Location: 85 % in the sacrococcyx or in the spheno-occipital region. Fifteen percentage in the vertebral body.
Clinical: Early symptoms in C. of the base due to compression of the hypophysis, the optic, oculomotor nerves, obstruction of the nose-pharynx, expansion in the pontocerebellar angle, and increase of intracranial pressure. Late symptoms in C. of the sacrum: insidious pain, constipation, hemorrhoids, dysuria, limping, hypoesthesia, and sphincteric paresis. Rare palpable swelling. In vertebral locations: signs of myeloradicular compression.
Imaging: On X-ray—osteolytic lesion of the clivus and sella turcica, of the sacrum. The outlines of bone and lines of the sacral foramina have disappeared. Ill-defined margins of the lesion that is central. Faded radiopaque spots of intratumoral calcifications. In the vertebral body relatively well-defined edge, with sclerotic rim, calcifications. On bone scan—uptake. On CT—extraosseous mass protruding more anteriorly than posteriorly in the sacrum, well-defined borders, infiltration of the adjacent muscles, and dislocation of the viscera or of the dural sac. On MRI—relationship between tumor and rectum, level of rising in the sacral canal, hypointense, homogeneous on T1, inhomogeneous, hyperintense, bright on T2.
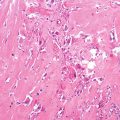
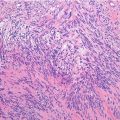
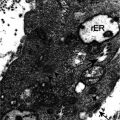
Histopathology: Small in the base of the skull, very large in the sacrum. Lobular, grayish, soft, gelatinous, mucoid aspect with frequent areas of hemorrhage, necrosis, and cystic changes. Lobular pattern with long ribbon or nests of large round cells embedded in a pinkish gelatinous appearance, with oval, round nuclei, and abundant cytoplasm with many fine, clear, mucous-filled vacuoles of different size which give a bubbly aspect, hence the term physaliferous cell. Cells arranged in strands separated by a faintly eosinophilic amorphous mucous, few cells in a large mass of mucoid to myxoid stroma. Nuclei mostly lie in the center of the cell giving a bull’s-eye or target appearance. Relatively vascular, frequent blood vessels in fibrovascular shoots among the tumoral lobules. Frequent cartilaginous differentiation is observed in C. of the base of the skull.
Course and Staging: Slow growth, frequent local recurrences if surgery is not adequate, rare, and late metastases (10 % of C. of the sacrum). Usually, stage IB, very few cases as stage IA, rarely as stage IIB.
Treatment: Wide resection is mandatory, but often impossible. Little hope of avoiding recurrence if marginal or contaminated excision is performed. Radiotherapy is effective and useful. Many C. of the base of the skull cause death within 2–3 years. Cases with cartilaginous differentiation have a better prognosis. Although recurrence may be reoperated many times and metastases are late, survival after 10 years for C. of the sacrum is very low because surgery is late and inadequate.
Key Points
Clinical | Old patients, pain and compression symptoms |
Radiological | Pure lytic lesion |
Histological | Lobular pattern with physaliferous cells |
Differential diagnosis | Bone metastasis and all other primary purely osteolytic lesions of adults—benign notochordal cell tumor |
Immunohistochemical Panel
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree