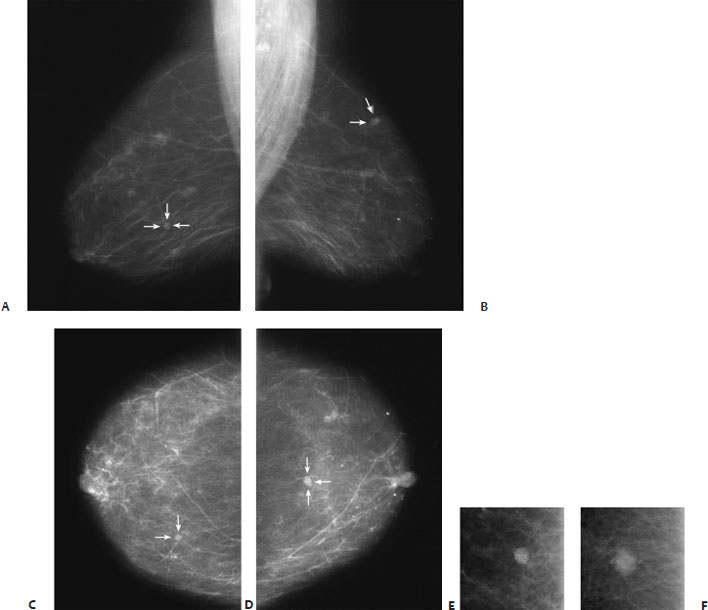
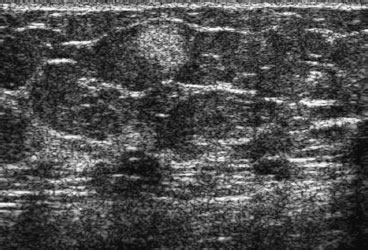
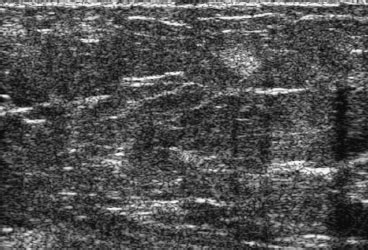
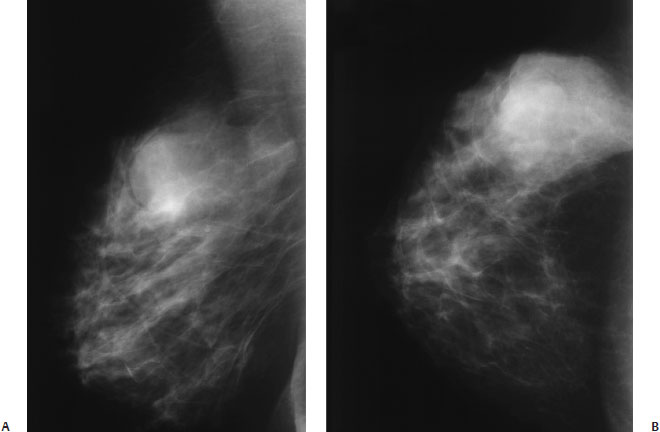
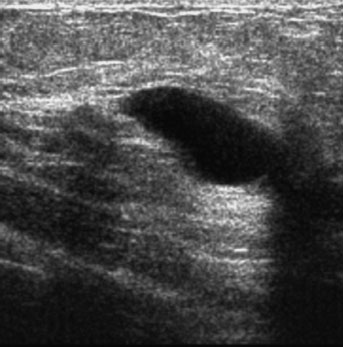
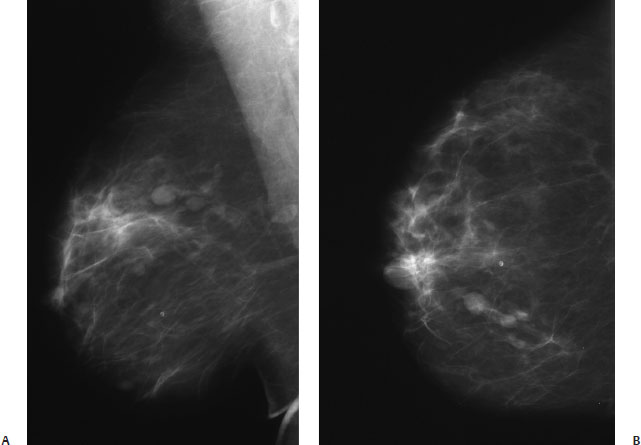
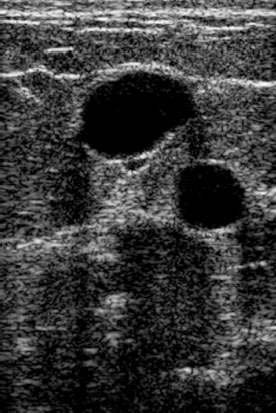
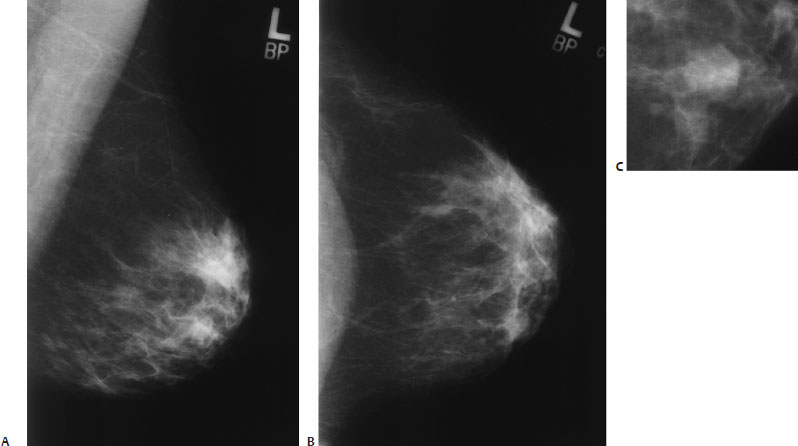
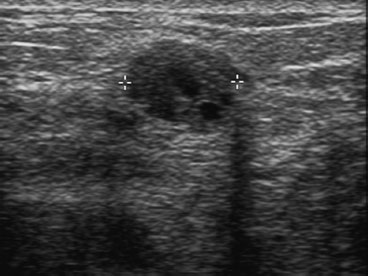
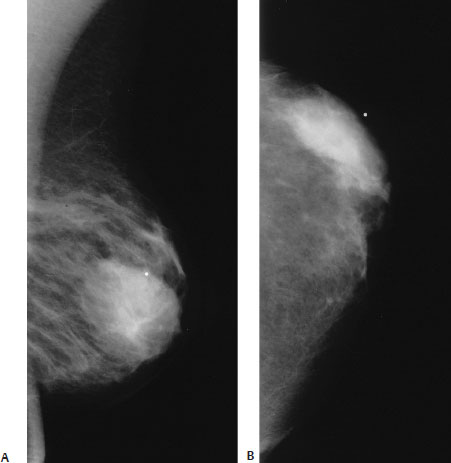
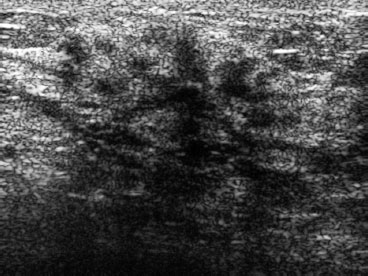
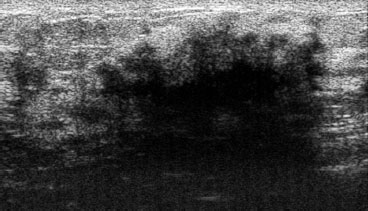
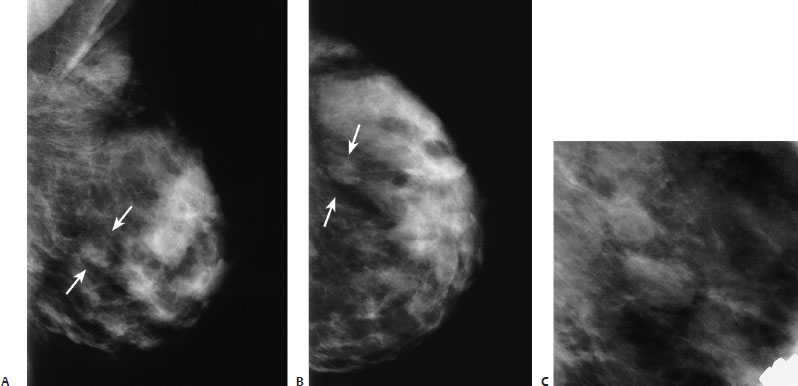
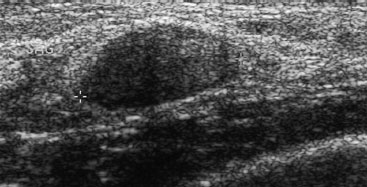
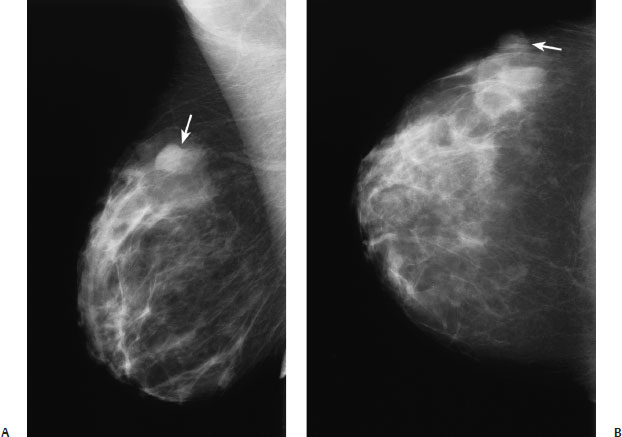
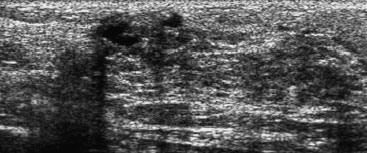
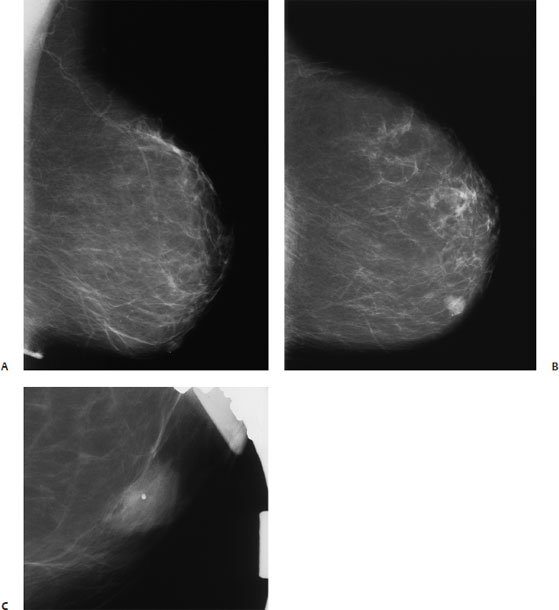
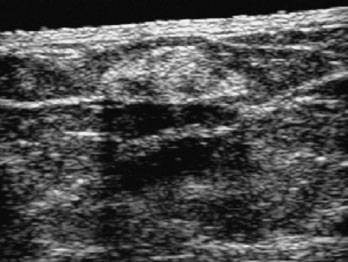
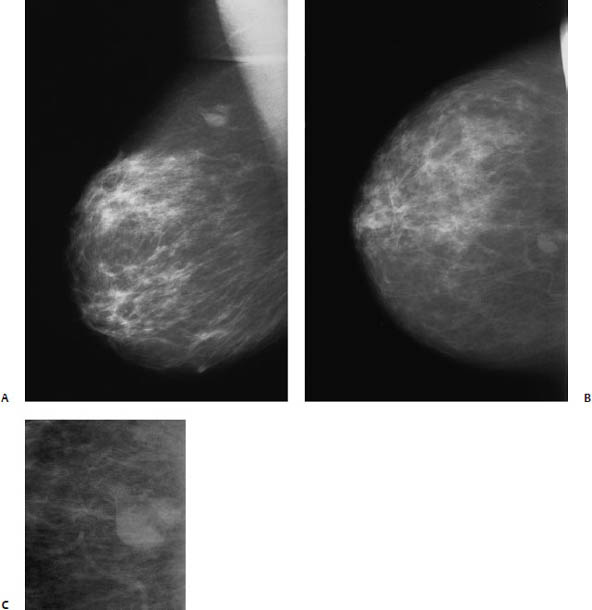
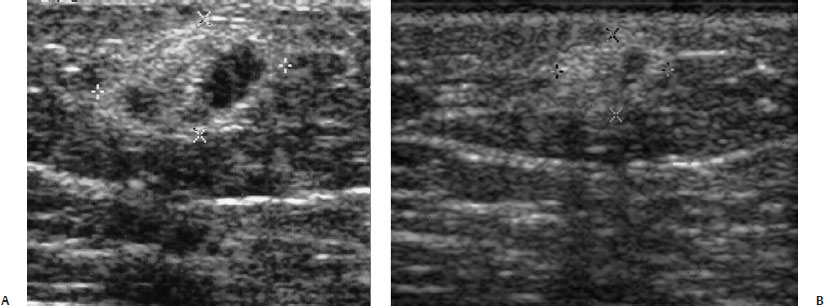
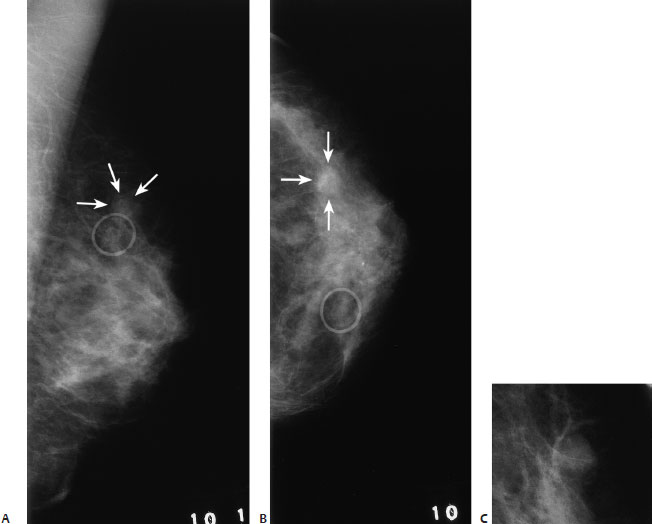
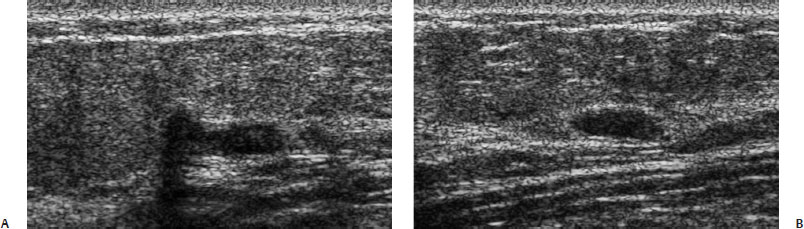
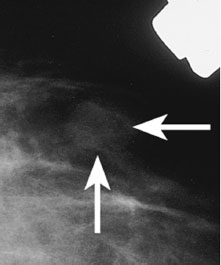
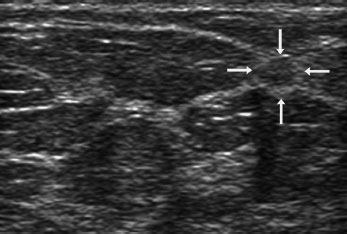
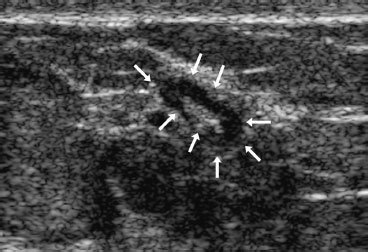
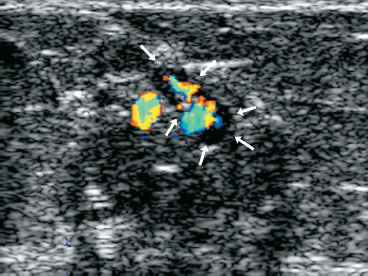
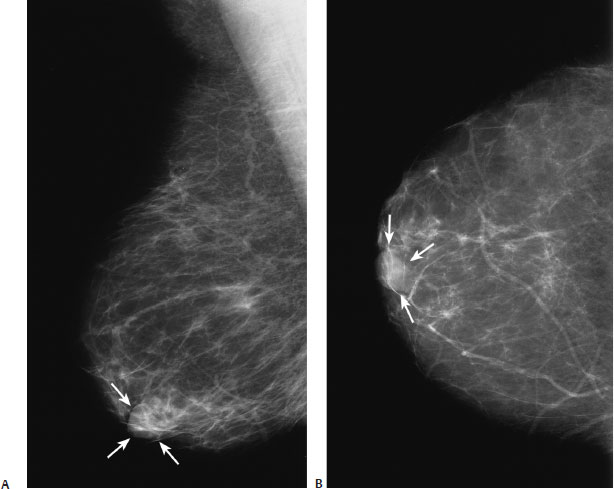
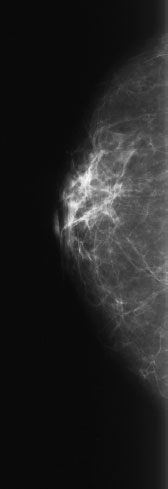
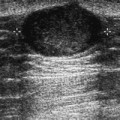
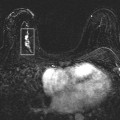
6 Circumscribed Masses: Medium- or High-Density Masses A 68-year-old woman presents with a new mass on her left screening mammogram. • Normal exam Mass (Fig. 6.1) • Margin: circumscribed • Shape: oval • Density: equal density Fig. 6.1 At the 12 o’clock position of the left breast and the 3 o’clock position of the right breast, there are two oval masses (arrows). The spot compression views demonstrate that the margins of the right mass are well defined, and the margins of the left mass are ill defined. (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammo-gram. (D) Left CC mammogram. (E) Right CC spot compression mammogram. (F) Left CC spot compression mammogram. Frequency • 10 MHz • Margin: ill defined • Echogenicity: hyperechoic • Retrotumoral acoustic appearance: no shadowing • Shape: ellipsoid Fig. 6.2 Right radial breast sonogram. The right mammographic mass identified in Fig. 6.1 corresponds to an oval, well-defined, hyperechoic mass. Fig. 6.3 Left radial breast sonogram. The left mammographic mass identified in Fig. 6.1 corresponds to a hyperechoic mass similar to the right breast mass. • Angiolipoma • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Uniformly hyperechoic sonographic masses are generally benign, but the category 4 (suspicious) assessment is based upon the information that the masses are new and the left mass is mildly ill-defined mammographically. • Clinically, angiolipomas resemble lipomas. Over 75% of patients are older than 50 years. Angiolipomas in other sites of the body generally are associated with pain. However, breast angiolipomas are generally painless. Microscopically, the mass consists of mature lipocytes associated with an extensive vascular network. Microthrombi are a prominent feature of the lesion. This mass is benign and does not recur. Brown RW, Bhathal PS, Scott PR. Multiple bilateral angiolipomas of the breast: a case report. Aust N Z J Surg 1982;52:614–616 Fleishman JS, Schwartz RA. Angiolipoma presenting as a breast mass. Ariz Med 1980;37:403–404 Sibala JL, Chang CH, Lin F, Thomas JH. CT of angiolipoma of the breast. AJR Am J Roentgenol 1980;134:840–841 A 43-year-old woman presents for screening mammogram. • Bilateral lumpy breasts; no new lumps Mass (Fig. 6.4) • Margin: circumscribed • Shape: oval • Density: equal density Fig. 6.4 In the upper outer quadrant of the right breast, there is an oval mass. Part of its margin is obscured by surrounding dense tissue, and part of the margin is associated with a lucent halo. (A) Right MLO mammogram. (B) Right CC mammogram. Frequency • 10 MHz Mass (Fig. 6.5) • Margin: well defined • Echogenicity: anechoic • Retrotumoral acoustic appearance: increased acoustic transmission • Shape: ellipsoid Fig. 6.5 Right radial breast sonogram. The mass identified in Fig. 6.4 corresponds to a simple cyst. The fluid collection is anechoic with increased acoustic transmission. • Cyst • BI-RADS assessment category 2, benign finding • Cysts are a component of fibrocystic change. This entity is considered a physiologic developmental process in which there is cystic dilatation of the terminal duct/lobular units. As a result of this origin, the cysts are lined either with epithelial-myoepithelial cells or by metaplastic apocrine cells. • Sonography is an excellent method to identify cysts and has been shown to accurately identify cysts in 96 to 100% of cases. As long as the wall of the cyst is well defined, thin, and hyperechoic, small moving particles within a cyst are generally not clinically significant. Azzopardi JGK. Problems in Breast Pathology. Philadelphia: WB Saunders; 1979:57–72 Hilton SV, Leopold GR, Olson LK, Willson SA. Real-time breast sonography: application in 300 consecutive patients. AJR Am J Roentgenol 1986;147:479–486 Jellins J, Kossoff G, Reeve TS. Detection and classification of liquid-filled masses in the breast by gray scale echography. Radiology 1977;125:205–212 Murad TM, Von Haam E. The ultrastructure of fibrocystic disease of the breast. Cancer 1968;22:587–600 Sickles EA, Filly RA, Callen PW. Benign breast lesions: ultra-sound detection and diagnosis. Radiology 1984;151:467–470 Tavassoli FA. Benign lesions. In: Tavassoli FA, Fattaneh A, eds. Pathology of the Breast. 2nd ed. Stamford: Appleton and Lange; 1999:115–204 A 51-year-old woman presents for screening mammogram. • Normal exam Mass (Fig. 6.6) • Margin: circumscribed • Shape: oval • Density: equal density Fig. 6.6 In the upper inner quadrant of the right breast, there are two dominant, well-defined oval masses. (A) Right MLO mammogram. (B) Right CC mammogram. Frequency • 11.5 MHz Mass (Fig. 6.7) • Margin: well defined • Echogenicity: anechoic • Retrotumoral acoustic appearance: increased acoustic transmission • Shape: ellipsoid Fig. 6.7 Right transverse breast sonogram. The two mammo-graphic masses correspond to two cysts. The fluid collections are anechoic; have well-defined, thin, hyperechoic walls; and have increased acoustic transmission. • Cysts • BI-RADS assessment category 2, benign finding • Cysts are a component of fibrocystic change. This process has been identified clinically in about one third of women between 20 and 45 years of age. Autopsy studies have found approximately 54% of normal breasts have histologic evidence of cystic changes. Frantz VK, Pickren JW, Melcher GW, Auchincloss H Jr. Incidence of chronic cystic disease in so-called normal breasts: a study based on 225 postmortem examinations. Cancer 1951;4:762–783 Jones BM, Bradbeer JW. The presentation and progress of macroscopic breast cysts. Br J Surg 1980;67:669–671 Leis HP Jr. Fibrocystic disease of the breast. J Med Assoc State Ala 1962;32:97–104 Leis HP Jr, Kwon CS. Fibrocystic disease of the breast. J Reprod Med 1979;22:291–296 Love SM, Gelman RS, Silen W. Sounding board. Fibrocystic “disease” of the breast—a nondisease? N Engl J Med 1982;307:1010–1014 A 48-year-old woman presents for screening mammogram. • No new breast lumps; both breasts normally lumpy Mass (Fig. 6.8) • Margin: circumscribed • Shape: oval • Density: equal density Fig. 6.8 In the left inferior inner quadrant, there is a circumscribed mass. This mass was new compared with previous exams. (A) Left MLO mammogram. (B) Left CC mammogram. (C) Left CC spot compression mammogram. Frequency • 7.5 MHz Mass (Fig. 6.9) • Margin: well defined • Echogenicity: heterogeneous • Retrotumoral acoustic appearance: bilateral edge shadowing • Shape: ellipsoid Fig. 6.9 Left longitudinal breast sonogram. The mammographic mass corresponds to a well-defined sonographic mass that is predominantly isoechoic to fat with a few anechoic oval lucencies within it. This mass was biopsied and found to be a complex benign cyst. • Cyst • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Sonography usually is successful in identifying benign cysts. However, occasionally, cysts exhibit internal echoes. These echoes may be caused by poor sonographic technique (e.g., gain settings too high), artifact (e.g., reverberation), proteinaceous debris, hemorrhage, infected debris, or cholesterol crystals. If the material completely moves, then the cyst is probably benign. However, if the material does not move, then an intracystic mass should be considered. In these cases, either aspiration or biopsy should be performed to identify intracystic tumors; 75% of solid intracystic masses are benign (mostly papillomas), 20% are malignant, and 5% are phyllodes tumors. Khaleghian R. Breast cysts: pitfalls in sonographic diagnosis. Australas Radiol 1993;37:192–194 Sohn C, Blohmer J-U, Hamper UM. Fibrocystic changes and breast cysts. In: Sohn C, Blohmer J-U, Hamper UM, eds. Breast Ultrasound. New York: Thieme; 1999:75–90 Stavros AT, Dennis MA. The ultrasound of breast pathology. In: Parker SH, Jobe WE, eds. Percutaneous Breast Biopsy. New York: Raven Press; 1993:111–127 A 32-year-old woman presents with a new left breast lump. She is diabetic and has been insulin dependent since childhood. • Left breast: large hard mass at the 3 o’clock position • Right breast: normal exam Mass (Fig. 6.10) • Margin: circumscribed • Shape: oval • Density: high density Fig. 6.10 In the 3 o’clock to 4 o’clock position of the left breast, there is a circumscribed oval mass that corresponds to the palpable mass designated by the metallic marker. (A) Left MLO mammogram. (B) Left CC mammogram. Low Frequency Frequency • 8 MHz Mass (Fig. 6.11) • Margin: ill defined • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: severe shadowing, mass completely obscured • Shape: irregular Fig. 6.11 Low-frequency left radial breast sonogram. (Same mass as Fig. 6.12.) As the frequency decreases, the mass attenuates the sound less, so the internal details of the mass become more apparent. The mass has a predominantly hyperechoic periphery with multiple linear lucencies centrally. Fig. 6.12 High-frequency left radial breast sonogram. With high frequency, the palpable mass attenuates the sound so only a heavily shadowing area is evident. High Frequency Frequency • 13 MHz Associated Findings • Lower frequency is more informative than high frequency for masses that severely attenuate sound because the internal architecture of the shadowing lesion is better displayed with the lower frequency (Fig. 6.11). • With high frequency, the palpable mass attenuates the sound so only a heavily shadowing area is evident (Fig. 6.12). • Diabetic mastopathy • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Occasionally, diabetes will affect the breast, causing diabetic mastopathy. Microscopically, diabetic mastopathy consists of perivasculitis, keloidlike fibrosis, and ductitis or lobulitis. Clinically, this abnormality presents as a hard breast mass. The palpable mass cannot be distinguished from malignancy. However, this presentation in a young woman who has had long-term insulin dependence should be a strong clue to the diagnosis. • The mammographic findings of diabetic mastopathy include a diffusely dense breast, asymmetric focal density, an irregular mass, and less commonly a circumscribed mass. • Sonographically, the fibrosis strongly attenuates sound, so usually only shadowing is evident. With very low frequencies, the internal architecture of the mass is identified. Boullu S, Andrac L, Piana L, Darmon P, Dutour A, Oliver C. Diabetic mastopathy, complication of type 1 diabetes mellitus: report of two cases and a review of the literature. Diabetes Metab 1998;24:448–454 Byrd BF Jr, Hartmann WH, Graham LS, Hogle HH. Mastopathy in insulin-dependent diabetics. Ann Surg 1987;205:529–532 Hunfeld KP, Bässler R. Lymphocytic mastitis and fibrosis of the breast in long-standing insulin-dependent diabetics: a histopathologic study on diabetic mastopathy and report of ten cases. Gen Diagn Pathol 1997;143:49–58 Pluchinotta AM, Talenti E, Lodovichetti G, Tiso E, Biral M. Diabetic fibrous breast disease: a clinical entity that mimics cancer. Eur J Surg Oncol 1995;21:207–209 Seidman JD, Schnaper LA, Phillips LE. Mastopathy in insulin-requiring diabetes mellitus. Hum Pathol 1994;25:819–824 A 40-year-old woman presents with a palpable left breast lump. • Left breast: palpable lump in left lateral breast • Right breast: normal exam Mass (Fig. 6.13) • Margin: well defined • Shape: oval • Density: equal Fig. 6.13 At the 3 o’clock position of the left breast, there is an oval mass (arrows). The spot compression view demonstrates that the mass has well-defined margins and a lucent halo around part of the border. (A) Left MLO mammogram. (B) Left CC mammogram. (C) Left MLO spot compression mammogram. Frequency • 10 MHz Mass (Fig. 6.14) • Margin: well defined • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: no shadowing • Shape: oval Fig. 6.14 Left radial breast sonogram. The oval mammographic density identified in Fig. 6.13 corresponds to a well-defined, hypoechoic solid mass. • Fibroadenoma • BI-RADS assessment category 3, probably benign; short-interval follow-up • Sonographically, if the mass has a well-defined margin, a hyperechoic, thin capsule, and no shadowing and is also homogeneously hypoechoic, then the chances of malignancy are very low (< 5%). Even though this lump was palpable, we chose short term follow up since the mass appeared sonographically to probably be benign. Cole-Beuglet C, Soriano RZ, Kurtz AB, Goldberg BB. Fibroadenoma of the breast: sonomammography correlated with pathology in 122 patients. AJR Am J Roentgenol 1983;140:369–375 Fornage BD, Lorigan JG, Andry E. Fibroadenoma of the breast: sonographic appearance. Radiology 1989;172:671–675 Jackson VP, Rothschild PA, Kreipke DL, Mail JT, Holden RW. The spectrum of sonographic findings of fibroadenoma of the breast. Invest Radiol 1986;21:34–40 Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology 1995;196:123–134 A 48-year-old woman presents with a new palpable right lump. • Right breast: palpable lump at the 10 o’clock position • Left breast: normal exam Mass (Fig. 6.15) • Margin: obscured • Shape: oval • Density: equal density Fig. 6.15 In the right upper outer quadrant, there is an oval mass (arrow) with obscured margins, which corresponds to the palpable lump demarcated with a metallic marker. (A) Right MLO mammogram. (B) Right CC mammogram. Frequency • 13 MHz Mass (Fig. 6.16) • Margin: well defined • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: single edge shadowing • Shape: lobulated Fig. 6.16 Right antiradial breast sonogram. At the 10 o’clock position, there is a hypoechoic, lobulated mass that corresponds to the mass identified in Fig. 6.15. • Fibrocystic changes • Stromal hyalinization, microscopic cysts, and apocrine metaplasia • BI-RADS assessment category 4, suspicious; biopsy should be considered. • In retrospect, the sonographic appearance of the mass correlates well with the histology as small cysts are evident within the lesion. • Fibrocystic changes generally cause symptoms in premenopausal women. About 75% of affected women are in the fourth or fifth decade. Three clinical stages have been described. Initially, women note premenstrual breast swelling or pain. Later, they develop breast lumps. Finally, the period of breast tenderness becomes continuous throughout the menstrual cycle. After menopause, the symptoms wane. Although at autopsy 25% of women have fibrocystic changes, only 10% of women older than 60 years have symptoms. Leis HP Jr, Kwon CS. Fibrocystic disease of the breast. J Reprod Med 1979;22:291–296 Tavassoli FA. Benign lesions. In: Tavasolli FA, Fattaneh A, eds. Pathology of the Breast. 2nd ed. Stamford: Appleton and Lange; 1999:115–204 Vorherr H. Fibrocystic breast disease: pathophysiology, patho-morphology, clinical picture, and management. Am J Obstet Gynecol 1986;154:161–179 A 65-year-old woman presents for her first mammogram. • Normal exam Mass (Fig. 6.17) • Margin: circumscribed • Shape: oval • Density: equal density Fig. 6.17 In the inferior medial left breast, there is an oval mass with a single round calcification. The spot compression view suggests that the margins are ill defined. (A) Left MLO mammogram. (B) Left CC mammogram. (C) Left MLO spot compression mammogram. Frequency • 7.5 MHz Mass (Fig. 6.18) • Margin: well defined • Echogenicity: heterogeneous • Retrotumoral acoustic appearance: posterior shadowing distal to mass • Shape: ellipsoid Fig. 6.18 Left radial breast sonogram. At the 8 o’clock position of the left breast there is a well-defined oval mass of heterogeneous (predominantly hyperechoic) echogenicity. • Fibrocystic change • Hyalin sclerosis (fibrosis) • BI-RADS assessment category 4, suspicious; biopsy should be considered. • The recommendation for biopsy is based on the mildly ill-defined mammographic margins and the mildly heterogeneous sonographic echogenicity. • When fibrocystic changes produce a circumscribed mammographic mass, the sonographic findings correspond to either a cyst or a focal solid mass. The sonographic appearance of a solid mass is variable and biopsy is generally required. The sonographic fibrocystic masses may be either well or ill defined. They may be hyperechoic, hypoechoic, or heterogeneous echogenicity. Love SM, Gelman RS, Silen W. Sounding board. Fibrocystic “disease” of the breast—a nondisease? N Engl J Med 1982;307:1010–1014 Teboul M, Halliwell M. Atlas of Ultrasound and Ductal Echography of the Breast, 2nd ed. Cambridge: Blackwell Science; 1996:106–110, 180–185 Tohno D, Cosgrove DO, Sloane JP. Benign breast change. In: Tohno D, Cosgrove DO, Sloane JP, eds. Ultrasound Diagnosis of Breast Diseases. New York: Churchill Livingstone, 1996:121–130 A 53-year-old woman presents with a new area of bruising in the right upper breast. She does not remember any trauma. She feels a lump under the bruise. • Right breast: ecchymosis associated with a palpable nodule in the upper breast at approximately the 12 o’clock position • Left breast: normal exam Mass (Fig. 6.19) • Margin: circumscribed • Shape: lobular • Density: equal density Fig. 6.19 At the 12 o’clock position of the right breast, there is a lobulated density. (A) Right MLO mammogram. (B) Right CC mammogram. (C) Right CC spot compression mammogram. Frequency • 7 MHz Mass (Fig. 6.20) • Margin: well defined • Echogenicity: heterogeneous • Retrotumoral acoustic appearance: bilateral edge shadowing • Shape: ellipsoid Fig. 6.20 (A) Right radial breast sonogram. The mammographic density identified in Fig. 6.19 corresponds to an oval mass of heterogeneous echogenicity with a hyperechoic rim. (B) Right radial breast sonogram. One month after the sonogram performed in A, the sono-graphic mass is smaller and has changed in appearance to an oval, predominantly hyperechoic mass. This change in size and appearance is consistent with a healing hematoma. • Hematoma • BI-RADS assessment category 3, probably benign; short-interval follow-up • Mammographically, acute hematomas are ill-defined or, less frequently, well-defined masses. As the hematoma resolves, a seroma or oil cyst may form, producing a well-defined round or oval mass. Finally, as the hematoma becomes fibrotic, the scar produces an irregular density or architectural distortion. The diagnosis of a breast hematoma rarely requires imaging, because there is usually a clear history of trauma or surgery. In this case, a mammogram 2 years later demonstrates complete resolution of the hematoma. • Sonographically, hematomas are uniformly hypoechoic or mixed echogenicity. They should demonstrate no internal flow with color Doppler and should decrease in size on subsequent exams. Harlow CL, Schackmuth EM, Bregman PS, Zeligman BE, Coffin CT. Sonographic detection of hematomas and fluid after imaging guided core breast biopsy. J Ultrasound Med 1994;13:877–882 Stigers KB, King JG, Davey DD, Stelling CB. Abnormalities of the breast caused by biopsy: spectrum of mammographic findings. AJR Am J Roentgenol 1991;156:287–291 A 67-year-old woman presents with an enlarging left breast mass. • Left breast: multiple stable lumps; enlarging mass cannot be palpated • Right breast: normal exam Mass (Fig. 6.21) • Margin: obscured • Shape: oval • Density: equal density Fig. 6.21 In the left upper outer quadrant, there is an oval mass (arrows) with obscured margins. The radiopaque circle and dot markers denote a skin lesion in the upper inner breast. (A) Left MLO mammogram. (B) Left CC mammogram. (C) Left MLO spot compression mammogram. Frequency • 13 MHz Mass (Fig. 6.22) • Margin: well defined • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: single edge shadowing • Shape: lobulated Fig. 6.22 The mammographic mass identified in Fig. 6.21 corresponds sonographically to a well-defined, lobulated, hypoechoic mass. (A) Left radial breast sonogram. (B) Left antiradial breast sonogram. • Leiomyoma • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Leiomyomas (smooth muscle) of the breast are extremely rare. They originate from the nipple or subareolar region, or within the breast parenchyma. They present as well-defined solid masses. In this case, the management assessment is based on the progressive growth of the lesion and the inability to mammographically display well-defined margins. Diaz-Arias AA, Hurt MA, Loy TS, Seeger RM, Bickel JT. Leiomyoma of the breast. Hum Pathol 1989;20:396–399 Nascimento AG, Karas M, Rosen PP, Caron AG. Leiomyoma of the nipple. Am J Surg Pathol 1979;3:151–154 Tavassoli FA. Mesenchymal lesions. In: Tavasolli FA, Fattaneh A, eds. Pathology of the Breast. 2nd ed. Stamford: Appleton and Lange; 1999:675–729 A 48-year-old woman presents for screening mammogram. • Normal exam Mass (Fig. 6.23) • Margin: circumscribed • Shape: oval • Density: equal density Fig. 6.23 Left CC spot compression mammogram. In the outer breast, there is an oval mass (arrows). Low Frequency Frequency • 7.5 MHz Mass (Fig. 6.24) • Margin: well defined • Echogenicity: heterogeneous • Retrotumoral acoustic appearance: single edge shadowing • Shape: ellipsoid Fig. 6.24 Left radial breast sonogram. Using a lower-frequency transducer, the mass (arrows) is difficult to identify. Frequency • 11.5 MHz Associated Findings In this case, a benign mass is originally missed with the lower-frequency examination. The mass is missed for two reasons: (1) the echogenicity of the mass matches the surrounding tissues because the dynamic range of the imaging program is too high, and (2) the internal architecture of the mass cannot be resolved due to poor resolution from the lower frequency. The higher-frequency study not only localizes the mammographic mass but also clearly identifies the benign nature of the mass (Figs. 6.25 and 6.26). Fig. 6.25 Left antiradial breast sonogram. Higher-frequency examination of the same area as Fig. 6.24 demonstrates that the mammographic mass is a normal lymph node (arrows). Fig. 6.26 Left antiradial color Doppler breast sonogram. Color flow high-frequency images confirm the normal pattern of blood flow through the center of the lymph node (arrows). • Lymph node • BI-RADS assessment category 2, benign finding • Masses may be missed with lower-frequency sonography because the lower resolution provides fewer visual clues to characterize masses. In this case, the hyperechoic center of the lymph node could not be identified with the lower frequency. Leucht D, Madjar H. Axillary, supraclavicular and infraclavicular lymph nodes. In: Leucht D, ed. Teaching Atlas of Breast Ultrasound. New York: Thieme; 1996:181–188 Sohn C, Blohmer J-U, Hamper UM. Sonography of the axilla. In: Sohn C, Blohmer J-U, Hamper UM, eds. Breast Ultrasound. New York: Thieme; 1999:94–97 A 53-year-old woman presents for screening mammogram. • Normal exam Mass (Figs. 6.27 and 6.28) • Margin: indistinct • Shape: oval • Density: equal density Fig. 6.27 In the subareolar region, there is an oval density (arrows). (A) Right MLO mammogram. (B) Right CC mammogram. Fig. 6.28 Right CC nipple profile mammogram. The oval density corresponds to the nipple. • Nipple • BI-RADS assessment category 2, benign finding
Case 6.1: Benign—Angiolipoma
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.2: Benign—Cyst
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.3: Benign—Cyst
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.4: Benign—Cyst
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.5: Benign—Diabetic Fibrous Mastopathy
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.6: Fibrodenoma
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.7: Benign—Fibrocystic Change
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.8: Benign—Fibrocystic Change
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.9: Benign—Hematoma
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.10: Benign—Leiomyoma
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.11: Benign—Lymph Node
Case History
Physical Examination
Mammogram
Ultrasound
High Frequency
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 6.12: Benign—Nipple Out of Profile
Case History
Physical Examination
Mammogram
Pathology
Management
Pearls and Pitfalls
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine