Abstract
Coarse reticular opacities are the result of lung destruction caused by retracting fibrosis, which also produces cystic spaces. This combination of coarse reticular opacities and cystic spaces is better shown on computed tomography (CT) and described as honeycombing. The pathology of most cases of honeycombing fibrosis is classified as usual interstitial pneumonitis (UIP), which may be caused by collagen vascular diseases, environmental diseases, or idiopathic pulmonary fibrosis when there is no known cause. Inflammatory diseases, including sarcoidosis, hypersensitivity pneumonitis, Langerhans cell histiocytosis, and rarely desquamative interstitial pneumonitis, are also causes of honeycombing fibrosis. High resolution CT is often required to confirm the pattern of honeycombing and assess the distribution within the lungs, which is essential for separating the UIP group of diseases from the inflammatory diseases.
Keywords
honeycombing fibrosis, idiopathic pulmonary fibrosis (IPF), Langerhans cell histiocytosis (LCH), rheumatoid lung, sarcoidosis, scleroderma, usual interstitial pneumonitis (UIP)
Questions
- 1.
Refer to Fig. 19.1, A-C . The term honeycomb lung indicates which one of these processes?
- a.
Emphysema.
- b.
Cystic bronchiectasis.
- c.
Paraseptal emphysema.
- d.
End-stage interstitial fibrosis.
- e.
Multiple cavities.

Fig. 19.1
- a.
- 2.
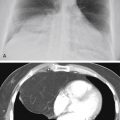
Which one of the following diagnoses is the least likely in the case shown in Fig. 19.2 ?
- a.
Lymphangitic metastases.
- b.
Sarcoidosis.
- c.
Asbestosis.
- d.
Usual interstitial pneumonia (UIP).
- e.
Rheumatoid lung.

Fig. 19.2
- a.
- 3.
Basilar distribution of interstitial disease is least likely in which of the following entities?
- a.
Asbestosis.
- b.
Idiopathic pulmonary fibrosis (IPF).
- c.
Scleroderma.
- d.
Sarcoidosis.
- e.
Rheumatoid lung.
- a.
Discussion
Honeycomb lung is characterized by coarse reticular interstitial opacities with intervening lucent spaces. 462 The typical appearance of honeycomb lung is shown in Figs. 19.1, A-C, and 19.2 . Diseases that produce honeycomb lung tend to affect both lungs and are usually extensive, although the degree of involvement is frequently not uniform. The lucent spaces are described as cysts and should not be confused with those seen in emphysema or cavities. Emphysema involves tissue destruction without fibrosis, whereas honeycombing involves tissue destruction by retracting fibrosis. Paraseptal emphysema involves the subpleural portions of the lung and, when it is extensive, may resemble honeycombing. The bullae of paraseptal emphysema are often in a single subpleural layer, in contrast to the cysts of honeycombing which are in multiple layers. Cavities may be multifocal and extensive but are not contiguous diffuse spaces. High-resolution computed tomography (HRCT) should reliably differentiate the cystic spaces caused by honeycombing from emphysema or cavities. 289 HRCT also provides a map of the distribution of the honeycombing and often allows the radiologist to determine a specific cause. 440
Recognizing the honeycomb pattern is helpful in narrowing the differential diagnosis for reticular interstitial opacities ( Chart 19.1 ). As previously suggested, the honeycomb appearance indicates end-stage scarring of the lung with revision of the pulmonary architecture by fibrosis. (Answer to question 1 is d .) Serial examinations may reveal progression from fine reticular opacities to honeycombing. This is often the case in the pneumoconioses, collagen vascular diseases, or idiopathic pulmonary fibrosis (IPF). Additionally, identification of the cystic spaces of honeycomb lung permits exclusion of other causes of reticular opacities such as acute pulmonary edema, viral pneumonia, mycoplasma pneumonia, lymphangitic spread of carcinoma, lymphoma, and lymphocytic interstitial pneumonia (answer to question 2 is a ). Honeycomb lung also has grave prognostic implications because the cystic spaces are due to end-stage irreversible scarring.
- I.
Usual interstitial pneumonitis
- A.
Collagen vascular diseases 296
- 1.
Rheumatoid lung 59 , 241 , 532
- 2.
Scleroderma 19
- 3.
Dermatomyositis and polymyositis 259 , 523
- 4.
Mixed connective tissue disease 309
- 5.
- 1.
- B.
Environmental diseases
- C.
Idiopathic pulmonary fibrosis (IPF) 86 , 104 , 440 , 553 , 569
- A.
- II.
Inflammatory diseases
- A.
Sarcoidosis
- B.
Langerhans cell histiocytosis (LCH) 1
- C.
Hypersensitivity pneumonitis (chronic) 58 , 128 , 497 , 501 , 570
- D.
Desquamative interstitial pneumonitis (DIP; rarely causes honeycombing) 355
- A.
- III.
Mimicking opacities with lucent spaces
- A.
Cystic bronchiectasis
- B.
Superimposed cysts (LCH; lymphangioleiomyomatosis [LAM]) 424
- A.
Cystic bronchiectasis ( Fig 19.3 ) sometimes produces a radiologic appearance of coarse irregular opacities with intervening cystic spaces that resemble honeycombing fibrosis. Bacterial, viral, and tuberculous pneumonias may all cause bronchial wall necrosis with late scarring and bronchiectasis, but this necrosis rarely causes diffuse bilateral bronchiectasis that would be confused with honeycombing fibrosis. However, the late stages of cystic fibrosis do cause diffuse disease with extensive scarring. 521 The scarring of cystic fibrosis is caused by recurrent pneumonias that complicate the chronic problems of thick mucus and impaired bronchial clearance. The radiologic appearance differs from the primary interstitial diseases that cause lung fibrosis by the presence of perihilar bronchial thickening. Additionally, because cystic fibrosis is an obstructive bronchial disease, there is often increased lung volume, in contrast with restrictive scarring from the fibrotic interstitial diseases that reduce lung volume.