The Normal Chest Image
Technical Considerations
Exposure
Making a properly exposed chest x-ray is much more difficult than making x-rays of other parts of the body because the chest contains tissues with a great range of contrast. The range stretches from small vessels in air-filled lungs to dense bony structures located behind the heart. A correctly exposed image should allow visualization of vessels to at least the peripheral one-third of the lung and, at the same time, allow visualization of the paraspinous margins and the left hemidiaphragm behind the heart.
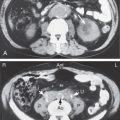
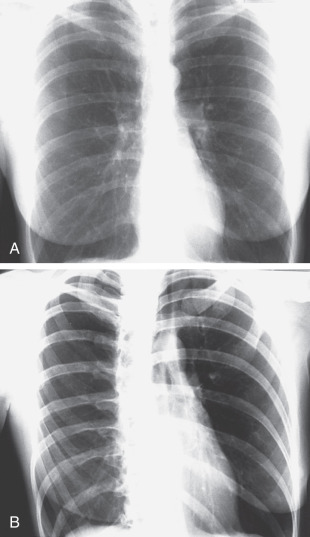
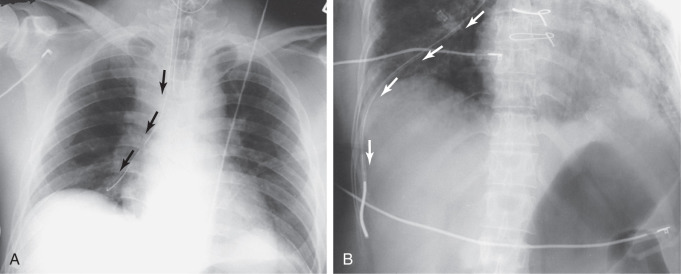
Overexposure causes the image to be dark. Under these circumstances, the thoracic spine, mediastinal structures, retrocardiac areas, and nasogastric and endotracheal tubes are well seen, but small nodules and the fine structures in the lung cannot be seen ( Fig. 3.1A ). If the image was obtained by using either digital or computed radiography, the image can be “windowed” lower on the computer, resulting in an interpretable image.
Underexposure causes the image to be quite white. This is a major problem for adequate interpretation. It will make the small pulmonary blood vessels appear prominent and may lead to thinking that there are generalized infiltrates when none are really present. Underexposure also makes it impossible to see the detail of the mediastinal, retrocardiac, or spinal anatomy (see Fig. 3.1B ). Even with digital or computed radiography, nothing can be done to an underexposed image to improve the image.
Male Versus Female Chest
The major difference between male and female chest x-rays is caused by differences in the amount of breast tissue. This is generally relevant only in interpretation of a posteroanterior (PA) or anteroposterior (AP) projection and not of the lateral projection. Breast tissue absorbs some of the x-ray beam, essentially causing underexposure of the tissues in the path. This results in the lung behind the breast appearing whiter and the pulmonary vascular pattern in the same area appearing more prominent. If the breasts are large, bilateral basilar lung infiltrates may appear to be present on the PA or AP projection.
One common problem is encountered in the woman who has had a unilateral mastectomy. In this circumstance, the lung density will be asymmetric. The lung on the side of the mastectomy will appear darker than the lung on the normal side. In this circumstance, recognition of the mastectomy will prevent you from making an erroneous diagnosis of an infiltrate or effusion based on the relatively increased density on the side with the remaining breast ( Fig. 3.2 ).

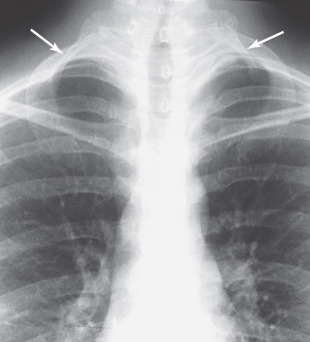
Visualization on a PA or AP chest x-ray of a single well-defined nodule in the lower lung zone should raise the suspicion that you are seeing a nipple shadow and not a real pulmonary nodule. Nipple shadows are common in both men and women. First, look at the opposite lung to see if a comparable nodule appears there. If one does, usually you can stop worrying ( Fig. 3.3 ), but before you completely stop worrying, also look at the lateral image and make sure that the nodule is not seen projecting within the lung. If only one nodule is found projecting over a lung in the PA projection and no nodule is seen on the lateral view, a small metallic BB can be taped over the nipple and the single PA view repeated to see whether it was the nipple that was being visualized.

Posteroanterior Versus Anteroposterior Chest X-Rays
Chest x-rays of ambulatory patients are usually done with the subject’s chest up against the detector plate. The x-ray tube is behind the patient, and the x-ray beam passes in from the back and exits the front of the chest. This is referred to as a PA (posterior to anterior) projection . If the patient is lying down, it is standard practice to take the image with the x-ray beam entering the front of the chest and have the detector plate behind the patient. This is called an AP (or anterior to posterior) chest x-ray .
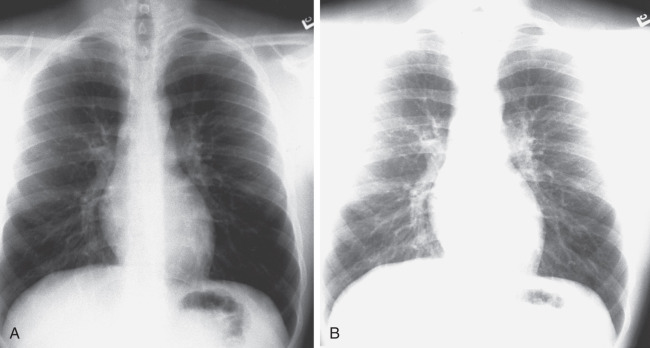
For interpretive purposes, the main difference is that the heart will be more magnified on the AP projection ( Fig. 3.4 ). This is because in the AP projection, the heart is farther from the detector plate and the x-ray beam diverges as it goes farther from the tube. Thus, the shadow of the heart appears larger on an AP chest x-ray than on a PA view. Simply remember to make sure that you are looking at a PA view before you interpret an image as showing mild or moderate cardiomegaly. Usually the technician will have written the projection on the x-ray requisition, and occasionally it may be marked on the image.
Upright Versus Supine Chest X-Rays
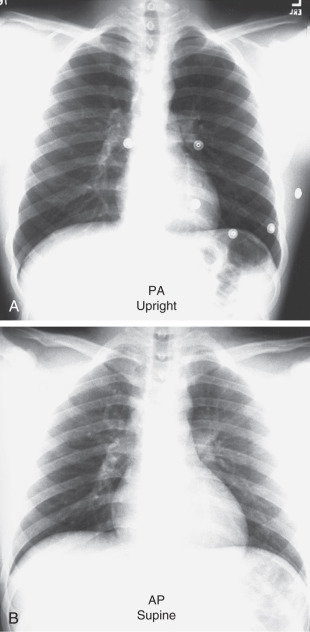
As you can imagine, patients who are able to stand or sit up usually have their chest x-rays done in that position for a number of reasons. The amount of inspiration is greater in each of these positions, spreading the pulmonary vessels and allowing clearer visualization. It is obviously easier to see a bird in a tree if the branches can be spread out instead of being squashed together. Another reason for preferring an upright examination is that small pleural effusions tend to run down into the normally sharp costophrenic angles, allowing relatively small effusions to be identified. Small pneumothoraces tend to go to the lung apex and can be relatively easy to see on an upright chest x-ray.
Now let us think about a patient lying in bed (supine). The typical chest x-ray will be done with a detector cassette under the patient. No lateral view is done. In this circumstance, the patient cannot take a full inspiration; the liver and abdominal contents push up on the lungs and heart, and the result is that the pulmonary vessels are crowded. In the supine position, the blood flow to the upper lungs essentially equals that in the lower lobes, and this will mimic congestive failure. On a supine image, the standard AP projection combined with the cephalic push of the abdominal contents will make a normal heart appear large. In addition, with the patient in a supine position, small pleural effusions will layer in the posterior pleural space, whereas small pneumothoraces will go to the anterior pleural surface, and both will easily be missed. As a result, you must be much more conservative and careful when interpreting the image of a portable supine examination.
Inspiration and Expiration Chest X-Rays
The degree of inspiration is important not only for assessing the quality and limitations of the examination but also for diagnosing different diseases. When standing, most adults can easily take an inspiration that brings the domes of the hemidiaphragms down to the level of the 10th posterior ribs. When the patient is sitting or lying down, often the level is between the eighth and tenth ribs. If the image has the domes of the diaphragms at the seventh posterior ribs, the chest should be considered hypoinflated, and you must be very careful before diagnosing basilar pneumonia or cardiomegaly ( Fig. 3.5 ). You should be cognizant of the major differences in the appearance of a chest x-ray as a result of combining all the factors mentioned earlier. Unless you are aware of these issues, you will diagnose cardiomegaly, lung infiltrates, and congestive heart failure (CHF) in a patient who is in fact normal ( Fig. 3.6 ).
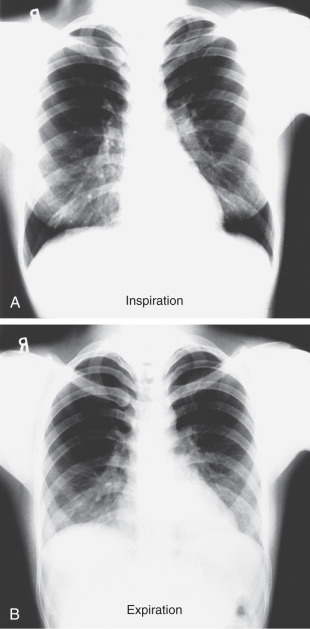

Expiration images do have occasional constructive uses. If a small pneumothorax is present, an expiration view makes the lung smaller and denser and, at the same time, makes the pneumothorax relatively larger and easier to see. Thus, if your prime interest is in identification of a small pneumothorax, order an upright expiration image. In the case of a foreign body (such as a peanut) lodged in a major bronchus, both inspiration and expiration examinations should be ordered. Either postobstructive atelectasis or a ball valve phenomenon may be seen. In the latter case, air can get in past the object during inspiration, but during expiration (as the bronchus gets smaller), air cannot get out around the object. As a result, on the expiration image, air trapping will occur in the affected lung, with a shift of the mediastinum toward the normal side.
Before hyperinflation is diagnosed on a chest x-ray, the lateral image should be examined. With hyperinflation, the diaphragms should be flattened on the lateral view. Many young adults can normally take a very deep inspiration, but on the lateral view they will not have an increased AP diameter or truly flattened hemidiaphragms. In long-standing chronic obstructive pulmonary disease (COPD), additional findings may appear, such as an increased AP diameter and an increase in the clear space between the sternum and the ascending aorta.
A typical chest x-ray is performed by using a level of energy that is a compromise for visualizing lung markings, soft tissues, and bones at the same time. Bones can be well seen by using relatively low-voltage x-rays, but then the pulmonary markings are hard to see ( Fig. 3.7 ).
Normal Anatomy and Variants
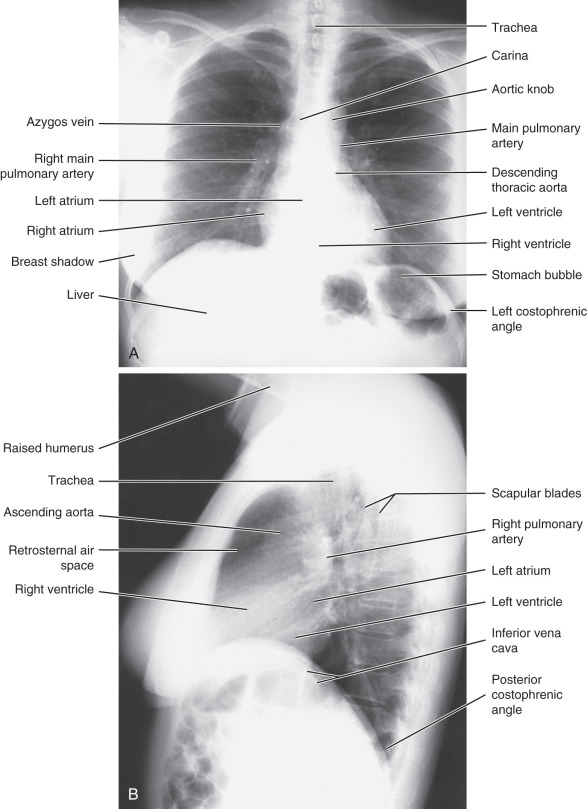
Normal anatomy as visualized on a chest x-ray is important to understand; major structures are shown in Fig. 3.8 . A method for examining a chest x-ray is given in Box 3.1 . The appropriate imaging studies to order in various clinical circumstances are shown in Table 3.1 . Some circumstances in which a chest x-ray is not indicated are shown in Box 3.2 .
Determine the age, sex, and history of the patient
Identify the projection and technique used:
AP, PA, lateral, portable, or standard distance
Identify the position of the patient:
Upright, supine, decubitus, lordotic
Look at the inspiratory effort:
Adequate, hypoinflated, hyperinflated
Identify the obvious and common abnormalities:
Heart size, large or normal
Heart shape, specific chamber enlargement
Upper mediastinal contours
Examine airway, tracheal deviation
Lung symmetry
Any mediastinal shift?
Hilar position
Lung infiltrates, masses, or nodules
Pulmonary vascularity
Increased, decreased, or normal
Lower greater than upper
Pleural effusions, blunting of costophrenic angles
Rib, clavicle, or spine fractures or other lesions
Check tube placement
Recheck what you thought was normal anatomy, and look at typical blind spots:
Behind the heart
Behind the hemidiaphragms
In the lung apices
Pneumothorax present?
Costophrenic angles
Chest wall
Lytic rib lesions
Shoulders
Look for old images, not just the last one
Decide what the findings are and their location
Give a common differential diagnosis correlated with the clinical history
AP , Anteroposterior; PA , posteroanterior.
| Clinical Problem | Imaging Study |
|---|---|
| Pneumonia | |
| Diagnosed clinically | Chest x-ray (confirmatory) |
| Immunocompromised patient with negative chest x-ray | CT without contrast |
| COPD (with acute exacerbation) | Chest x-ray |
| CHF (new or worsening) | Chest x-ray, echocardiogram |
| Blunt trauma (high-energy mechanism) | Chest x-ray, contrast chest CT (CTA if aortic injury suspected and transthoracic echocardiography if cardiac injury suspected) |
| Rib fracture (blunt trauma confined to ribs) | Chest x-ray, rib views less appropriate |
| Chest pain, acute (low probability of CAD) | Chest x-ray (additional studies depend on suspected cause) |
| Chest pain, chronic (low to intermediate probability of CAD) | Chest x-ray (possibly US or NM cardiac stress test) |
| Chest pain, chronic (high probability of CAD) | NM or US cardiac stress test or coronary angiogram |
| Shortness of breath | |
| Severe or long duration | Chest x-ray |
| Negative chest x-ray, pulmonary origin suspected | CT chest without contrast (high resolution) |
| Hypertension | |
| Uncomplicated | No imaging needed |
| Moderate or severe | Initial chest x-ray |
| Pulmonary hypertension | Initial chest x-ray, then transthoracic resting echocardiography, right heart catheterization |
| Asthma (with suspected superimposed disease or resistant to therapy) | Chest x-ray |
| Interstitial or occupational lung disease | Chest x-ray, pulmonary function studies, CT without contrast (with contrast for asbestosis) |
| Immunosuppressed patient (with fever, cough, or dyspnea) | Chest x-ray |
| Foreign body | Inspiration/expiration chest x-ray |
| Aspiration pneumonia | Chest x-ray |
| Mediastinal mass | Contrast CT |
| Solitary pulmonary nodule | See Table 3.2 and text |
| Lung tumor or lung metastasis screening | Chest x-ray and CT without contrast (extend through adrenals) |
| Pleural mass or fluid | CT |
| Localization of pleural effusion for thoracentesis | Stethoscope, US |
| Suspected pneumothorax | Chest x-ray (possibly expiration view as well) |
| Hemoptysis | Chest x-ray, CTA with contrast (if moderate or massive) |
| Pericardial effusion | Cardiac ultrasound |
| Myocardial thickness | Cardiac ultrasound |
| Cardiac wall motion | Cardiac ultrasound |
| Cardiac ejection fraction | NM (gated blood pool study) or US |
| Pulmonary embolism | Chest x-ray, and CT angiogram or NM lung scan |
| Coronary ischemia | Stress ECG, stress nuclear medicine (myocardial perfusion scan) or stress echocardiogram, coronary angiogram |
| Aortic aneurysm | CT with IV contrast or transesophageal US |
| Aortic tear | CT with IV contrast or CT angiogram |
| Aortic dissection | CT with IV contrast or transesophageal US |
| Compression upper limb neurovascular bundle (thoracic outlet syndrome) | Chest x-ray, MRA with and without contrast (if not available CTA) |
| Preoperative or admission of patient | Chest x-ray not indicated unless acute or chronic cardiopulmonary disease |
| Intensive care unit patient | Chest x-ray on admission, transfer, and clinical worsening, postinsertion catheter or tube |
Prenatal examination
Routine admission or preoperative (no cardiac or chest problem) in a patient younger than 65 years
ICU patient, no change in clinical status
Routine preemployment examination
Screening for occult lung cancer
Screening for tuberculosis
Uncomplicated asthmatic attack
Chronic obstructive pulmonary disease without acute exacerbation
Dyspnea of short duration and intensity in an adult younger than 40 years
Chest pain in an adult younger than 40 years with a normal physical examination and no history of trauma
Uncomplicated hypertension
Chronic bronchitis
Acute respiratory illness in an adult younger than 40 years with a negative physical examination and no other symptoms or risk factors
ICU , Intensive care unit.
The heart is the easiest thing to see, so we begin there. On the PA view of the heart, the left border is much more prominent than the right. It would be simple to say that the left ventricle is on the left and the right ventricle is on the right. Unfortunately, the heart chambers are somewhat twisted in the chest and, on the PA and lateral views, the cardiac chambers mostly overlie each other. As a general rule, if the right side of the heart is enlarged more than the left, a right chamber lesion is present. The same holds true for the left side.
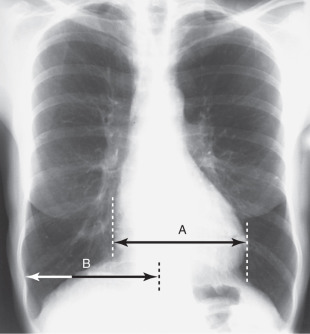
On an upright PA chest x-ray, the greatest width of the heart should be less than half the width of the thoracic cavity at its widest point ( Fig. 3.9 ). This is determined by finding the farthest right and left portions of the cardiac silhouette. These will not be at the same horizontal level, but that is all right. Find the horizontal distance between the two most lateral cardiac margins. Sometimes patients have either dextrocardia or situs inversus ( Fig. 3.10 ). Before the latter diagnosis is made, it is important to make sure that the technician did not misplace the right or left marker on the image.

The upper mediastinal structures that are visualized on the right are the brachiocephalic vessels, azygos vein, and ascending aorta. The right border of the ascending aorta can be seen beginning below the right hilum. The aortic arch is most commonly seen to the left of the trachea. The descending thoracic aorta can usually be visualized only along its left lateral border, where it abuts the left lung. The trachea should be midline and can be followed down to the carina. The right and left major bronchi are easily seen. The esophagus is not normally seen on a standard chest x-ray.
Hila and Lungs
The hila are made up of the main pulmonary arteries and major bronchi. The right hilum is usually somewhat lower than the left; it should not be at the same level or higher. The pulmonary veins usually are more difficult to see than the arteries. They converge on the atria at a level 1 to 3 inches below the pulmonary arteries. Lymph nodes are not normally seen on a chest x-ray, either in the hilar regions or in the mediastinum.
The lungs are composed mostly of air, so normally not much is seen other than blood vessels. These should be distinct and remain that way as they are traced back to the hila. If you cannot see blood vessels clearly near the hila, a perihilar infiltrate or fluid may be present (such as from CHF). Normal hila are sometimes indistinct on portable x-rays because the exposure takes longer and the vessels are blurred by motion.
The blood vessels in the lung are usually clearly seen out to within 2 to 3 cm of the chest wall. Some people say that visualization of vessels in the outer third of the lung is abnormal, but this is not true. It depends on the quality of the image and how hard you look. Lines located within 2 cm of the chest wall are abnormal and probably represent edema, fibrosis, or metastatic disease. Secondary bronchi are not normally visualized except near the hilum, where they can sometimes be seen end-on. The walls of the visualized bronchi normally should not be thicker than a fine pencil point.
A normal variant called an azygos lobe can occasionally be seen in the right upper lung. This is seen on the PA view as a fine curved line extending from the right lung apex down toward the mediastinum ( Fig. 3.11 ). It has a teardrop shape at its lower edge. This is caused embryologically by the azygos vein migrating inferiorly from the lung apex while trapping some of the lung medially.

Remember that on a PA or AP chest x-ray, the lungs go behind the heart, behind and below the dome of the hemidiaphragms, and behind and in front of mediastinal structures. Forty percent of the lung area and 25% of the lung volume will be obscured by these other structures. If you do not look carefully at these regions, you will miss a significant amount of pulmonary pathology.
Diaphragms
The diaphragms are typically dome-shaped, although many persons have polyarcuate diaphragms that look like several domes rather than one. This is an important normal variant and should not be mistaken for a pleural or diaphragmatic tumor; it should not be called an eventration ( Fig. 3.12 ). The right hemidiaphragm is usually higher than the left, and most people believe that this is because the liver is pushing up the right hemidiaphragm. This is nonsense, because the liver, which weighs many pounds, cannot push up into the lungs while the person is standing. The diaphragms are at different levels because the heart is pushing the left hemidiaphragm down. The edges of both hemidiaphragms form acute angles with the chest wall, and blunting of these angles should raise the suspicion of pleural fluid.

Most people have trouble telling the right from the left hemidiaphragm on the lateral view, but several ways exist to tell them apart. The right hemidiaphragm is usually higher than the left and can be seen extending from the anterior chest wall to the posterior ribs. The left side usually can be seen only from the posterior aspect of the heart to the posterior ribs. It also is the hemidiaphragm that is most likely to have a gas bubble (stomach or colon) immediately beneath it.
Bony Structures
Skeletal structures of interest on a chest x-ray include the ribs, sternum, spine, and shoulder girdle. Twelve ribs should appear, but only the upper ones are completely seen on a PA chest x-ray. Ribs are very difficult to evaluate on the lateral view owing to superimposition of the right and left ribs and the many soft tissue structures. Evaluation should include searches for cervical ribs ( Fig. 3.13 ), fractures, deformity, missing ribs (from surgery), and lytic (destructive) lesions. The upper margin of the ribs is usually well seen, because the rib is rounded here. The lower edge of the ribs is usually very thin, and the inferior cortical margin can be difficult to appreciate. Look for symmetry between the right and left ribs at the same level. If they are symmetric, they are usually normal. At the anterior ends of the ribs, cartilage connects to the sternum. In older individuals, significant calcification of this cartilage may occur; this is a normal finding ( Fig. 3.14 ).

In the case of minor blunt trauma confined to the ribs, a chest x-ray is the initial imaging examination and the addition of dedicated rib views is often not very helpful. Most rib fractures affect the fifth to ninth ribs, likely because the upper ribs are protected by the shoulder girdle and the lower ribs are mobile. Rib fractures after cardiopulmonary resuscitation (CPR) are more commonly anterior and on the left. A PA chest x-ray is specific but not very sensitive for rib fractures, and an AP chest is even less so. Finding a rib fracture is not a big deal but rather should alert you to look for the more significant complications of flail chest, pneumothorax, hemothorax, pulmonary contusion, cardiovascular injury, and potential injury to abdominal organs.
The sternum is well seen only on the lateral view of the chest. On this view, look for pectus deformity, fractures, and lytic lesions. A pectus deformity can cause apparent cardiomegaly, because the sternum is depressed and squashes the heart against the spine, making the heart look wider than normal on the PA chest view ( Fig. 3.15 ). Occasionally, overexposed oblique views of the chest can show the sternum well. If this does not work, you may need to resort to a CT scan with bone windows.

The clavicles and shoulders also should be routinely examined. Often the inferior and medial portions of the clavicle have a scalloped appearance. This is called a rhomboid fossa , and it is bilateral. It should not be mistaken for a pathologic bone lesion ( Fig. 3.16 ). The medial aspect of the scapula projects over the upper lateral aspect of the lungs and sometimes can be mistaken for a pathologic line, such as a pneumothorax. When you think that you see a pneumothorax, make sure that it is not the scapular border. Note that the medial scapular border is usually straight rather than curved, and traces the outline of the scapula.

The thoracic spine is seen only incompletely on a standard chest x-ray because, on the frontal view, it is obscured by the heart and mediastinal structures. In older people, substantial degenerative changes or bone spurs may extend laterally from the vertebral bodies. These can often be seen on the PA view ( Fig. 3.17 ) and, on the lateral view, the spurs can look like pulmonary nodules. A key to differentiating bony spurs from nodules is that spurs project over the vertebral disks on the lateral view and do not look like round nodules on the frontal chest x-ray.

Soft Tissues
The soft tissues also should be examined. We have already seen the problems in interpretation that can arise as a result of a mastectomy or nipple shadows, but other soft tissues also are important. It is important to look for asymmetry of soft tissues and for air or calcium in them. Calcification may be seen in the carotid arteries or great vessels in older persons ( Fig. 3.18 ). A common confusing artifact can be caused by hair (especially braids). If the hair is greasy and braided, strange artifacts that may be mistaken for apical lung infiltrates can be seen ( Fig. 3.19 ).


Normally, not much soft tissue or water density should exist between the peripheral aerated lung and the ribs. The pleura are not normally seen at the lung margins. In some adults, a collection of fat appears along the chest wall between the lung and the ribs. This is extrapleural fat, which is usually seen only on the PA view of the chest and almost always in the upper outer portion of the thoracic cavity ( Fig. 3.20 ). The biggest pitfall is mistaking this for bilateral pleural effusions. If no other sign of effusion (such as costophrenic angle blunting) is noted, and if the finding is bilateral, is seen near the upper lateral lung zones, and does not exceed 3 to 4 mm in thickness, it is almost certainly extrapleural fat rather than pleural fluid.

Computed Tomography Anatomy
The cross-sectional anatomy of the chest is important to understand, because computed tomography (CT) is commonly used for the evaluation of thoracic pathology. CT scanning of the chest may be done with or without intravenous (IV) contrast. Most standard CT scanning techniques provide CT slice images that are 5 mm thick. To evaluate a lung nodule, use thinner cuts, and IV contrast is not needed. For evaluation of a potential dissecting aortic aneurysm, a bolus of IV contrast is essential. Consult a radiologist if you are in doubt about what to order. The radiologist usually will use the correct technique, provided that you have supplied complete clinical information. With current spiral multidetector CT technology, the entire chest can be scanned in several seconds while the patient holds his or her breath. After the scan is done, the data can be manipulated on almost any computer to show bone, mediastinal windows, or pulmonary parenchymal windows. This affords a good look at the pulmonary parenchyma and still allows differentiation of mediastinal structures ( Fig. 3.21 ).




In some special circumstances, you will want to look at the fine details of the lung. In these circumstances, high-resolution computed tomography (HRCT) can be performed. The slices that are obtained are 1 to 2 mm thick. This usually is not done for the whole lung because it would involve too many images, and it is not necessary for making most diagnoses. For this reason, a regular CT scan is often done with thin cuts at selected levels ( Fig. 3.22 ). Repeated chest CT scans for follow-up of pulmonary nodules should be performed using a low-dose protocol.

The Abnormal Chest Image
Admission, Preoperative, and Prenatal Chest X-Rays
Routine admission chest x-rays have a low yield and are not indicated. If a patient is being admitted with a cardiothoracic problem, cancer, or febrile illness, a chest x-ray is appropriate. In a similar fashion, routine preoperative chest x-rays are not indicated (e.g., before foot or knee surgery). Preoperative chest x-rays are indicated for patients who are undergoing neck or chest surgery; have a history of respiratory or cardiac problems; are febrile or immunocompromised; have altered mental status, an acute abdomen, or a known or suspected cancer; or are older than 65 years. A chest x-ray also is appropriate for children who are admitted to an intensive care unit for any reason.
Chest X-Ray Examinations in Occupational Medicine
Preemployment and preplacement chest x-rays should be done selectively based on pertinent factors in the medical history, clinical examination, and proposed work assignment. Surveillance of persons who work with or may be exposed to substances that adversely affect pulmonary function or cause pulmonary disease should be done if this is the diagnostic procedure with the greatest accuracy and earliest detection. The periodicity of such testing would vary with the particular circumstance.
Silhouette Sign
The silhouette sign is one of the most useful signs in interpreting a chest x-ray. It helps determine the location of an abnormality in relation to normal structures. Loss of a normal border occurs if an abnormality is contiguous with that structure. For example, if an infiltrate is identified on the PA or AP image in the lower right lung zone, it could be in either the right middle or right lower lobe. If a loss of the normally distinct right heart border is found, then the infiltrate must abut the heart and can only be in the medial segment of the right middle lobe. If, however, loss of the outline of the right hemidiaphragm is found, the infiltrate is almost certainly in the right lower lobe. The silhouette sign also can be used in the reverse fashion. If on a PA chest x-ray, a mass projects over the aortic knob and the aortic knob is clearly defined, then the mass must be either in front of or behind the aortic knob.
Routine Chest Radiography
The literature over the past four decades does not show evidence for the benefit of a broad utilization of routine chest x-rays, and generally most abnormalities can be predicted with a good history and physical examination. Preoperative examinations in apparently healthy patients have a very low yield. There is increased value when the patient is older than 70 years, when there is a clinical suspicion of cardiopulmonary disease, unreliable history, or confusing physical examination, or the surgery is high risk.
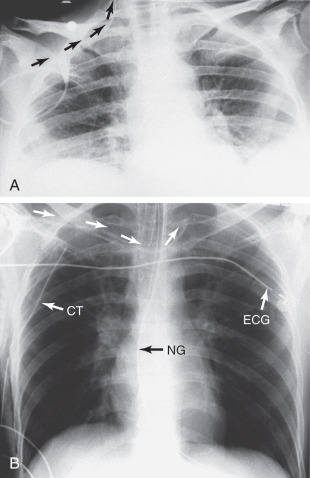
Portable Chest Radiography in the Intensive Care Unit
Much has been written about the utility or overuse of chest x-rays in intensive care units (ICUs). In general, standing or routine orders for a chest x-ray should be avoided. However, by definition, patients in ICUs are very sick, are usually lying supine all day, and are not ventilating normally. Almost all of these patients have supporting tubes or lines that are changed or repositioned frequently. Daily routine chest x-rays are not indicated. Placement of an endotracheal (ET) tube or nasogastric (NG) tube, Swan-Ganz catheter, central venous catheter, or any other life-support item is an indication for a chest x-ray. Change in clinical condition is also an indication. A chest x-ray after chest tube removal is not recommended unless there is a change in clinical condition. Abnormalities to look for on a postsurgical or posttraumatic chest x-ray are shown in Box 3.3 .
Position of the endotracheal tube, pleural tubes, venous catheters
Upper mediastinal widening
Left apical pleural cap
Ill-defined aortic knob or anteroposterior window (signs of aortic tear)
Pneumothorax
Apical
Loculated or basilar
Mediastinal emphysema
Subcutaneous emphysema
Infiltrates (? changing)
Mediastinal shift
Atelectasis
Lobar
Focal
Pleural fluid collection
Rib or sternal fractures
Spine fractures (including paraspinous soft tissue widening)
Shoulder fractures and dislocations
Free air under the diaphragms
Tubes, Wires, and Lines
Evaluation of the placement and associated complications of various tubes, wires, and lines is a common reason for ordering a chest x-ray. For patients who are extremely sick and in an ICU, the portable chest x-ray often resembles a plate of spaghetti with tubes, lines, and wires everywhere. Your job is to figure out which parts of the tubes and wires are inside the patient and which are simply lying on the patient. In addition, you need to know if the lines and tubes that are inside the patient are going to the right place or are at the correct level.
Endotracheal Tube
An ET tube is probably the easiest item to identify, because it is within the air shadow of the trachea. In an adult or child, the ET tip should be at least 1 cm above the carina and preferably slightly more. A tube in a lower position can obstruct airflow to one side and cause atelectasis (collapse) of a lung or a portion of a lung. An ET tube in a low position usually will go into the right main stem bronchus because it is more vertically oriented than the left main stem bronchus ( Fig. 3.23 ). The highest that an ET tube tip should be is at the level of the suprasternal notch, which is midway between the proximal clavicles.

Nasogastric Tube
An NG tube should follow the course of the esophagus on the frontal chest x-ray and, on the lateral view, it should pass behind the trachea and then along the posterior aspect of the heart ( Fig. 3.24 ). You must ascertain the position of the tip of an NG tube before putting any liquid through the tube. The position often can be determined by clinical means without resorting to a chest x-ray. The most common method is to put air into the tube and listen over the stomach with a stethoscope.

NG tubes have two favorite abnormal positions. The most common is with the NG tube only partway down the esophagus or coiled in the esophagus. Fluid placed down the tube can reflux and be aspirated into the lungs. Less commonly during insertion, the NG tube can pass into the trachea instead of going into the esophagus. When this happens, it tends to go down the right main stem bronchus (just as an ET tube that is advanced too far does). Because NG tubes can be stiff and have a rigid end, if pushed hard enough, they can perforate the lung and go out into the pleural space ( Fig. 3.25 ). Many patients require alimentation via an NG tube; this works best if the tube tip is in the distal aspect of the duodenal loop near the ligament of Treitz.
Jugular or Subclavian Venous Line
This is a common route of venous access. The tip of the catheter should optimally be placed in the superior vena cava (SVC). On the frontal chest x-ray, the catheter tip should be about 1 to 4 cm below the medial aspect of the right clavicle ( Fig. 3.26 ). The favorite abnormal positions of subclavian catheter tips are turning up into the jugular vein rather than down into the SVC ( Fig. 3.27A ) and crossing the midline and extending into the opposite subclavian vein (see Fig. 3.27B ).

Swan-Ganz or Pulmonary Artery Catheter
Central lines are usually placed to monitor cardiac or pulmonary arterial pressure. The normal course is almost circular: down the SVC, through the right atrium and right ventricle, and out into the main pulmonary and peripheral pulmonary arteries. The most common natural course that the catheter follows leads it into the right rather than the left main pulmonary artery ( Fig. 3.28 ). Some venous catheters are placed from the inguinal region. In this case, the catheter usually follows a gentle S curve from the inferior vena cava (IVC) into the right atrium and right ventricle and into the pulmonary artery ( Fig. 3.29 ). A central venous catheter placed too far out into a pulmonary artery will obstruct blood flow and can result in pulmonary infarction ( Fig. 3.30 ). The tip of a central venous pressure line should not extend more than halfway between the hilum and the lung periphery, or lung infarction can occur. Another problem encountered is the passage of such a catheter from the SVC into the IVC instead of into the right heart ( Fig. 3.31 ).





Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree