameter of remaining cysts decreased from 9 to 3 cm. Symptoms completely resolved or improved in all patients with solitary cysts; symptoms recurred in 7 patients with polycystic liver disease, owing to growth of other untreated cysts.23 If tolerated without immediate complication, PES can be performed as an outpatient procedure. Short-term follow-up at 1 to 2 months with ultrasound is generally performed, with further follow-up performed only for symptom recurrence. A small sample of 39 benign intraabdominal cysts, 21 hepatic, that were treated with PES followed by frequent ultrasound during the first year demonstrated that of those cysts that recurred, all recurred at a smaller volume and subsequently decreased spontaneously in size without intervention. The authors concluded that initial recurrence after percutaneous ablation is usually a transient reactive inflammatory reaction and not true treatment failure.24 Should symptoms recur in the setting of cyst recurrence, repeat PES or laparoscopic de-roofing may be considered. Cystic echinococcosis (CE) is a zoonotic infection of the Echinococcus tapeworm, with Echinococcus granulosus and Echinococcus multilocularis being the species that most commonly cause human disease. In endemic areas and Middle Eastern, South American, and Mediterranean countries, the annual incidence of CE ranges from 1 to 200 per 100,000, with a mortality rate of 2% to 4% and higher mortality rates seen in the setting of inadequate medical care.25 CE can affect multiple organ systems, although 80% of patients present with a solitary cyst, most commonly hepatic.26 Disease presentation and progression is markedly variable. Cysts may remain stable for years, regress or resolve spontaneously, or grow rapidly with symptom onset generally secondary to mass effect on adjacent structures, although intraperitoneal rupture and subsequent anaphylaxis can occur. Traditionally, surgical management has been the standard of care for treating active or symptomatic CE because of the fear that percutaneous treatment could result in spillage of cyst contents and peritoneal seeding or a fatal anaphylactic reaction. Use of the anthelmintic chemotherapy drugs mebendazole and albendazole prior to percutaneous intervention decreases this risk and has resulted in increased use of percutaneous treatment strategies at many high-volume centers (Fig. e144-2).27 The appropriateness for a puncture, aspiration, injection, and reaspiration (PAIR) treatment strategy depends on the complexity and activity of the cyst being treated. In 1996, the World Health Organization Informal Working Group on Echinococcosis (WHO-IWGE) produced a standardized classification system to replace the previous classification schemes.28 The most popular scheme at the time was proposed by Gharbi et al. in 1981 and is still regularly referenced.29 PAIR is first-line treatment for WHO-IWGE CE1 and CE3a cysts (Gharbi types 1 and 2).30 These cysts contain clear fluid; a detached membrane and daughter cysts may or may not be present. It is also indicated for patients who are not surgical candidates, patients who refuse surgery, and for cases that failed surgery or medical management. PAIR of CE is performed with real-time ultrasound or CT guidance after the diagnosis of CE is confirmed with an indirect hemagglutination test (IHA), or enzyme-linked immunosorbent assay (ELISA) confirms the presence of antibodies against Echinococcosis, and ultrasound or CT has identified a characteristic cyst. Albendazole or mebendazole is administered at least 4 hours before the procedure and continued for 1 month after.31 In the case of large cysts (>10 cm in diameter), a PAIR procedure may be performed with drainage (PAIR-D). Following a traditional PAIR procedure, a 0.035-inch Amplatz wire is placed through the needle into the cyst, with the needle then withdrawn. The Seldinger technique is used to advance an 8F multipurpose drainage catheter with side holes into the cyst, with care taken to only dilate the tract through the subcutaneous tissues and most superficial liver to reduce the risk of cyst content spillage. The drainage catheter is left to drainage and irrigated with isotonic fluid 4 or 5 times daily until drain output is less than 10 mL/day.32 Controversy initially surrounded the safety of percutaneous treatment of CE with PAIR, owing to the fear that this strategy would result in increased rates of peritoneal seeding or anaphylactic reactions. For decades, CE was treated with an open surgical approach, but after the introduction of chemotherapeutic drugs to treat CE, there has been increased interest in percutaneous management. Large series have since demonstrated PAIR to be a safe and efficacious treatment strategy that is supported by long-term data when appropriate patient selection criteria are used.30,33 The optimal protoscolicidal agent is also a point of controversy. No study has demonstrated superiority of ethanol over hypertonic saline, although some believe ethanol is more sclerosing and results in quicker cyst involution.33,34 In the setting of cystobiliary communication, however, the risk of sclerosing cholangitis precludes administering ethanol. Smego et al. performed a large meta-analysis of 769 patients with CE who were treated with PAIR and albendazole or mebendazole, compared to 952 era-matched historical control subjects treated surgically. PAIR produced clinical and parasitologic cure in 95.8% of patients, compared to 89.8% in the surgical group (P < .0001).27 Rates of cyst disappearance or solidification observed with follow-up ultrasound after PAIR generally range from 80% to 100%.30,32,35 Postprocedure seroconversion rates, as determined by serial IHAs or ELISAs, range from 50% to 100% in smaller studies.30,34,36,37 A statistically significant lower rate of disease recurrence was also observed with PAIR compared to surgery: 1.6% to 6.3%, resectively.27 Patients are monitored in the hospital for adverse reaction, with 2 or 3 days being a typical hospital stay, and then continued on albendazole or mebendazole for 28 days post procedure. Follow-up imaging and blood tests are performed to assess for treatment response. Treatment cure is generally defined as disappearance of symptoms and either (1) real-time observation of endocyst separation from the pericyst or subsequent cyst solidification, (2) decreased cyst size with increased density on CT scan, or (3) seroconversion on IHA or ELISA (<1 : 160 titers).27 As such, patients are followed with ultrasound and IHA or ELISA at 1, 6, and 12 months post procedure. Ultrasound is then performed yearly thereafter to document stability.
Chemical Ablation of Liver Lesions
Chemical Ablation of Benign Liver Lesions
Simple Liver Cysts
Percutaneous Ethanol Sclerotherapy
Indications
Contraindications
Equipment
Technique
Controversies
Outcomes
Postprocedural and Follow-up Care
Puncture, Aspiration, Injection, and Reaspiration of Cystic Echinococcosis
Indications
Technique
Controversies
Outcomes
Postprocedural and Follow-up Care
Radiology Key
Fastest Radiology Insight Engine