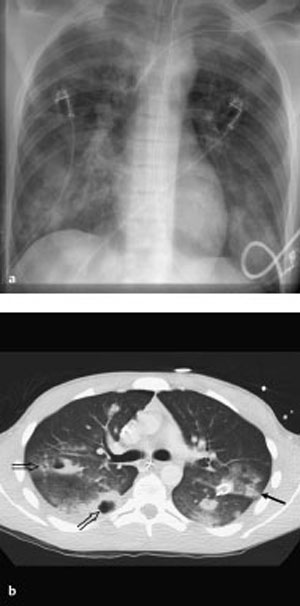
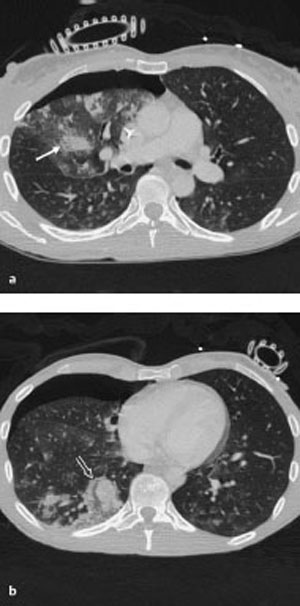
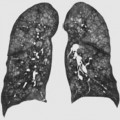
12 Chest Trauma Pulmonary contusions and lacerations represent different degrees of damage to the pulmonary parenchyma; these injuries account for 30–60% of all chest trauma A distinction is made between blunt and penetrating chest trauma, depending on the mechanism of injury Radiographs Homogeneous opacity with an ill-defined border A contusion appears as an ill-defined minimally invasive area of increased density resembling a ground-glass opacity Pulmonary contusions and lacerations are usually clinically asymptomatic Extent of injury Fig. 12.1 Multiple trauma in a 16-year-old boy. a The plain chest radiograph shows coarsely nodular to patchy densities over both lungs. b The CT scan allows better differentiation between the contused areas (arrows), and the lacerations with pneumatoceles (open arrows). Fig. 12.2 Multiple trauma. The CT scans show a right anterior pneumothorax. Contused areas appear as ill-defined areas of nodular opacification (arrow), and hematomas from lacerations as denser sharply demarcated focal lesions (open arrow).
Pulmonary Contusion and Laceration
Definition
 Epidemiology
Epidemiology
 Main causes in everyday life include: Motor vehicle accidents (about 75% of cases)
Main causes in everyday life include: Motor vehicle accidents (about 75% of cases)  Falls from a great height (18%)
Falls from a great height (18%)  Occupational accidents (7%)
Occupational accidents (7%)  Rarely, stab or gunshot wounds (depending on local environmental factors).
Rarely, stab or gunshot wounds (depending on local environmental factors).
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
 Acceleration/deceleration forces predominate in severe chest trauma
Acceleration/deceleration forces predominate in severe chest trauma  Variants include blast injuries, which involve a shock wave
Variants include blast injuries, which involve a shock wave  Shock wave trauma leads to severe tears along the air–tissue interfaces
Shock wave trauma leads to severe tears along the air–tissue interfaces  There is a risk of air embolism, and prompt artificial respiration is required.
There is a risk of air embolism, and prompt artificial respiration is required.
Imaging Signs
 Modality of choice
Modality of choice
 CT in severe chest trauma and multiple trauma.
CT in severe chest trauma and multiple trauma.
 Radiographic findings
Radiographic findings
 Laceration is distinguishable from contusion only by the presence of pneumatoceles or dense hematoma
Laceration is distinguishable from contusion only by the presence of pneumatoceles or dense hematoma  Findings manifest themselves within hours of the injury
Findings manifest themselves within hours of the injury  Contusions resolve within days; lacerations heal in weeks to months.
Contusions resolve within days; lacerations heal in weeks to months.
 CT findings
CT findings
 Lacerations are denser and more inhomogeneous
Lacerations are denser and more inhomogeneous  Air inclusions with air–fluid levels are consistent with traumatic pneumatoceles.
Air inclusions with air–fluid levels are consistent with traumatic pneumatoceles.
Clinical Aspects
 Typical presentation
Typical presentation
 Gas exchange is impaired only where there is extensive parenchymal damage with associated injuries (unstable chest, pneumothorax, hemothorax)
Gas exchange is impaired only where there is extensive parenchymal damage with associated injuries (unstable chest, pneumothorax, hemothorax)  Blast injuries are invariably associated with respiratory insufficiency.
Blast injuries are invariably associated with respiratory insufficiency.
 What does the clinician want to know?
What does the clinician want to know?
 Associated injuries requiring treatment (hemothorax, pneumothorax, tension pneumothorax, unstable chest, aortic rupture, rupture of the diaphragm).
Associated injuries requiring treatment (hemothorax, pneumothorax, tension pneumothorax, unstable chest, aortic rupture, rupture of the diaphragm).
Differential Diagnosis
Sequelae of aspiration | – Gravitational location and segmental distribution – Sequelae of trauma do not respect anatomic borders except for the interlobar fissures |
Atelectasis | – Volume loss of varying degrees – Uniform enhancement on contrast CT |
Tips and Pitfalls
In contrast to CT, less extensive associated pleural injuries (pneumothorax or hemothorax) are easily overlooked on plain chest radiographs  Such injuries usually do not require treatment.
Such injuries usually do not require treatment.
Selected Reference
Schnyder P, Wintermark M. Radiology of blunt trauma of the chest. Berlin: Springer; 2000
Aortic Rupture
Definition
 Epidemiology
Epidemiology
Aortic ruptures occur in about 1–2% of all cases of chest trauma (> 80% are fatal)  Traffic accidents are the most common cause.
Traffic accidents are the most common cause.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Acceleration/deceleration forces predominate in severe chest trauma  Intimal flap
Intimal flap  Intramural and/or periaortic hematoma.
Intramural and/or periaortic hematoma.
Imaging Signs
 Modality of choice
Modality of choice
CTA.
 Radiographic findings
Radiographic findings
Abnormal widening of the upper mediastinum (> 8 cm) in combination with signs of a mass (trachea and esophagus shifted to the right; left main bronchus is also shifted)  High negative predictive value where plain chest radiograph is normal (98%).
High negative predictive value where plain chest radiograph is normal (98%).
 CTA findings
CTA findings
Aortic rupture on CTA appears as an abrupt change in caliber  Abnormal aortic contour
Abnormal aortic contour  Intimal flap
Intimal flap  Intramural and/or periaortic hematoma.
Intramural and/or periaortic hematoma.
Clinical Aspects
 Typical presentation
Typical presentation
Cardinal symptom of aortic rupture is shock, a sign of which may be a difference in blood pressure between the right and left arms or between the upper and lower halves of the body.
 What does the clinician want to know?
What does the clinician want to know?
Confirm and localize or exclude  Hemothorax
Hemothorax  Associated injuries.
Associated injuries.
Differential Diagnosis
Mediastinal hematoma | – Most mediastinal hematomas are caused by bleeding from smaller vessels – Wherever mediastinal widening is observed in the setting of trauma, one must consider the possibility of a spinal fracture in addition to vascular injury |
Tips and Pitfalls
Pulsation artifacts can mimic aortic dissection (pulsation artifacts change direction and location in every slice).
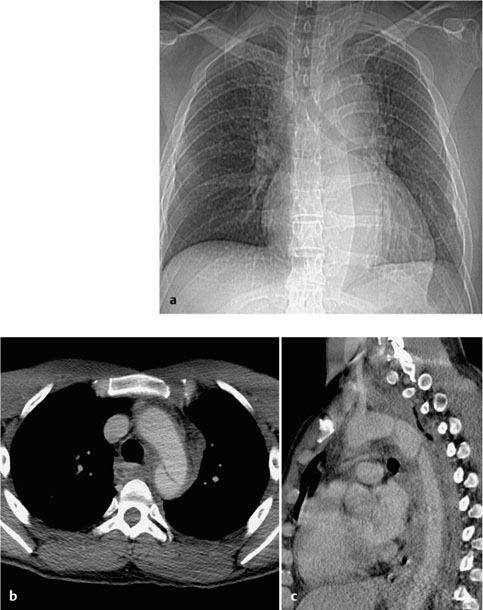
Fig. 12.3 Contained aortic rupture in a 40-year-old man with multiple trauma.
a The plain chest radiograph shows widening of the upper mediastinum. The knob of the aorta is no longer clearly distinguishable although the contour descending aorta still is. The left main bronchus is elongated and displaced. There is slight tracheal shift.
b, c CT demonstrates the aortic rupture at a typical location distal to the origin of the subclavian artery, with an intimal flap. There is an associated periaortic hematoma.
Selected Reference
Wintermark M, Wicky S, Schnyder P. Imaging of acute traumatic injuries of the thoracic aorta. Eur Radiol 2002; 12: 432–442
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree