Introduction
Classification systems provide a common language through which physicians and researchers can communicate. They can help create a framework for standardized treatment algorithms through which surgeons can directly and reproducibly contribute to improvements in patient outcomes. In order for these algorithms to be generalized to the population, they must be clinically relevant, reliable, and validated. If measurements are involved as part of the tool for outcome prediction, there must be a standardized way to obtain such data in an accurate way: whether that be through specific language to determine landmarks, image acquisition, imaging modalities, etc. This chapter will explore some of the more commonly used classification systems used in the subaxial cervical spine, specifically, within the domains of the traumatic, degenerative, and stenotic spine. It will also examine the literature for assessment of their reliability, validation and, if present, their clinical impact with focus on standard health-related quality of life (HRQOL) measures and surgeon expert opinion parameters thought to be relevant for evaluating and predicting outcomes.
The Traumatic Subaxial Cervical Spine
Classification systems in the traumatic subaxial cervical spine encompass a broad spectrum of pathology. They can assist the provider in making a quick assessment of initial stability for emergency triage and ultimately, in working out a finalized treatment plan. This becomes critical for the patient when assessing initial neurologic injury, recovery potential, and surgical timing. Sadiqi et al. launched an international web-based survey to ascertain what parameters were thought to influence outcomes in patients with subaxial cervical spine trauma. They polled 279 AO Spine International and International Spinal Cord Society members and concluded that neurological status, implant failure within 3 months, and patient’s satisfaction were the most relevant parameters in the short and long term: bony fusion was the most relevant in the long term, and surgical site infection, spinal canal encroachment on advanced imaging, facet or lateral mass fracture on radiographs, and age were the most relevant in the short term. These parameters, along with HRQOL scores, will be the basis for examining clinical correlates for three of the most widely used classification systems for subaxial cervical spine trauma, the Allen and Ferguson Classification, the Subaxial Injury Classification and Severity Scale (SLICS), and the AO Spine Subaxial Cervical Spine Injury Classification System.
Allen and Ferguson Classification of Subaxial Cervical Spine Injury
Overview
The Allen and Ferguson Classification, proposed in 1982, is regarded as one of the first broadly used classification systems for subaxial cervical spine trauma. It is based on the biomechanical concepts that allow the mechanism of injury to be deduced from radiographic patterns via “injury vectors.” The following injury mechanisms make up the schema and are derived from the major injury vector involved: vertical compression, compressive flexion, compressive extension, lateral flexion, distractive flexion, and distractive extension. These injury vectors have a magnitude and produce a spectrum of injury, which the authors have termed, a phylogeny. Each phylogeny is made up of stages that denote a specific type and degree of injury to a cervical motion segment, and it was noted by the authors that these stages correlated well with neurologic status. An important point to this system is that it assumes an indirect injury mechanism; the assumption is that a direct injury mechanism (i.e., blow to the neck, and penetrating projectile) is biomechanically different and often causes a much less predictable pattern of injury that cannot readily be deduced. The classification system is simplified in the following:
- •
Vertical compression (VC): compressive loading of the entire vertebral centrum—as the severity of the vertebral body fracture increases, the incidence of vertebral arch fractures increases (16%, 25%, and 40% in stages 1, 2, and 3, respectively)
- •
VC Stage 1: fracture of a superior or inferior endplate with a cupping deformity
- •
VC Stage 2: fracture of both endplates with cupping. Sometimes associated with a nondisplaced or minimally displaced fracture through the centrum
- •
VC Stage 3: fracture of both endplates with a fragmented centrum
- •
Fragments are displaced peripherally and sometimes, into the neural canal
- •
- •
- •
Compressive flexion (CF): anterior compression and burst fracture variants—the occurrence of multiple contiguous CF lesions suggests a greater magnitude of force imparted to the anterior elements
- •
CF Stage 1: blunting of the anterior-superior vertebral margin to a rounded contour
- •
CF Stage 2: CF 1 changes and obliquity of the anterior vertebral body with loss of height at the centrum. May see a fracture through the centrum
- •
Resulting appearance is a “beaking” of the anterior-inferior vertebral body
- •
- •
CF Stage 3: CF 2 changes and a fracture line passing obliquely from the anterior surface of the vertebral body through the centrum and extending through the inferior subchondral plate
- •
The “beak” in CF 2 is fractured
- •
- •
CF Stage 4: CF 3 changes and less than 3 mm of displacement of the inferior-posterior vertebral margin into the neural canal
- •
CF Stage 5: CF 3 and gross displacement of the posterior portion of the vertebral body into the canal with signs of ligamentous failure
- •
Separation of the articular facets and increased distance between the spinous processes at the injury level indicating failure of at least the posterior portion of the anterior ligamentous complex and entirety of the posterior ligamentous complex
- •
- •
- •
Compressive extension (CE): posterior compression/vertebral arch injuries—the severity of anatomic damage does not correlate well with the severity of the spinal cord lesion
- •
CE Stage 1: unilateral vertebral arch fracture with or without anterorotary vertebral body displacement
- •
Linear fracture through the articular process, compression of the articular process, pedicle or lamina fracture, or a combination of the two
- •
Rotary listhesis of the centrum may occur
- •
- •
CE Stage 2: Bilaminar fractures
- •
Typically, at contiguous multiple levels
- •
- •
CE Stage 3: Bilateral vertebral arch fractures without displacement of the vertebral body
- •
CE Stage 4: CE Stage 3 with partial vertebral body displacement anteriorly
- •
CE Stage 3 and 4 are theoretical and were actually not encountered in this study
- •
- •
CE Stage 5: CE stage 3 with full vertebral body width displacement anteriorly
- •
Ligamentous failure occurs posteriorly between the above and fractured vertebra and anteriorly between the fractured and lower vertebra
- •
The anterior-superior portion of the centrum is characteristically sheared off by the anteriorly displaced centrum
- •
- •
- •
Lateral flexion (LF): asymmetric lateral compression injury of the centrum and ipsilateral vertebral arch with distraction of the contralateral vertebral arch—sometimes associated with occult “kissing compressive lesions” of the uncovertebral joint
- •
LF Stage 1: compression fracture on the centrum plus vertebral arch fracture on the ipsilateral side without displacement of the arch on the AP view
- •
LF Stage 2: LF Stage 1 with displacement of the arch on the AP view or ligamentous failure on the contralateral side with separation of the articular processes
- •
Both can occur simultaneously
- •
- •
- •
Distractive flexion (DF): spectrum of facet-displacing injury patterns—the degree of ligamentous failure is sequentially greater in each subsequent stage and this correlates well with neurologic status
- •
DF Stage 1: failure of the PLC as evidenced by subluxation of the facet in flexion with abnormally great divergence of the spinous processes at the injury level
- •
Can see blunting of the anterior-superior margin of the vertebra similar to CF 1
- •
- •
DF Stage 2: unilateral facet dislocation
- •
The range of ligamentous injury is variable and may require dynamic studies for full assessment
- •
Facet subluxation on the opposite side of the dislocation would suggest severe ligamentous injury
- •
- •
DF Stage 3: Bilateral facet dislocation with approximately 50% anterior displacement of the vertebral body
- •
DF Stage 4: DF Stage 3 with full vertebral body width displacement anteriorly or grossly unstable motion segment
- •
- •
Distractive extension (DE): anterior ligamentous failure with posterior vertebral displacement—frequently resulting from a fall and occurred more commonly in older age groups as compared to the other fractures and dislocations
- •
DE Stage 1: failure of the anterior ligamentous complex or a transverse nondeforming fracture of the centrum
- •
Abnormal widening of the disc space is a radiographic hint
- •
- •
DE Stage 2: DE Stage 1 with failure of the posterior ligamentous complex with displacement of the upper vertebral body posteriorly into the canal
- •
This type of displacement tends to reduce when the head is in neutral so radiographic hints may be subtle (often less than 3 mm).
- •
- •
Reliability and validation
Reliability of the classification system was not discussed in the initial manuscript by Allen and Ferguson but was explored separately in the literature. In the landmark manuscript by Vaccaro et al., reliability was assessed, along with the SLICS and Harris Scores, via surveys after 2 rounds of case presentations given to 20 members of the Spine Trauma Study Group (STSG). Because the Allen and Ferguson Classification system is nonordinal, it could not be assessed with intraclass correlation coefficient (ICC)—instead, it was assessed with Cohen’s kappa coefficient (compares qualitative items). As compared to the SLICS and Harris classification systems, the interrater and intrarater reliability scores were highest in the Allen and Ferguson system (Intrarater reliability: AF [0.63], SLICS [0.60], and Harris [0.53]; Interrater reliability: AF [0.53], SLICS [0.51], and Harris [0.41]). Validation efforts were also made in the SLICS manuscript whereby the SLIC score and its recommendation to the participant’s management recommendation were compared; raters agreed with the SLIC score algorithm in 91.8% of cases. They also compared the SLIC morphology domain and the Ferguson and Allen description of morphology with 71.5% agreement between the two systems.
Stone et al. assessed the reliability of the Cervical Spine Injury Severity Score (CSISS), SLICS, and Allen and Ferguson Classifications and found mixed results compared to some of the previous literature. Their team found that ICC values for CSISS and SLICS suggested excellent interobserver reliability. The kappa coefficient for Allen-Ferguson, however, suggested moderate to poor reliability, particularly when assessing the 6 main groups and all 21 groups, respectively. Urrutia et al. showed similarly poor interobserver reliability but substantial intraobserver reliability.
Clinical correlates
There are no studies in the literature prospectively implementing the Allen and Ferguson Classification to assess patient outcomes. Instead, these concepts served as a steppingstone for the generation of subsequent subaxial cervical spine classification systems. Harris et al. would expand on these ideas to produce their own classification system in 1986 that was followed by the Magerl classification in 1994. These classification systems, while providing significant contributions to the language associated with classifying spine fractures, were unable to be reliably used or clinically validated in the literature.
Subaxial Injury Classification and Severity Scale
Overview
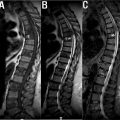
The Subaxial Injury Classification Scale (SLICS, Fig. 1 ) is one of the most readily used classification systems in the traumatic subaxial cervical spine. Its development consisted of expert opinions of a subgroup within the Spine Trauma Study Group (STSG) and the amalgamation of a thorough literature review for cervical trauma with previously obtained surveys used to establish what was believed to be the most important characteristics for defining these injuries. These surveys, previously used for thoracolumbar injuries, were thus adapted based on the literature search and developed into the current subaxial classification system. It was developed for the purpose of categorizing injuries in a standardized way and, at the time of its development, was the only classification attempting to predict treatment.

This system uses three previously generated critical characteristics for clinical decision making that were also found to be appropriate for the subaxial cervical spine—injury morphology (based on column disruption), integrity of the disco-ligamentous complex (DLC), and patient’s neurologic status. These characteristics can all be determined by traditional radiographic studies such as X-ray, CT, and MRI imaging. Each component within the three domains is given a numerical value (with 0 being normal) in an ascending manner based on presumed severity of outcome and/or necessity for requiring surgery. The point totals in the three domains are added such that higher point totals assume a more severe injury. A score of less than 4 would recommend for nonoperative treatment while a score greater than 4 would recommend for surgical intervention. The classification system is simplified in the following:
- •
Injury morphology
- •
Compression (1 point): includes compression, burst, flexion/compression (teardrop), and nondisplaced/minimally displaced lateral mass and facet fractures. The latter two only included if there is no visible translation between vertebral levels noted
- •
Burst patterns (2 points) are considered higher energy and therefore scored higher than traditional compression fractures
- •
- •
Distraction (3 points): includes anatomic dissociations in the vertical axis; hyperextension/hyperflexion injuries
- •
Signifies a more severe injury pattern due to the force required to overcome the protective forces (i.e., facet capsule in flexion, anterior longitudinal ligament in extension)
- •
Commonly involves ligamentous disruption traversing the disc space and facet joints, and therefore, MRI is useful for assessment
- •
- •
Translation/rotation (4 points): includes anatomic dissociations in the horizontal axis; unilateral/bilateral facet fracture-dislocations, fracture separation of the lateral mass, and bilateral pedicle fractures
- •
A relative angulation of ≥ 11 degrees implies displacement exceeding physiologic ranges
- •
- •
- •
DLC integrity
- •
Components include the intervertebral disc, anterior/posterior longitudinal ligaments, ligamentum flavum, interspinous/supraspinous ligaments, and facet capsules
- •
Indeterminant (1 point)
- •
T2 MRI imaging showing only hyperintense signal
- •
Isolated interspinous ligament widening
- •
- •
Indications of instability (2 points)
- •
Abnormal facet alignment (articular apposition < 50% or diastasis > 2 mm through facet joint)
- •
Abnormal widening of the disc space on either neutral or extension radiographs
- •
Horizontal signal intensity on T2 sagittal MRI through a disc involving the nucleus and annulus
- •
Subluxation of the vertebral bodies (i.e., translational/rotational abnormalities)
- •
- •
- •
Neurologic status
- •
Root (1 point) injury: implies lower energy mechanism and less likelihood for catastrophic neurologic disability
- •
Incomplete (3 points) vs complete (2 points): thought to warrant surgical intervention in the setting of ongoing compressive phenomenon in order to provide the patient’s highest likelihood of improvement and therefore receives the highest score
- •
Reliability and validation
Reliability was assessed via surveys after 2 rounds of case presentations given to 20 members of the STSG. Interrater and intrarater agreement were assessed by ICC scores of the morphology, DLC, and neurologic status, and compared with the same cases using the Allen and Ferguson and the Harris classifications. The interrater and intrarater reliability were variables among the three domains of the classification system; however, the overall reliability of the SLIC score was substantial with an interrater ICC of 0.71 and an intrarater ICC of 0.83. The interrater and intrarater reliability ICC for the SLIC management recommendations were moderate and substantial, respectively (ICC of 0.58 and 0.77). As compared to the other two aforementioned systems, the SLIC interrater and intrarater reliability scores were higher than the Harris system, but lower than the Ferguson and Allen system.
Validation of the system was determined by testing the assumption that SLICS would be able to morphologically characterize injuries and predict treatments and that the expert panel would gain consensus on treatment. This was done via internal testing by comparing the SLIC score and its recommendation to the participant’s management recommendation for the aforementioned cases. Raters agreed with the SLIC score management in 91.8% of cases. A comparison was also made between the SLIC morphology domain and the Ferguson and Allen description of morphology with 71.5% agreement between the two systems. The authors describe the reliability of this system as moderate and the validity as sufficient.
Separate external validation studies in the literature confer mostly positive results; however, there have been disagreements on the morphology domain of the system. Urrutia et al. published a study independently evaluating the reliability of the SLIC scale. They observed that the interobserver agreement was substantial when considering the main types and moderate when considering subtypes and the intraobserver agreement was substantial for both main and subtypes. Stone et al. and Lee et al., in separate studies, observed excellent and significant reliability, respectively. More recently, in a study published by van Middendorp et al., poor agreement on morphologic injury characteristics and no improvement in agreement among surgeons with the SLICS treatment algorithm were seen.
Clinical correlates
There is a paucity of literature attempting to ascertain outcomes based on the prospective application of the SLICS system. The first and only to do so was Joaquim et al. —in their study, they assessed neurologic status as the primary outcome of successful treatment; 48 patients were included. In the 23 patients treated nonoperatively (SLIC < 4), there was no neurological deterioration. There were 25 treated surgically (SLIC > 4); of those with incomplete deficits, 72% showed improvement in their American Spinal Injury Association (ASIA) score and no patient showed neurological worsening. As previously mentioned, neurologic status is one of the more relevant parameters in regard to short- and long-term outcome estimations. With these data in mind, the authors concluded that SLICS was both safe and efficacious in guiding surgical treatment for the parameter of neurologic status.
The information generated from the SLICS study was the spark for a plethora of new manuscripts with important clinical correlates. In one such study, Dvorak et al., using the SLICS scale as their basis, undertook a systematic review of the literature to create an evidence-based algorithm for subaxial cervical spine injury surgical approach; their approach algorithm was based on the three morphological domains of the SLICS study. The systematic review verified that for the burst morphology, an anterior approach w/ vertebral body resection and stabilization provides mechanical reconstitution of the motion segment, optimal decompression of the neural elements, and ample bone graft to reinforce the fusion. For distraction injuries, the surgical approach tends to be denoted by the pattern of DLC disruption—hyperextension injuries tend to be anterior and thus will require an anterior approach, hyperflexion injuries tend to be posterior, along with cases of severe spondylosis, DISH, or ankylosing spondylitis (these entities create long lever arms) and are thus best approached posteriorly. The exception to this rule is for facet subluxation, where the approach is determined based on disc herniation—posteriorly displaced disc herniation is preferentially treated anteriorly, if there is no disc herniation, the case can be approached via surgeon preference. Translational/rotational injuries are further subcategorized based on the presence of vertebral body fracture along with the presence and severity of neural compression. Facet-fracture dislocations associated with endplate fractures necessitate posterior fusion; if there is a concern for progressive kyphosis, significant discoligamentous injury on MRI, or severe comminuted fracture, then a combined approach is warranted. If there is no vertebral body fracture, the approach is determined by the presence of disc herniation, similarly to cases of facet subluxation (after attempted reduction).
AO Spine Subaxial Cervical Spine Injury Classification System
Overview
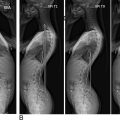
The AO Spine Subaxial Cervical Spine Injury Classification System ( Fig. 2 ) is a morphology-based system that was constructed in response to the lack of wide acceptance for any one subaxial cervical spine classification system. While SLICS, both internally and externally, showed good reliability and validity, other studies in the literature showed disagreement in the domain of morphology—this was the basis for the creation of the AO system. Its development stemmed from multiple assessments and revisions of concepts from the aforementioned thoracolumbar system and SLICS in conjunction with a database of AO spinal trauma cases and was considered complete once unanimous consensus was achieved in all domains.

The components of the system include injury morphology and neurologic status—carried over from the thoracolumbar system and SLICS—with the inclusion of two new domains, facet integrity and case-specific modifiers. The inclusion of facet integrity arises from previous literature attesting to its role in stability and, when injured, the implied high-energy mechanism and the worse patient outcomes that are associated. Injuries are described by their level, then morphologic type (the primary injury) with secondary injuries and modifiers placed in parentheses. The classification system is simplified in the following:
- •
Injury morphology
- •
Type A: fractures that result in compression of the vertebra with intact tension band
- •
A0: no bony or minor injury such as an isolated lamina or spinous process fracture
- •
Includes patients with central cord syndrome and no fracture
- •
- •
A1: compression fractures involving a single endplate without the involvement of the posterior wall of the vertebral body
- •
A2: coronal split or pincer fractures involving both endplates without the involvement of the posterior aspect of the vertebral wall
- •
A3: burst fractures involving a single endplate
- •
A4: burst fracture or sagittal split involving both endplates
- •
- •
Type B: failure of the posterior or anterior tension band through distraction with physical separation of the subaxial spinal elements while maintaining continuity of the alignment of the spinal axis without translation or dislocation
- •
B1: posterior tension band injury of bony structures only with extension into the vertebral body
- ⇒
Anterior structures such as disc or annulus may also be involved
- ⇒
- •
B2: posterior tension band injury of the posterior capsuloligamentous or bony capsuloligamentous structures
- ⇒
Anterior structures such as vertebral body or disc may also be involved and should be specified separately
- ⇒
- •
B3: anterior tension band injury with tethering of the posterior elements
- •
- •
Type C: injuries with displacement or translation of one vertebral body relative to another in any direction; anterior, posterior, lateral translation, or vertical distraction
- •
Because type C involves vertebra relative to one another, any associated injury should be specified as a subtype with a designation of Type A or B after the initial type C designation
- •
- •
- •
Facet injury
- •
If there are multiple injuries to the same facet, the highest level injury gets classified
- •
If both facets at the same level are injured, the right side is designated first
- •
F1: nondisplaced facet fracture
- •
< 1 cm fragment, < 40% of the lateral mass
- •
- •
F2: facet fracture with instability potential
- •
> 1 cm fragment, > 40% of the lateral mass, or displacement
- •
- •
F3: floating lateral mass—pedicle and lamina disruption resulting in disconnection of the superior and inferior articular facets at a level
- •
F4: pathologic subluxation or perched/dislocated facet
- •
BL: The bilateral (BL) modifier is used if both facets have the same injury at the same level
- •
- •
Neurologic status
- •
N0: neurologically intact
- •
N1: transient neurological deficit
- •
N2: radiculopathy
- •
N3: incomplete spinal cord injury
- •
“+” is designated for ongoing cord compression
- •
- •
N4: complete spinal cord injury
- •
NX: undetermined due to unexaminable patient
- •
- •
Case-specific modifiers
- •
M1: posterior capsuloligamentous complex injury without complete disruption
- •
often identified on MRI
- •
- •
M2: critical disc herniation—evidence of nucleus pulposus protruding posteriorly to a vertical line drawn along the posterior border of the inferior vertebral body at the injured level
- •
M3: Stiffening/metabolic bone disease
- •
Diffuse skeletal hyperostosis (DISH), ossification of the posterior longitudinal ligament (OPLL), ankylosing spondylitis (AS), ossification of the ligamentum flavum (OLF)
- •
- •
M4: signs of vertebral artery injury
- •
Reliability and validation
The authors assessed the interrater and intrarater reliability and validity of their system via an internal assessment of their data. They had 10 reviewers—beforehand, all received a paper with background information and purpose of the system—grade 10 cases to prove their competency against a gold standard determined by two of the senior authors. Once they felt that the authors had a correct understanding of the system (no incorrect grades given), they sent out 30 additional cases to be a review on two separate occasions. They found substantial overall interrater reliability when comparing levels of fracture severity (A/B/C/F) with k values of 0.64 and 0.65, respectively, between the two sessions. For intraobserver reliability, for all subtypes, they obtained a k value of 0.75, indicating substantial reliability. As for validation, for the first round of assessments, they found the range of correctness compared to the predetermined gold standard to be 20–29 cases. In the second round, the range was between 16 and 29 cases noting a decrease from the first round. Several external studies agreed that this system has high reliability, validity, and repeatability.
Clinical correlates
The young age of this classification system has resulted in a few available studies assessing its applicability in regard to HRQOL measures. One such study assessed the injury morphology and how it affects the long-term neurologic outcome. Mushlin et al. determined the AO Spine Subaxial Cervical Spine Injury Classification System’s morphology in a sample of 82 patients reviewed retrospectively and recorded the admission and 6-month follow-up ASIA Impairment Scale (AIS) and ASIA motor score (AMS). The A0 subtype was the most common and was found to have no complete injuries on admission or follow-up. They also showed significant improvement in AMS on follow-up from 70 to 90. Groups A3, A4, and C had the worst neurologic injuries and the highest percentage of patients with complete injuries; A3/A4 had the highest percentage at 55.6%, was the only subtype to have patients with complete injuries on follow-up, and also had the lowest AMS scores on follow-up. The authors hypothesized that this difference between A3/4 and C subtypes on follow-up was possibly due to the amenability of type C fractures to be decompressed by reduction maneuvers, which theoretically reduces time to decompression and ultimately improves long-term outcomes. This study successfully associates specific subtypes with ASIA designation and AMS score and can potentially influence timing to surgery and the risk/benefits discussion with patients in regard to long-term prognosis.
Du et al. prospectively assessed the effects of early vs delayed decompression on AIS and the Spinal Cord Independence Measure III (SCIM version 3) at 12-month follow-up. They included 402 patients who were divided into early decompression (< 72 hours after injury) and delayed decompression (≥ 72 hours after injury) groups. After intervention, each group was subsequently broken down into five morphology subtypes (A0, A1–4, B, C/F4, or F1–3) and outcomes were measured. 100 patients in the early group and 76 patients in the late group showed AIS improvement ≥ 1 grade, with only B and C/F4 types being statistically significant. SCIM version 3 showed that the early group also showed better functional recovery, with B subtypes being statistically significant. The authors concluded that early decompression led to better neurologic and functional recovery for the B and C/F4 subtypes and that type A and F1–3 subtypes failed to show significant clinical advantages to undergoing aggressive early decompression.
The Degenerative Subaxial Cervical Spine
The development of a classification system for spinal deformity, as seen in the Scoliosis Research Society-Schwab Classification, has proven clinically valuable by demonstrating correlation with standardized HRQOL measures. The literature points to a correlation between the simultaneous occurrence of deformities of the thoracolumbar and cervical spine and to correlations between cervical spine sagittal imbalance and HRQOL measures, Neck Disability Index (NDI), and myelopathy (modified Japanese Orthopedic Association [mJOA] score). As the spinal deformity literature matures, it is becoming increasingly clear that cervical deformity should be addressed in the context of global spinal alignment, as compensatory efforts are often made by the body to maintain horizontal gaze. These correlations created the basis for the development of a cervical spine deformity classification. As of the publication of this chapter, the Ames Classification stands alone as the most comprehensive and widely studied classification system for subaxial cervical spine deformity.
The Ames Classification
Overview
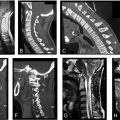
The overall goal of the Ames Classification ( Fig. 3 ) is to assess cervical spine deformity (CSD) in the context of global spinopelvic alignment and to address clinically relevant parameters. This system is an adaptation of the SRS-Schwab classification for adult thoracolumbar deformity and uses a deformity descriptor and five modifiers that include sagittal, regional, and global spinopelvic alignment and neurologic status. According to the authors, in order to utilize the classification system in practice, the following requirements must be obtained: (1) full-length standing posteroanterior (PA) and lateral spine radiographs that include the cervical spine and femoral heads; (2) standing PA and lateral cervical spine radiographs; (3) completed and scored mJOA questionnaire; (4) a clinical photograph or radiograph that includes the skull for measurement of the chin-brow vertical angle (CBVA).