Presentation and Presenting Images
( ▶ Fig. 60.1, ▶ Fig. 60.2, ▶ Fig. 60.3, ▶ Fig. 60.4, ▶ Fig. 60.5, ▶ Fig. 60.6)
A 42-year-old female with right breast cancer treated with a mastectomy presents for screening mammography.
60.2 Key Images
( ▶ Fig. 60.7, ▶ Fig. 60.8, ▶ Fig. 60.9, ▶ Fig. 60.10, ▶ Fig. 60.11)
60.2.1 Breast Tissue Density
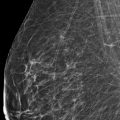
The breasts are heterogeneously dense, which may obscure small masses.
60.2.2 Imaging Findings
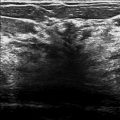
The right breast is surgically absent. The left breast demonstrates an oval mass with obscured margins (circle) in the lower inner quadrant at the 7 o’clock location in the anterior depth, 3 cm from the nipple ( ▶ Fig. 60.7, ▶ Fig. 60.8, ▶ Fig. 60.9, ▶ Fig. 60.10, and ▶ Fig. 60.11). There are two postbiopsy clips in the left breast that denote the sites of prior benign biopsies. The bar-shaped clip marks a prior magnetic resonance (MR) biopsy of a fibroadenomatoid change, stromal fibrosis, and findings suggestive of intraductal papilloma. The baby-diaper–shaped clip marks a prior ultrasound biopsy of a fibroadenoma.
60.3 BI-RADS Classification and Action
Category 0: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
60.4 Diagnostic Images
( ▶ Fig. 60.12, ▶ Fig. 60.13, ▶ Fig. 60.14, ▶ Fig. 60.15)
60.4.1 Imaging Findings
Spot-compression digital breast tomosynthesis (DBT) movies were done to further evaluate the obscured mass in the left breast. Slices from these movies confirm the mammographic suspicion of a mass and show the mass’s margins to be circumscribed ( ▶ Fig. 60.12 and ▶ Fig. 60.13). A targeted ultrasound reveals an oval hypoechoic mass with circumscribed margins at the 6 o’clock location ( ▶ Fig. 60.14 and ▶ Fig. 60.15). This mass underwent ultrasound-guided biopsy.
60.4.2 BI-RADS Classification and Action
Category 4A: Low suspicion for malignancy
60.5 Differential Diagnosis
Fibroadenoma: Fibroadenomas may range from isoechoic to hypoechoic with variable posterior acoustic enhancement. Fibroadenomas do not have a true capsule; the thin echogenic capsule seen on sonography is a pseudocapsule caused by the compression of adjacent tissue. The vascularity of solid masses does not help distinguish a cancer from a fibroadenoma.
Complicated cyst: Complicated cysts may have sonographic features similar to fibroadenomas.
Ductal carcinoma in situ (DCIS): DCIS typically presents as a group of calcifications varying in size, density, and form. A mass lesion is an uncommon presentation for DCIS.
60.6 Essential Facts
Fibroadenomas are solid, benign fibroepithelial breast masses that occur most often in young women.
Benign-appearing masses should not be dismissed as benign. Sonography is required to definitively characterize masses. Benign and malignant entities may present as benign-appearing or well-circumscribed masses on tomosynthesis.
In this case, specifically, this patient is at an increased risk of developing a malignancy given her personal history of breast cancer.
The mass is better seen on tomosynthesis than on conventional mammography. Digital breast tomosynthesis (DBT) is excellent at localizing masses, which is helpful to guide the sonographic evaluation.
If the finding was not seen on sonography, it could have been biopsied under the guidance of tomosynthesis.
60.7 Management and Digital Breast Tomosynthesis Principles
Tomosynthesis systems are highly flexible and support screening mammography, diagnostic mammography, stereotactic biopsies, and tomosynthesis all with one machine.
The anatomical structures of the breast inherently can obscure findings due to overlapping tissue. DBT overcomes the limitations of overlapping tissue.
The DBT system moves in an arc over the breast generating low-dose images. The data is compiled into a three-dimensional (3D) volume set, which may be viewed as a single slices or a cine movie. This allows for better detection and analysis of breast lesions over conventional imaging.
Only findings within an imaged section appear sharp, whereas those above or below appear out of focus.
60.8 Further Reading
[1] Enhancing imaging capabilities with breast tomosynthesis. Siemens white paper. Accessed 12/25/2015. Available at: http://www.healthcare.siemens.com/siemens_hwem-hwem_ssxa_websites-context-root/wcm/idc/groups/public/@global/@imaging/@mammo/documents/download/mdaw/mtuy/~edisp/enhancing_imaging_capabilities_with_breast_tomosynthesis-00078508.pdf
[2] Smith A. Fundamentals of breast tomosynthesis. Improving the performance of mammography. Hologic white paper. Accessed 12/25/2015. Available at: http://www.hologic.com/sites/default/files/Fundamentals%20of%20Breast%20Tomosynthesis_WP-00007.pdf
[3] Souchay H, Carton A-K, Iordache R. Boosting dose efficiency with digital breast tomosynthesis. GE white paper. Accessed 12/25/2015. Available at: https://www.google.co.in/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0ahUKEwjA-NnigePMAhWKNI8KHRh6AP8QFgghMAA&url=http%3A%2F%2Fwww3.gehealthcare.com.br%2F~%2Fmedia%2Fdownloads%2Fbr%2Fsenoclaire_dose_white_paper_-_doc1403841.pdf%3FParent%3D%257B10196544–07D9–4A31–95BB-DD2D94F05C16%257D&usg=AFQjCNEZqb51t7uNyS1TGyT2S_kzhrHkJA&bvm=bv.122129774,d.c2I

Fig. 60.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree