Factor 1
Factor 2
Factor 3
Factor 4
Hyperalgesia signs (0.75)
Temperature asymmetry symptoms (0.68)
Edema signs (0.69)
Decreased range of motion signs (0.81)
Hyperesthesia symptoms (0.78)
Color change signs (0.67)
Sweating asymmetry signs (0.62)
Decreased range of motion symptoms (0.77)
Allodynic signs (0.44)
Color change symptoms (0.52)
Edema symptoms (0.61)
Motor dysfunction signs (0.77)
Motor dysfunction symptoms (0.61)
Tropic symptoms (0.52)
Trophic signs (0.51)
The fundamental signs and symptoms of CRPS entail sensory, motor, autonomic, and trophic changes. The IASP requires that these clinical features be identified under these four categories. No supportive clinical tests are included in the IASP classification. However, tests of sudomotor dysfunction, e.g., the quantitative sudomotor axon reflex test (QSART), quantitative sensory testing (QST), skin biopsy, and the use of sympathetic blocks to determine whether any significant autonomic dysfunction is evident, can be undertaken.
The differential diagnosis of CRPS requires the elimination of other clinical syndromes which share clinical features with CRPS but which are clearly distinct by virtue of their own unique constellation of signs and symptoms. Clinical features similar to those of CRPS include the pain, edema, and temperature asymmetry characteristic of trauma patients, but who nevertheless do not develop CRPS. Table 44.2 describes the clinical diagnostic criteria of CRPS, termed the “Budapest Criteria” and published in 2010.
Table 44.2
Budapest clinical diagnostic criteria for complex regional pain syndrome (CRPS)
1. Continuing pain, which is disproportionate to any inciting event |
2. Must report at least one symptom in three of the four following categories: |
Sensory: reports of hyperesthesia and/or allodynia |
Vasomotor: reports of temperature asymmetry and/or skin color changes and/or skin color asymmetry |
Sudomotor/edema: reports of edema and/or sweating changes and/or sweating asymmetry |
Motor/trophic: reports of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin) |
3. Must display at least one sign at time of evaluation in two or more of the following categories: |
Sensory: evidence of hyperalgesia (to pinprick) and/or allodynia (to light touch and/or deep somatic pressure and/or joint movement) |
Vasomotor: evidence of temperature asymmetry and/or skin color changes and/or asymmetry |
Sudomotor/edema: evidence of edema and/or sweating changes and/or sweating asymmetry |
Motor/trophic: evidence of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin) |
4. There is no other diagnosis that better explains the signs and symptoms |
Movement disorders, not previously associated with CRPS, are now well recognized (see Table 44.3) [8]. They include weakness, tremor, muscle spasms, dystonia, and inability to initiate movement. Occasionally sympathetic blockade, when undertaken soon after the onset of CRPS, may eliminate the movement disorder.
Table 44.3
Prevalence of movement disorders in complex regional pain syndrome (CRPS)
N | Weakness (%) | Akinesia (%) | Dystonia (%) | Spasms (%) | Tremor (%) | Reference |
|---|---|---|---|---|---|---|
200 | 22 | Schwartzman and Kerrigan (1990) | ||||
829 | 95 | 36a | 25 | 49 | Veldman et al. (1993) | |
181 | 89 | 80 | 45 | Blumberg and Jänig (1994) | ||
123 | 75/76b | 24/94b | Harden et al. (1999) | |||
145 | 79 | 45 | 30c | 48 | Birklein et al. (2000) |
Contemporary thinking accepts that the initial clinical features of CRPS resemble a significant inflammatory disorder. However, this thinking has been shaped by studies revealing that free O2 radical expression can sensitize activity in C and A-δ fibers. Continuous excitation of these nociceptors will in turn sensitize first-order and higher neurons in the central nervous system (CNS). Central sensitization can be demonstrated not only in the spinal cord but also at the supratentorial centers in the brain [9].
Rationale for the Use of Neurostimulation
Most pharmacologic treatments of CRPS target neurologic dysfunction. The treatments include membrane stabilizers, antidepressants, norepinephrine reuptake inhibitors, and NMDA antagonists—all of which are used to support a return of function by means of physiotherapeutic measures [10]. Two other measures used to support rehabilitation are (1) epidural infusions of local anesthetics with or without opioids and (2) the addition of alpha-2 agonists like clonidine. These techniques have proved very effective but are associated with a low incidence of infection as well as technical failure of the infusion system. They are also expensive because they require home health-care support and associated pharmaceuticals.
When sympathetically maintained pain (SMP) has been demonstrated by a sympathetic block, with almost complete symptomatic relief, a comparatively long duration of effect can be achieved by segmental radio frequency ablation (RFA) of the sympathetic trunk.
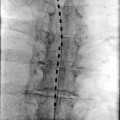
Increasing evidence now supports the use of neuroaugmentative procedures such as spinal cord stimulation (SCS) or peripheral nerve stimulation (PNS) [11–13]. This evidence includes randomized controlled trials (RCTs), several long-term studies, and several case studies. The first RCT, conducted by Kemler et al., was published in 2000 [14]. The patients in this study met the IASP diagnostic criteria for CRPS and were unresponsive to conventional medical management (CMM). Two randomly assigned groups comprised patients who undertook spinal cord stimulation (SCS) plus physical therapy and patients who received only physical therapy. All patients who successfully completed their trial underwent implantation of the neurostimulator. The subsequent intention-to-treat analysis demonstrated a significant reduction in pain in the SCS/physical therapy group [15]. Other measures showed that the SCS/physical therapy group experienced improvement both in the global perceived effect (GPE) and in quality of life (QOL). All patients underwent implantation of their SCS. The same authors demonstrated long-term improvement in pain relief and GPE among the SCS/physical therapy group, in comparison to the patients who received only physical therapy at 2 years. At 5 years, the GPE remained better than in patients who had received only physical therapy, although the “expressed” pain relief did not differ between the two groups. However, all the patients who had received an SCS stated they would repeat the treatment should the need arise.
In one study, carbamazepine and morphine were compared in patients previously implanted with an SCS [16]. This study, divided into two phases, investigated the effect of administering carbamazepine or placebo in phase I and morphine and placebo in phase II after the patient’s SCS system had been deactivated. Carbamazepine was superior to morphine in reducing the level of pain. However, only 2 of the 38 patients preferred to continue their treatment with carbamazepine; the remaining 36 preferred to continue their treatment with SCS. These results clearly demonstrated the successful symptomatic management of either neuropathic pain or CRPS.
Although most of the papers during the past 35 years have been case studies or retrospective reviews, a common thread of success runs through these works. The latest publication that supports the use of SCS is probably the 2009 Health Technology Assessment report, issued by the National Institute for Health and Clinical Excellence (NICE). This report reviewed 6,000 citations, including 11 RCTs of neuropathic pain and eight of ischemic pain [17], and concluded that SCS effectively decreases chronic neuropathic pain, and the results are more effective than those of conventional medical management (CMM). With regard to cost containment, the incremental cost-effectiveness ratio (ICER) described a range of $25,000–$30,000 per quality-adjusted life year (QALY), and if based on device longevity of 4 years, these figures were reduced to $20,000 per QALY.
It should be emphasized that most of the data reported so far have been obtained with comparatively unsophisticated systems. However, the efficacy of SCS, and in particular its effect on CRPS, has been improved by means of more modern neurostimulation systems with computerized programming capabilities, multiple arrays, and dual or multiple electrode systems. When the results of these latest systems are carefully studied, it becomes clear that early intervention is responsible for a much greater success rate in reversing or suppressing the symptoms.
The temporary use of SCS to provide analgesia in support of a physiotherapeutic program or a more comprehensive interdisciplinary treatment program was advocated by Prager and Chang in 2000 [18]. In this study, the authors described a triple-lead (tripolar) system that was temporarily implanted, and an “extended trial” was used to facilitate exercise therapy. The system was retained for 4 weeks, and if the patient required further analgesia after that time, it was implanted. A second set of 16 patients, who had failed 4 weeks of comprehensive therapy, underwent permanent implant of SCS with continuing interdisciplinary treatment. Patients who no longer felt that SCS was necessary underwent explantation. Five of the original eight patients showed improvement in their symptoms sufficient to warrant removal of the system. The authors noted that SCS is a fairly inexpensive treatment compared to CMM or multiple sympathetic blocks. Finally, it should be noted that an implanted SCS lead with an externalized pulse generator could always be converted to a totally implanted system, circumstances prevailing.
Patient Selection
Appropriate selection of patients for SCS is essential to a successful outcome [11]. Most published treatment algorithms describe the use of SCS after simpler and more conservative therapies have been tried in a stepwise fashion although usually in support of an exercise therapy treatment program [19]. Conventional wisdom would suggest that any patient who is likely to need an implantable device such as an SCS must undergo a satisfactory behavioral assessment [20]. Such an assessment is essential for precluding those patients who might believe that a simple or rapid intervention such as SCS is most likely to cure their clinical problem, or who may have unrealistic expectations regarding the management of their syndrome. Although SCS is a minimally invasive procedure, it should always follow an adequate screening trial. The trial should demonstrate to the patient and to the treating physician that the activities of daily living (ADLs) can be improved and that notwithstanding improved symptoms, the patient should maintain their exercise therapy (Table 44.4).
Table 44.4
Selection criteria for spinal cord stimulation in complex regional pain syndrome (CRPS)
Oakley [11] | |
Inclusion | Exclusion |
Diagnosis of CRPS | Absence of initial CMM |
6-month pain duration | Previous failed SCS trial |
Psychological clearance | Untreated axis I psychiatric disorder |
Informed consent | Certain psychoses |
Contraindications | |
North et al. [21] | |
Relative | Absolute |
Medication dependence | Coagulopathy |
Unresolved psychiatric disorder | Immunosuppressive therapy |
Nonorganic signs (Waddell’s) | Unacceptable surgical risk |
Inconsistent history | Conflicting therapy diathermy |
Anticoagulation therapy | Serial MRI requirements |
Alternative therapy with lower risk/benefit ratio | Occupational risk |
In this respect, convention requires a 50 % reduction of pain. If other comorbidities, or the possible anatomic anomalies, are suggested, preradiologic screening with MRI or CT scan is imperative. Additional selection criteria have been developed by several authors (see Table 44.3). In an effort to standardize criteria for the selection of patients for SCS, several scientific bodies, including the International Association for the Study of Pain (IASP), the International Neuromodulation Society (INS), the North American Neuromodulation Society (NANS), and the American Academy of Pain Medicine (AAPM), are involved in the education and dissemination of guidelines to be met before patients are selected for neurostimulation. The requirement for psychological pretesting is addressed by the Centers for Medicare Services (CMS), the industrial commissions and state bureaus of workers compensation (BWC), and most health insurance agencies. Most contemporary psychological evaluation is based on an inventory of risk factors which, together with behavioral management, play a significant role in patient care that supports the use of SCS in selected patients [23, 24].
Risk–Benefit Analysis
The potential benefit of SCS as a treatment modality for CRPS has been described in the supporting literature. Table 44.5 identifies several observations that underscore the value of SCS; however, pain relief remains the most significant reason to consider SCS. For more than 30 years, success has been defined as a reduction of 50 % in pain [30]. However, pain reduction is subjective, and the level of pain is assessed by means of arithmetic scales such as the visual analog scale (VAS), verbal rating scale (VRS), and numerical rating scale (NRS). Unfortunately, because pain is subjective and is an exponential function, the values, expressed arithmetically, bear little resemblance to the constellation of symptoms about which the patient complains. Furthermore, chronicity and environmental factors materially impact the number chosen on any one of the above scales. Function should become the standard by which the impact of pain can influence a variety of functional markers (Table 44.5).
Table 44.5
Potential benefits of spinal cord stimulation in treating complex regional pain syndrome (CRPS)a