Fig. 4.1
(a)–(c) Select sagittal, coronal, and axial T2 images from a 3-T MRI of the right knee without contrast. A contained grade IV lesion measuring approximately 8 mm involving the lateral femoral condyle. There is a small amount of signal within the underlying bone without any cyst formation or bone loss
The patient had continued symptoms at the end of the season, particularly lateral joint line pain and swelling. Given the MRI findings of a full-thickness chondral defect involving the lateral femoral condyle, surgical treatment was discussed. After reviewing the risks and benefits, the patient elected to pursue a diagnostic arthroscopy and likely microfracture of the chondral defect.
Arthroscopy
The patient was taken to the operating room and placed in the supine position. A standard diagnostic arthroscopy of the right knee was performed. Multiple small chondral loose bodies were identified, measuring <2 mm, demonstrated in Fig. 4.2a, b. A small, focal grade IV chondral defect was identified involving the lateral femoral condyle. It measured 4 mm in size and was surrounded by an approximate 4 mm rim of mild grade II chondral changes, seen in Fig. 4.2c. Finally, there was a small horizontal cleavage tear involving the lateral meniscus, which was flipped into the femoral notch, demonstrated in Fig. 4.3a, b. These arthroscopic findings of the chondral defect correlated nicely with the MRI findings.
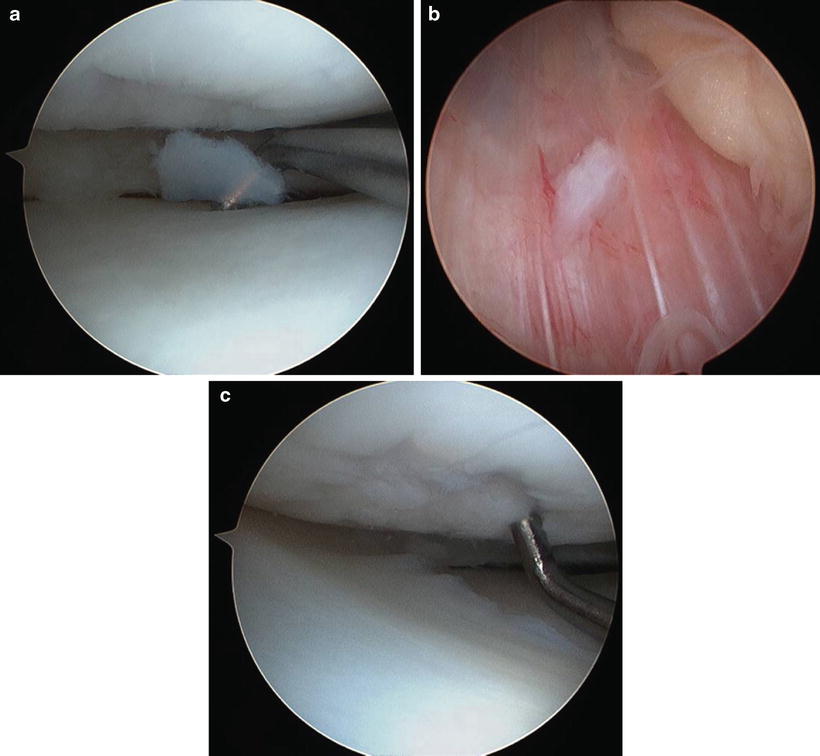
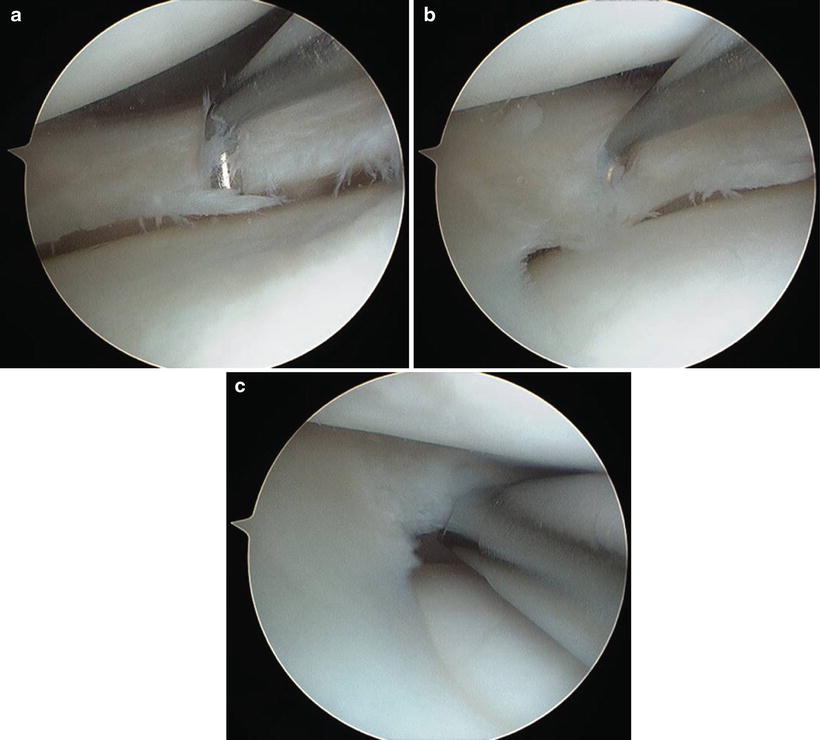
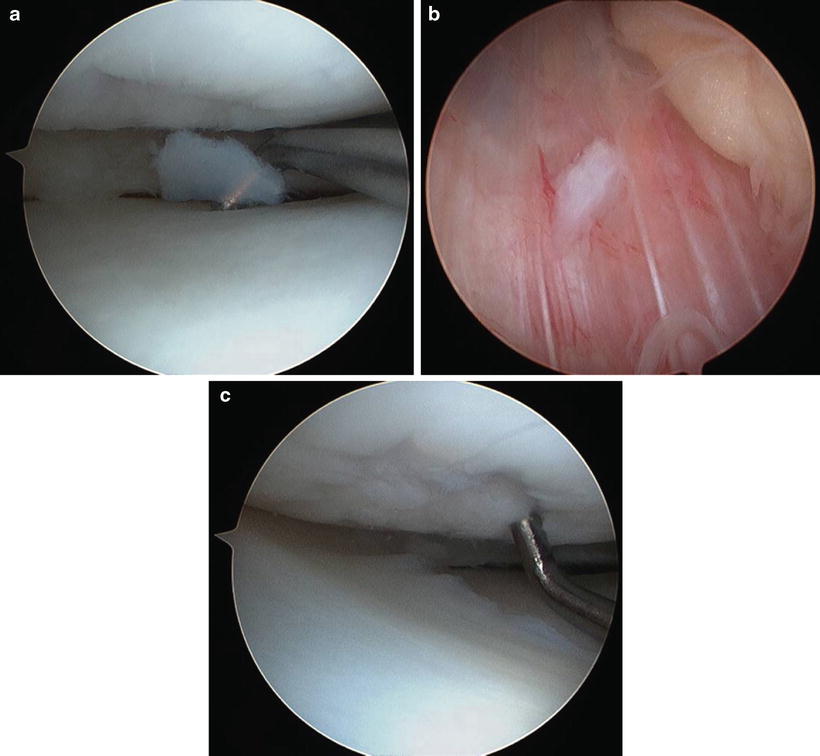
Fig. 4.2
(a)–(c) Two arthroscopic views demonstrating loose chondral pieces measuring 2–4 mm. A chondral defect involving the lateral femoral condyle measuring approximately 8 mm
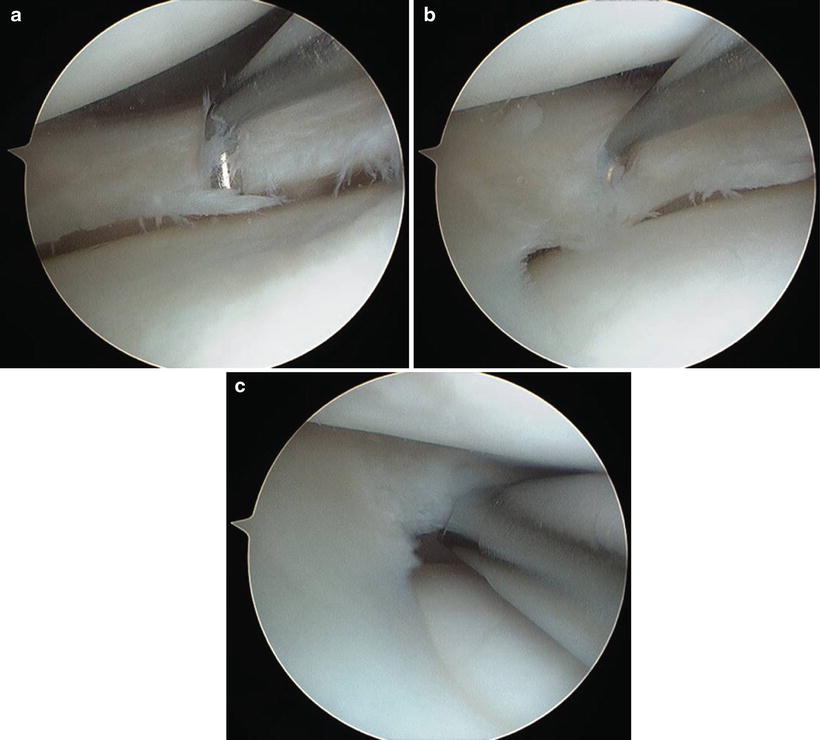
Fig. 4.3
(a)–(c) Two arthroscopic views depicting the horizontal cleavage tear involving the lateral meniscus. There was an unstable flap component that could be displaced into the joint with an arthroscopic probe. The tear was debrided with a 4.0 mm arthroscopic shaver
The small chondral loose bodies were removed with a 4.0 mm arthroscopic shaver without difficulty. The horizontal cleavage tear involving the lateral meniscus was addressed with a partial meniscectomy using the arthroscopic biters and shaver, shown in Fig. 4.3c. Finally, the chondral defect of the lateral femoral condyle was addressed. The cartilage defect was debrided down to the subchondral bone. Care was taken to maintain stable shoulders around the defect. A microfracture awl was then used to penetrate the subchondral bone. The arthroscopic fluid flow was turned off, and bleeding from the microfracture holes was confirmed, seen in Fig. 4.4a, b.
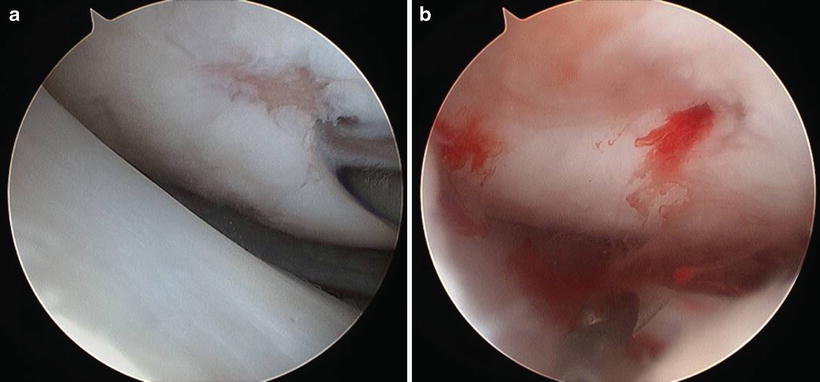
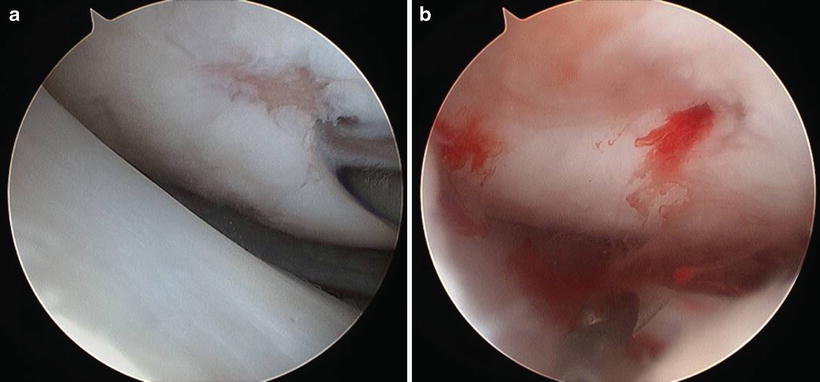
Fig. 4.4
(a, b) Arthroscopic views of the chondral lesion after debridement to stable shoulders showed that the area of grade IV changes was 4 mm with a surrounding 4 mm ring of grade II changes. An arthroscopic awl was used to perform a microfracture. When flow was turned off, there was bleeding from the microfracture holes
Case 2: Grade IV Femoral Condyle Lesion Treated with Osteochondral Autograft Transplantation (OATS)/Mosaicplasty
History/Exam
A 33-year-old male presented with a 6-month history of waxing and waning left knee pain. He initially experienced pain when he hyperextended his knee while removing an engine block from an automobile. He felt a pop in his knee and developed laterally based pain and an effusion within hours of the injury. He treated the knee conservatively and had a resolution of his pain and effusion. However, as these symptoms resolved, he began to develop a sense of instability. One instability event leads to another hyperextension event with sharp lateral pain and effusion development. His lateral pain, effusions, and instability have continued since the second hyperextension injury.
On physical examination the left knee was found to have intact skin with no erythema or warmth. There was a moderate-sized effusion. The knee was tender along the lateral joint line. Active range of motion was noted to be 15°–90° of flexion. Passively, the knee’s range of motion improved to 10°–100°. Pain was recreated laterally with deep flexion. McMurray testing produced a lateral catch and pain. The knee was stable to varus and valgus stress. The Lachman’s, anterior drawer, and posterior drawer were negative. The remainder of the extremity was neurovascularly intact.
Imaging
Plain radiographs of the left knee demonstrated well-maintained joint spaces on the AP and Rosenberg views. No lucencies were identified on AP or lateral views, as shown in Fig. 4.5a, b.
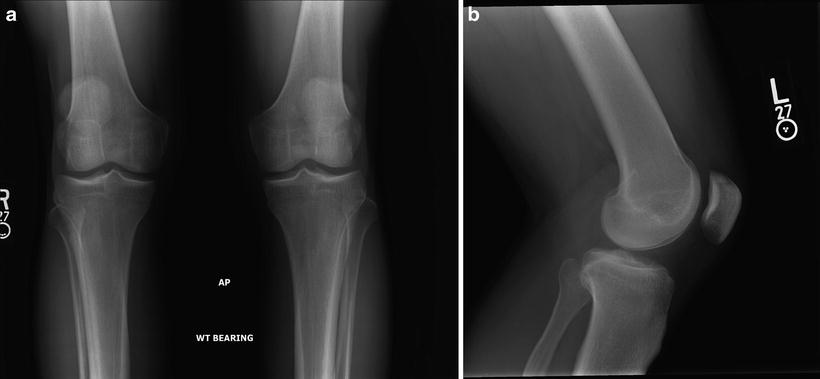
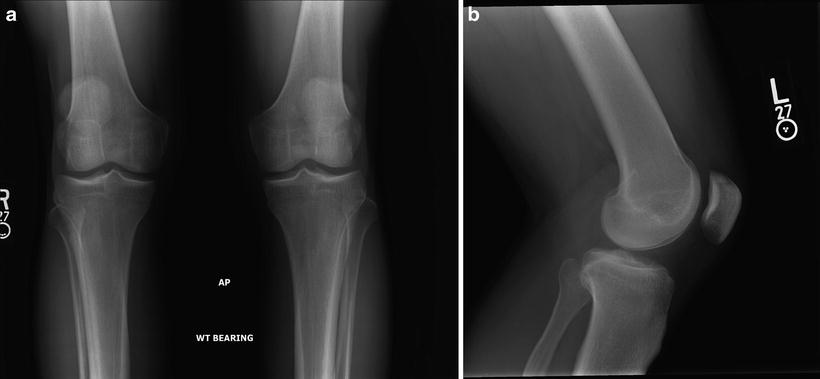
Fig. 4.5
(a, b) AP and lateral views of the left knee showing well-maintained joint spaces with no lucencies
Magnetic resonance imaging was obtained to further evaluate the meniscus and chondral surfaces. A full complement of images was obtained. The technique used included fat-suppressed, fast T2-weighted images acquired axially, sagittally, and coronally, as well as T1-weighted sagittal images.
The MRI demonstrated bone marrow edema involving the posterolateral femoral condyle. The cartilage overlying this area of bony edema had a notable signal abnormality on T2 images. There was a linear band of signal intensity at the interface between the cartilage and subchondral bone, which was suggestive of a delamination or flap. The area of delamination measured approximately 1.4 cm in the anterior to posterior dimension. A small joint effusion was present, demonstrated in Fig. 4.6a, b. The remainder of the MRI was normal.


Fig. 4.6
(a, b) Select sagittal and coronal T2 views of the left knee with a 3-T MRI without contrast. They demonstrate a chondral lesion involving the posterior portion of the lateral femoral condyle. There is fluid signal between the cartilage and underlying subchondral bone, suggesting a flap-type configuration to the chondral lesion. The lesion measures 15 mm in the AP dimension and 9 mm in the medial to lateral dimension. There is also signal within the bone without cyst formation or bone loss
Given the patient’s continued lateral pain and effusion, arthroscopy and possible cartilage procedure were discussed. After reviewing the risks and benefits of surgery, the patient decided to proceed with surgery.
Arthroscopy
The patient was taken to the operating room and placed in the supine position. A standard diagnostic arthroscopy of the right knee was performed. A grade IV chondral defect with an overlying flap of cartilage was found involving the lateral femoral condyle with the knee flexed to 45°. It measured 9 mm in the medial to lateral dimension and 15 mm in the anterior to posterior dimension. It was slightly narrower at its most anterior portion, demonstrated in Fig. 4.7a, b. This correlated to the MRI images.
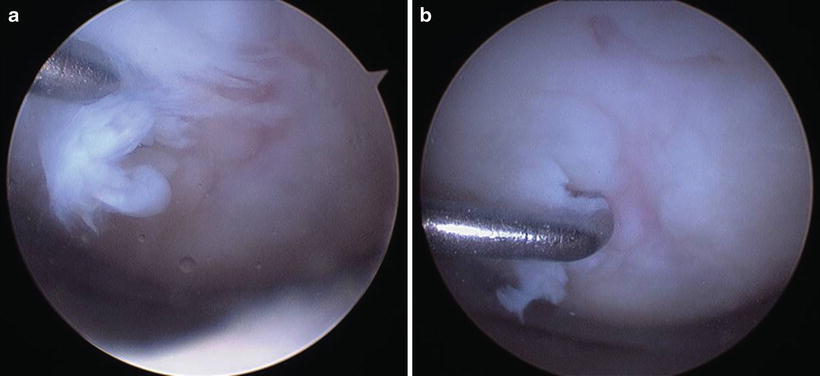
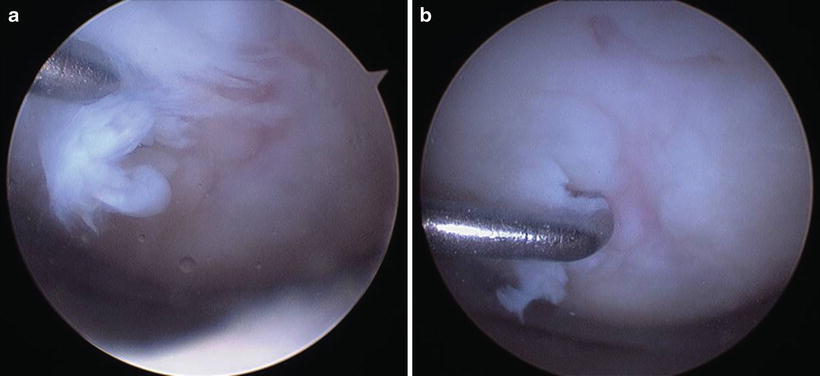
Fig. 4.7
(a, b) Arthroscopic views showing a large flap lesion of the posterior portion of the lateral femoral condyle with the knee flexed to 45°
The defect was debrided down to the subchondral bone with an arthroscopic shaver and sized with the osteochondral autograft transplantation system, as shown in Fig. 4.8a–c. It was decided to use the superomedial aspect of the trochlea as the donor sight for the osteochondral autograft. Two donor plugs were harvested from this region, measuring 10 × 14 mm and 6 × 14 mm, respectively. The transplant site was then prepared by removing a 10 × 12 mm and 6 × 12 mm core of bone. The 10 × 4 mm donor plug was then placed into the corresponding hole followed by the 6 × 14 mm donor plug, demonstrated in Fig. 4.9a–c.
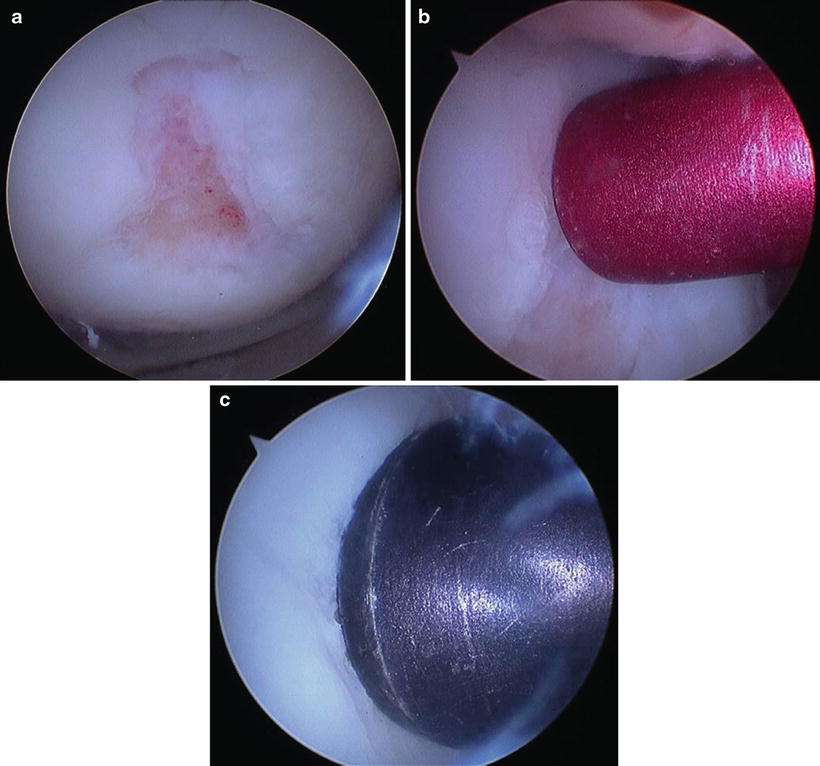
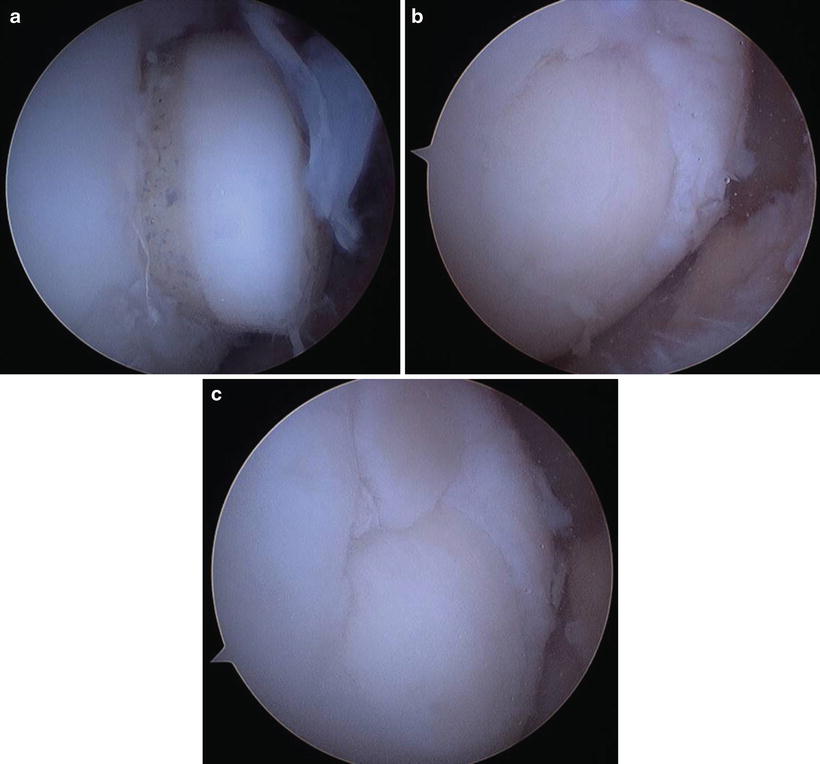
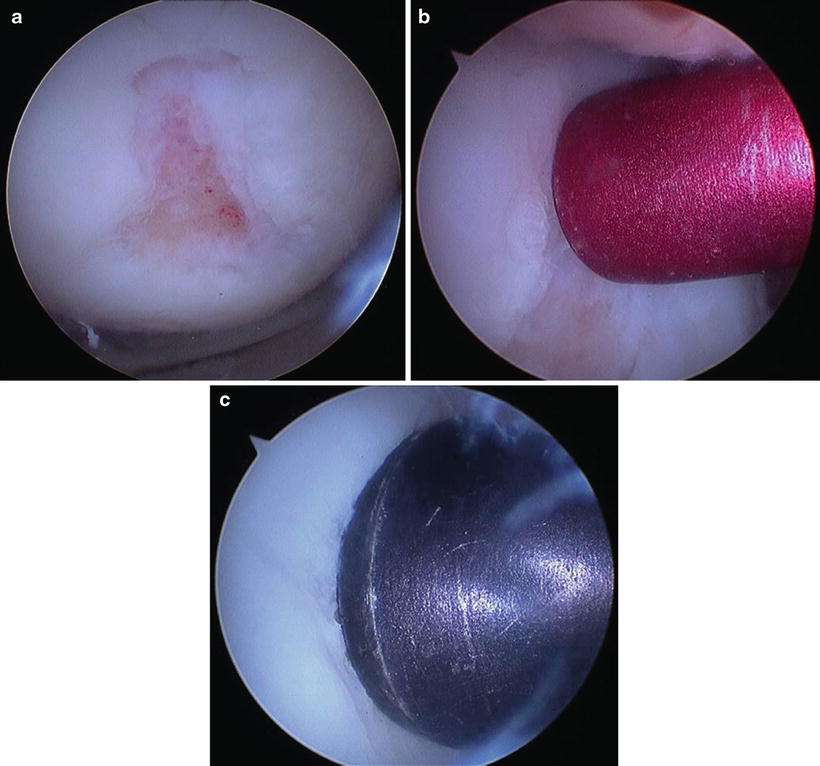
Fig. 4.8
(a)–(c) Arthroscopic view of the lesion after debridement. The two components of the lesion measured 6 mm and 10 mm in diameter, respectively
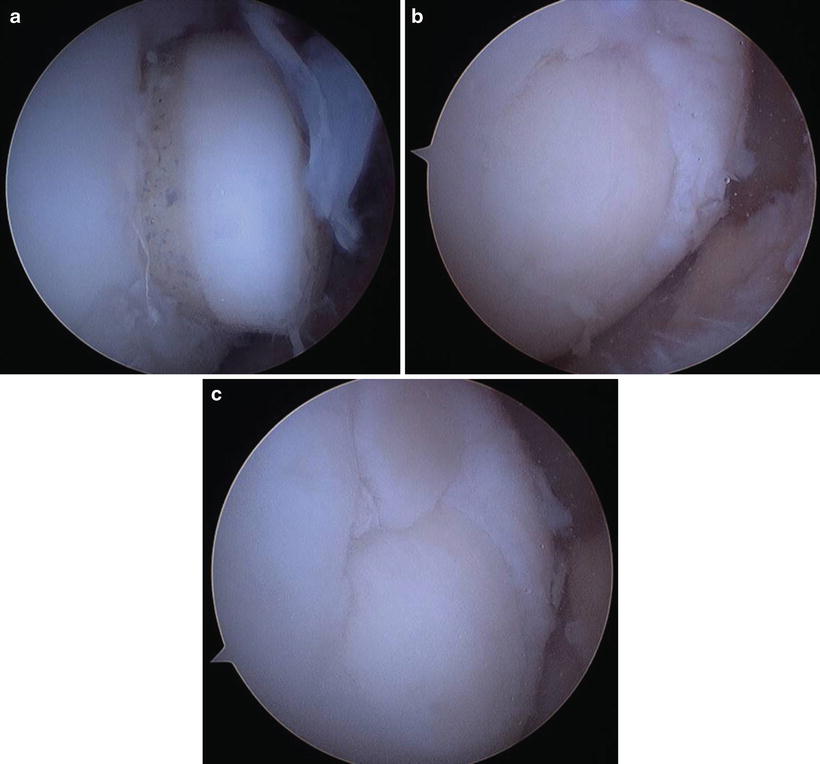
Fig. 4.9
(a)–(c) Arthroscopic views of the 10 × 14 mm plug being advanced into its receiving site until it was flush. Final arthroscopic view of the final two plugs in place at their receiving sites
Discussion for Microfracture and OATS/Mosaicplasty
Cartilage lesions are evident on both T1 and T2 MR sequencing. These lesions can appear as cartilage thinning, fissuring, or full-thickness defects. The full-thickness defects are easily identified on T2 imaging, as the defect will fill with joint fluid. This shows up as a bright white signal within the cartilage defect extending to the black layer of the subchondral bone. Depending on how long the defect has been present, its size, and the overall limb alignment, the underlying bone may have white signal within it on T2-weighted images signifying bony edema.
During arthroscopy, cartilage lesions will present in many different ways. The Outerbridge classification helps to define the severity of these defects. Grade I chondral changes present as cartilage softening and/or blistering. Grade II chondral changes appear as mild thinning of the cartilage and possible fissuring. The fissures do not extend down to the subchondral bone. Grade III chondral changes present as cartilage thinning and fissuring that extends all the way to the subchondral bone. Finally, grade IV changes appear as full-thickness cartilage defects that extend to the subchondral bone.
In treating these chondral lesions, grade I changes are typically left alone. Grade II changes are debrided to stable transitions between the normal and thinned cartilage. Grade III and grade IV chondral defects require more aggressive treatment. The treatment begins with debriding the lesions back to a stable cartilage shoulder. The calcified cartilage layer is then removed, exposing the subchondral bone. Further decisions on treatment are then made depending on the relative size of the lesion.
Microfracture and other bone marrow-stimulating techniques work well for lesions less than 2 cm2. Short-term results are good. However, the longevity of the fibrocartilage that fills in the cartilage defect is questionable in long-term studies secondary to the fibrocartilage’s inferior biomechanical properties compared to hyaline cartilage.
OATS is reserved for lesions that are typically less than 10 mm2 or a stacked lesion, as seen in Case 2. Mosaicplasty can be used for larger lesions. The benefit of these procedures is that the cartilage defect is being filled with hyaline cartilage, with only a small band of fibrocartilage forming between the donor plug and surrounding cartilage. The disadvantage of these procedures is the morbidity of taking the donor plug from a non-weight-bearing portion of the knee. Another disadvantage of mosaicplasty is that it is likely that more fibrocartilage will fill in between the various plugs.
Case 3: Nontraditional, Unstable Osteochondritis Dissecans (OCD) of the Knee Treated with Arthroscopic Fixation
History/Exam
A 13-year-old female presented to the orthopedic clinic after a 3-week history of right knee pain. This began as she increased her activity from softball to playing for three separate basketball teams. The pain was localized to the deep, lateral portion of the knee. It was aggravated by knee flexion and impact from running and jumping. There was associated swelling since the pain began, along with clicking and catching. She stated that the knee gave out on average of two times per day. She found that ice helped with the symptoms, but NSAIDS were not helpful. Of interest, the patient’s older sister had a history of osteochondritis dissecans.
On exam, the right knee had intact skin. There was a small effusion. The knee was tender to palpation along both the medial and lateral joint lines. The knee was stable to varus and valgus stress. The Lachman’s, anterior drawer, and posterior drawer test results were negative. McMurray and Wilson test results were also negative.
Imaging
Plain radiographs of the right knee demonstrated well-maintained joint spaces on the AP and Rosenberg views. There were no identified lucencies on these two views. On the Merchant view, a lucency was identified over the lateral trochlea. A suggestion of this lucency was also seen on the lateral, as shown in Fig. 4.10a, b.
Fig. 4.10
(a, b) Merchant and lateral views of the right knee showing a lucency at the lateral trochlea
Magnetic resonance imaging was obtained to further evaluate the meniscus and chondral surfaces. A full complement of images was obtained. The technique used included fat-suppressed, fast T2-weighted images acquired axially, sagittally, and coronally, as well as T1-weighted sagittal images.
A 16 × 19 mm osteochondral lesion was noted in the superior aspect of the lateral trochlea. There was a fragmented and sclerotic fragment overlying the osteochondral lesion. Fluid extended deep to the fragment, and there was subjacent marrow edema, all seen in Fig. 4.11a–c. The chondral surfaces of the patella, medial compartment, and lateral compartment were found to be intact. The medial meniscus and lateral meniscus were normal. All ligamentous structures were intact.
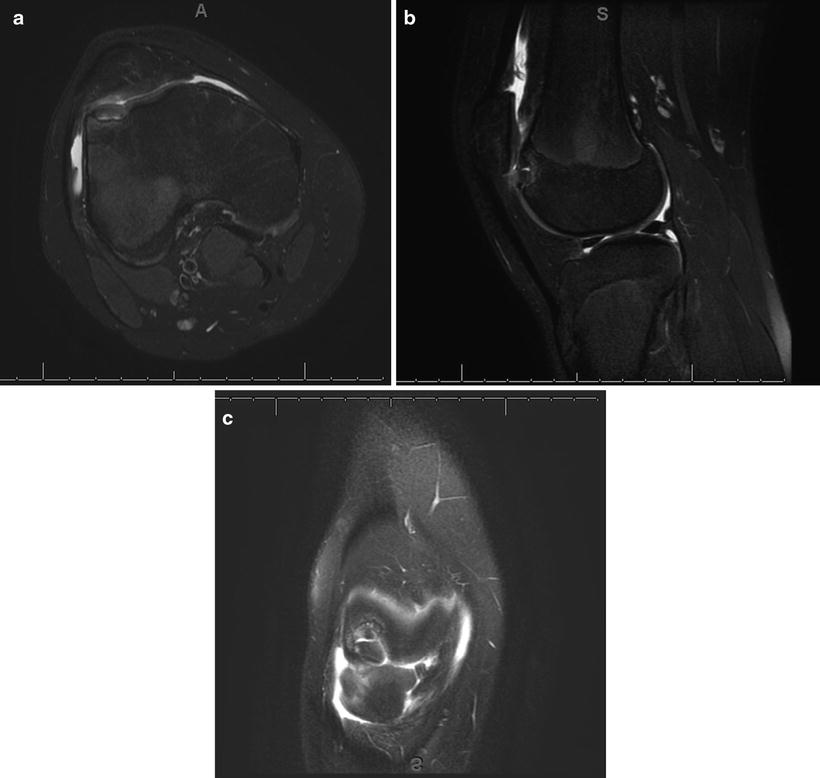
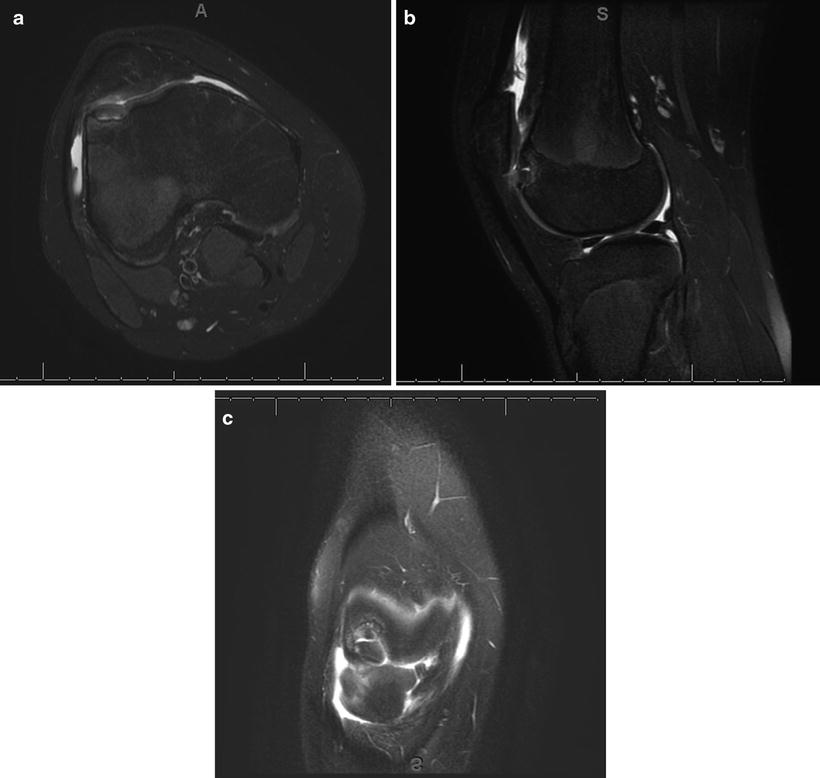
Fig. 4.11




(a)–(c) Select axial, sagittal, and coronal T2 views of the right knee from a noncontrast 3-T MRI. They demonstrate an unstable OCD lesion of the lateral trochlea which is fragmented and measures 16 × 19 mm
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








