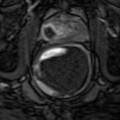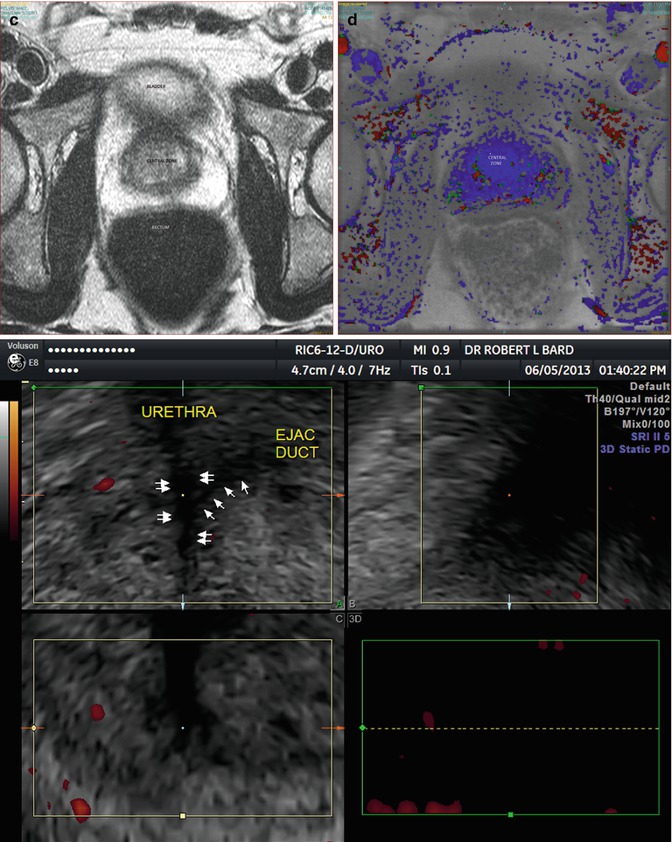
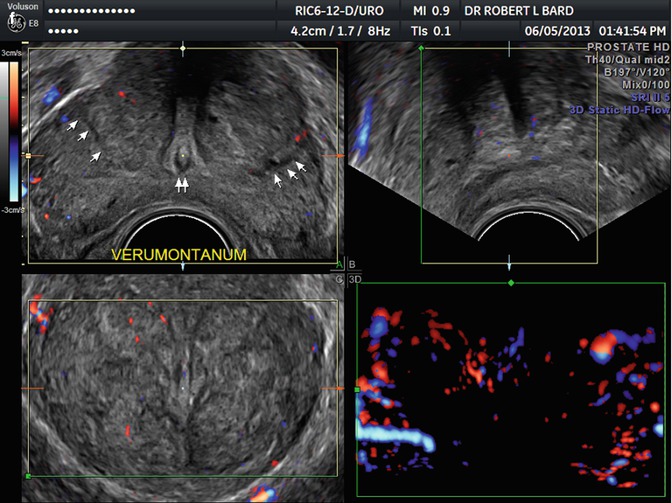
Fig. 12.1
(a) Sagittal plane. Base is cephalad between bladder and seminal vesicles. (b) Transverse plane. Central zone abuts bladder base. (c) Transverse plane. Peripheral zone (white). Bladder anterior to central zone (gray). (d) Transverse plane. Prostate homogeneously blue (no enhancement). (e) Urethra (double arrows) ejaculatory duct (arrows). (f) Verumontanum (double arrows) peripheral-central zone border (arrows)
The rectum is posterior to the prostate and separated by Denonvillier’s fascia in which part of the neurovascular plexus is located as it extends anterolaterally. For practical reasons of symmetry analysis, most images will be exhibited in the transverse sonographic plane and the transverse or axial MRI plane.
The urethra is centrally located within the longitudinal axis and receives the ejaculatory ducts in the midgland structure of the verumontanum. These areas are not imaged unless diseased.
The paired seminal vesicles and vas deferens ducts are located posterior and superior to the prostatic base. The seminal vesicles are readily imaged if ejaculation is postponed for 3 days (Fig. 12.2a–e).
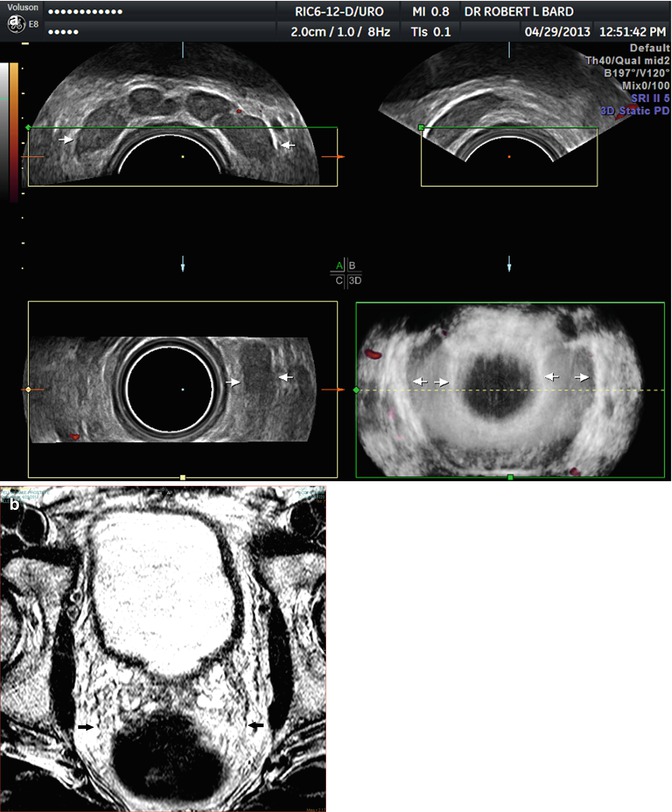
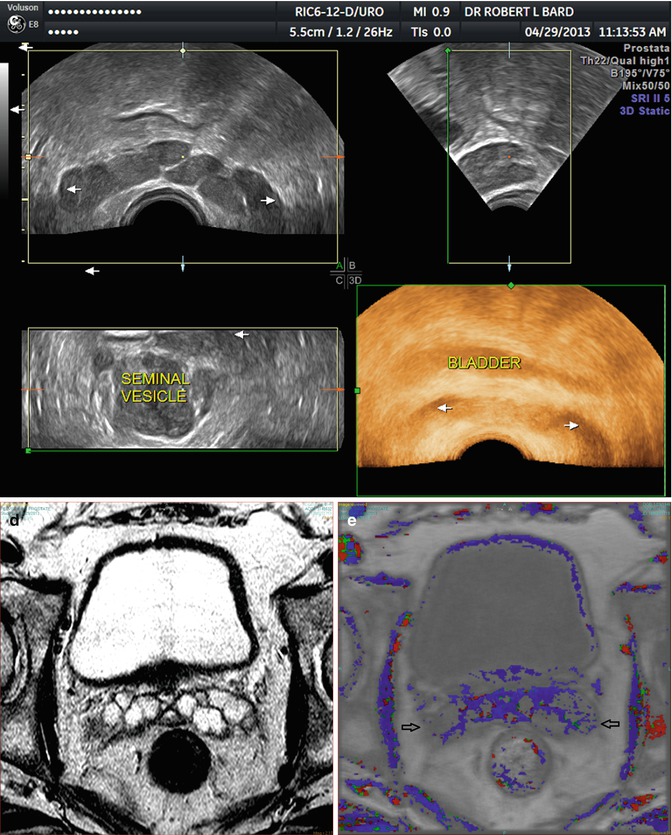
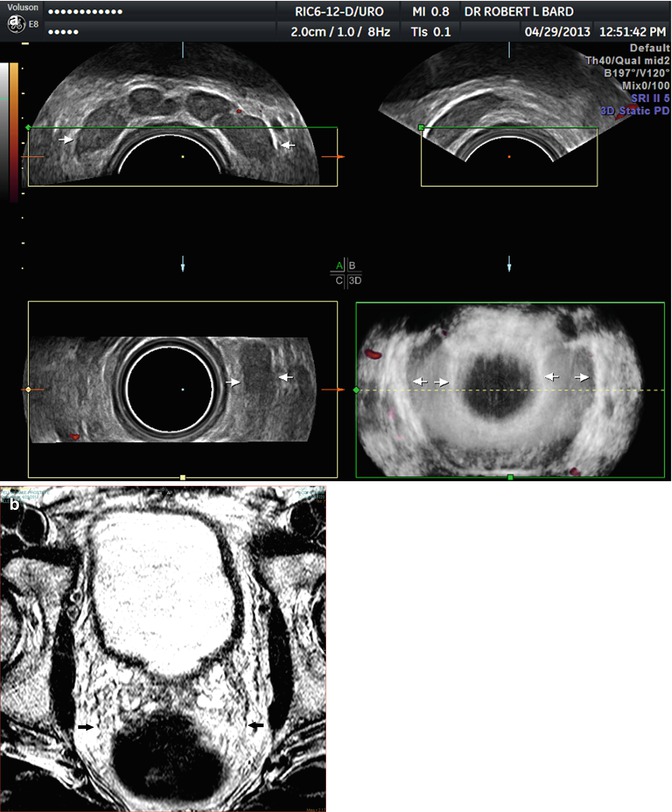
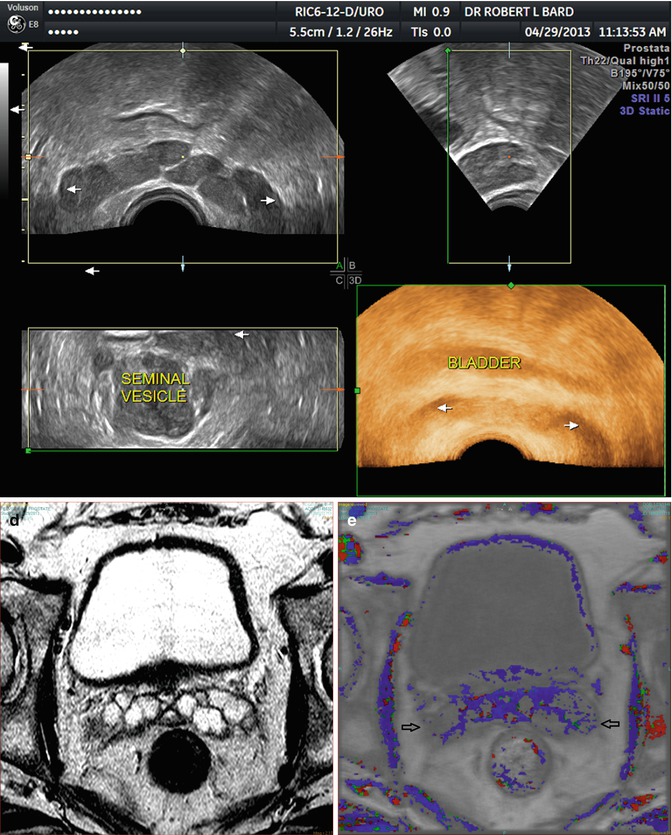
Fig. 12.2
(a) Transverse plane. Seminal vesicles (arrows). (b) Seminal vesicles between rectum (black) and bladder (white). (c) 3D image of seminal vesicles (3 orthogonal views + composite). (d) MRI. Septations in both seminal vesicles. (e) DCE-MRI. Scattered trace enhancement
12.2.2 Congenital Anomalies and Cysts
Congenital cysts are usually midline and thin-walled regions. Mullerian duct cysts are pear shaped and occur near the prostate base with the neck of the cyst extending to the verumontanum. In chronic cysts, the walls may thicken or calcify (Figs. 12.3a–c and 12.4a–d).
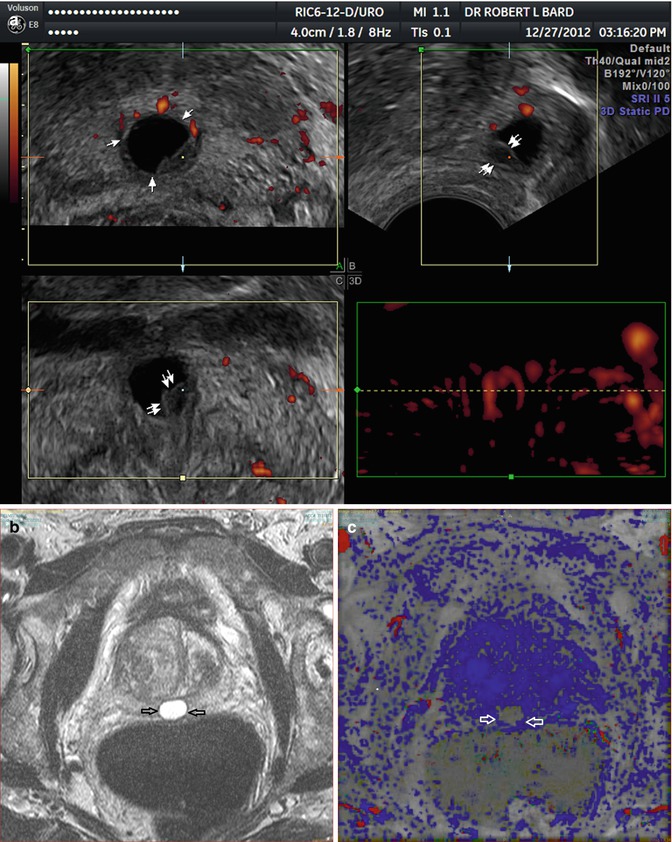
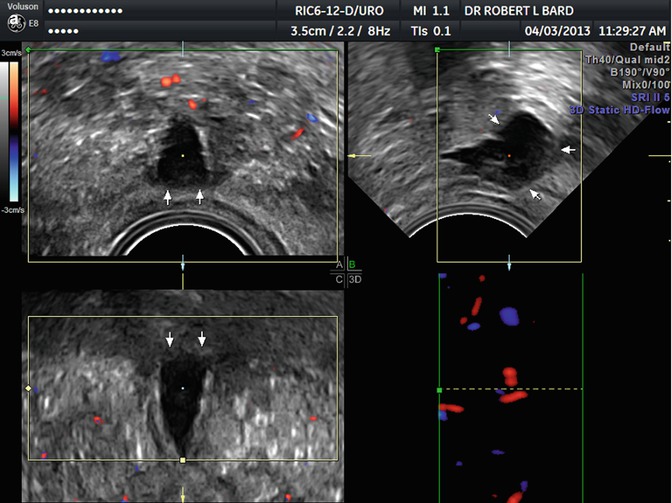
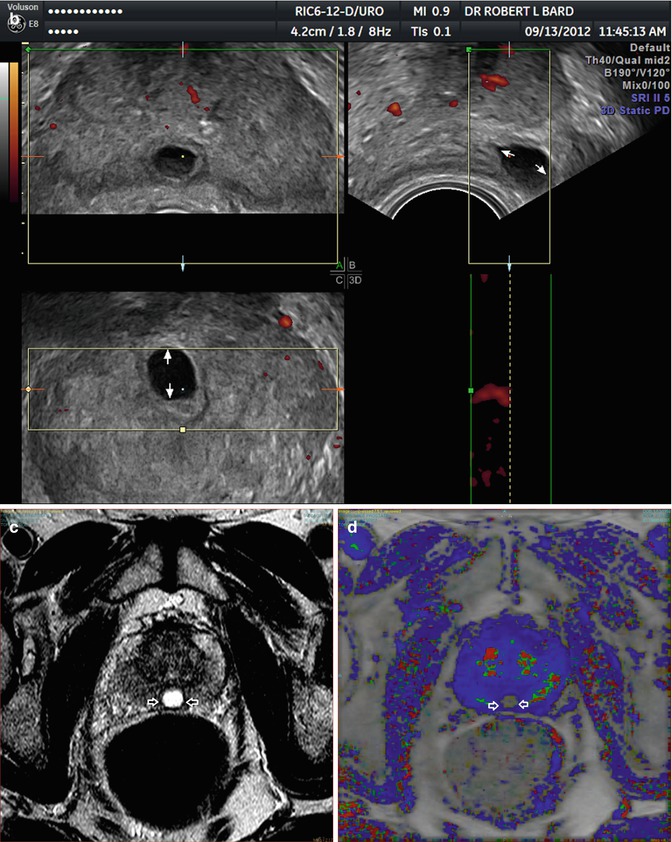
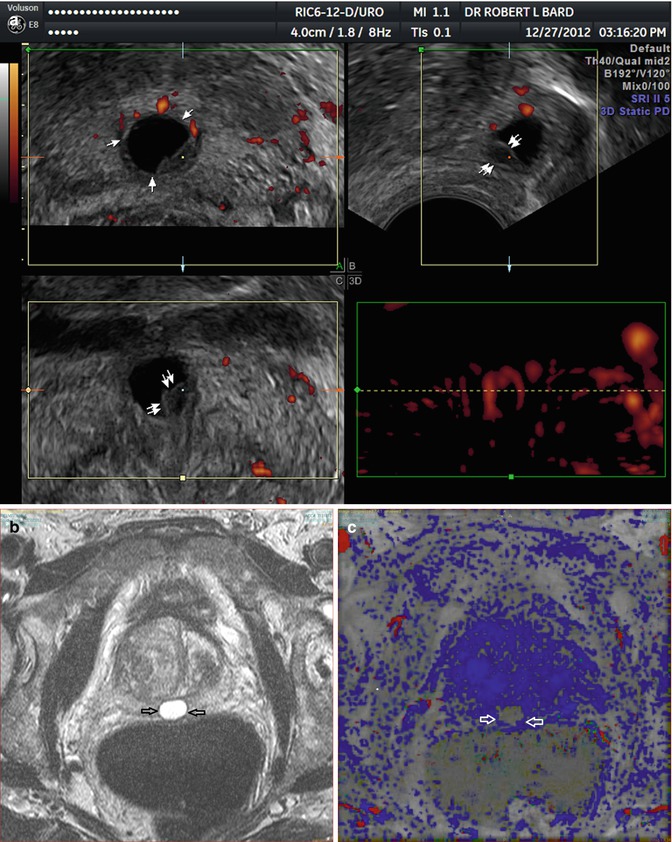
Fig. 12.3
(a) Midline cyst with solid wall elements. (b) MRI. Cyst (white) without wall irregularity. (c) DCE-MRI. No enhancement in cyst
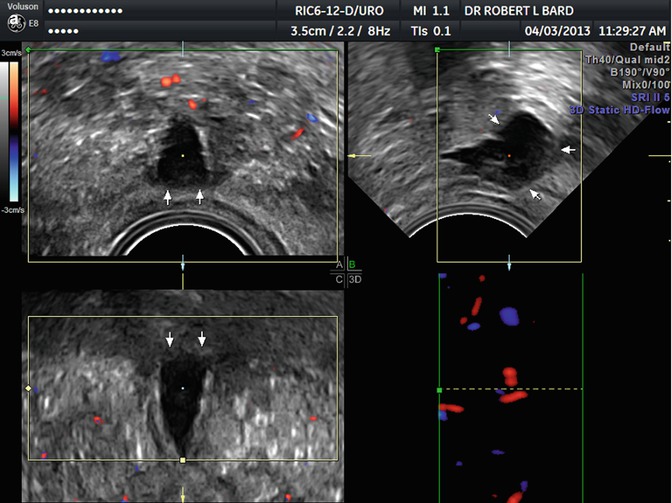
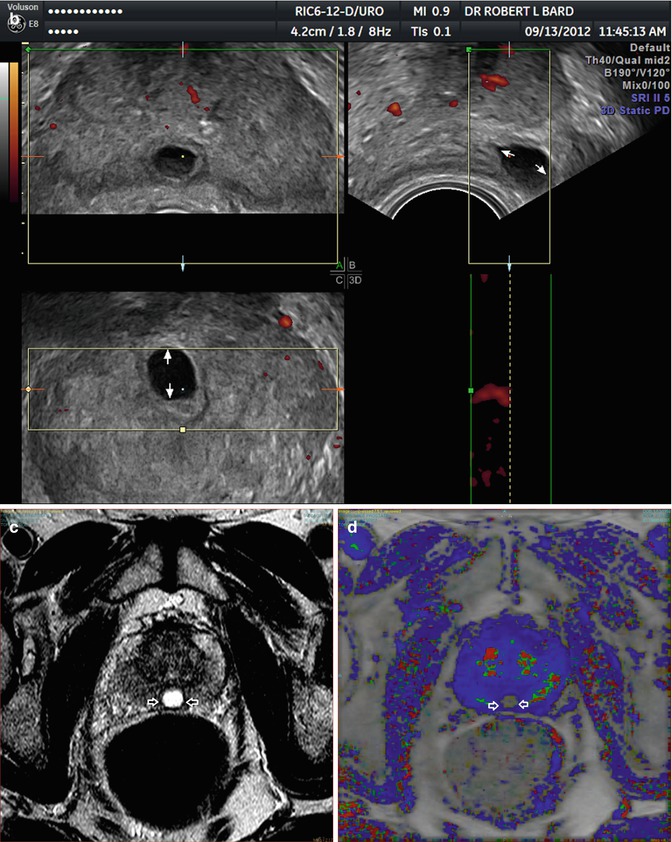
Fig. 12.4
(a) 3D. Pear-shaped nature of cyst. (b) 3D. Note thick cystic wall. (c) MRI. Well-marginated cyst. (d) DCE-MRI with no cyst enhancement
Ultrasound findings of a complex cyst wall may be missed by MRI. Utricle cysts or congenitally enlarged prostatic utricles are not true cysts although they are imaged as such and project from the posterior wall of the prostatic urethra as a diverticulum. This entity is associated with hypospadias and undescended testes allowing clinical differentiation of these cystic entities.
Ejaculatory cysts are diagnosed when the cystic areas are bilateral. Urethral diverticula, usually symptomatic in females, are difficult to distinguish from other cystic areas.
On occasion cysts can bleed producing internal echoes on US and T1 findings on MRI-chronic cysts may simulate tumors (Bard 2009).
Acquired cysts are the most common finding in older men. These are generally no larger than 10 mm and tend to be irregular in outline. These are usually off the midline, most common in the hyperplastic inner gland of benign prostatic hypertrophy and are not easily mistaken as congenital cysts (Landes and Ransom 1949). Rarely are periprostatic cysts noted on the periphery (Hamper et al. 1990).
12.2.3 Benign Prostatic Hypertrophy (BPH)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree