, Leonid Tiutin2 and Thomas Schwarz3
(1)
Russian Research Center for Radiology and Surgery, St. Petersburg, Russia
(2)
Department of Radiology and Nuclear Medicine, Russian Research Center for Radiology, St. Petersburg, Russia
(3)
Department of Nuclear Medicine Division of Radiology, Medical University Graz, Graz, Austria
Abstract
Presently colorectal cancer (CRC) is one of the most prevalent of oncological diseases. In 2003, 45,020 cases of CRC were detected in the Russian Federation (Merabishvili 2006). However, stages I-II of the disease were detected in only 22.8% of patients. In the remaining cases, signs of stages III and IV of tumor process were revealed. Consequently, within 1 year of tumor detection, lethality reached 32.3% and radical treatment was given to only 41.3% of patients (Shalimov et al. 2000).
Presently colorectal cancer (CRC) is one of the most prevalent of oncological diseases. In 2003, 45,020 cases of CRC were detected in the Russian Federation (Merabishvili 2006). However, stages I-II of the disease were detected in only 22.8% of patients. In the remaining cases, signs of stages III and IV of tumor process were revealed. Consequently, within 1 year of tumor detection, lethality reached 32.3% and radical treatment was given to only 41.3% of patients (Shalimov et al. 2000).
Growth in number of CLC cases is influenced by the following factors: the nature of food (high-caloric food with prevalence of animal fats, proteins and refined carbohydrates-sugars); sedentary life leading to obesity, especially after the age of 50; hypotonia and atonia of the intestine at elderly age, accompanied by constipations; presence of endogenous carcinogens (indole, skatole, guanidine, metabolites of steroid hormones) in the intestinal contents; chronic traumatism of the mucous membrane of the large intestine in areas of physiologic curves; presence of precancerous diseases (chronic nonspecific and granulomatous colites, diverticulites and diverticuloses, polipous lesions).
Pathognomonic signs of colorectal cancer do not exist. The small-sized tumor as a rule does not manifest itself. As the malignant neoplasm grows, general symptoms of intestinal malfunction appear.
The main clinical forms of cancer of the colon include toxic-anemic, electrolytic, dyspeptic, obturative, pseudoinflammatory and tumorous (atypical) cancers. In case of colorectal cancer, the most frequent (and most often late) symptoms are bleeding, pain in the area of the perineum, functional bowel disorders (change in rhythm of defecation, form of faeces, diarrhea, constipation, fecal and gas incontinence).
8.1 Pathologic Anatomy and Mechanisms of Metastases
Malignant neoplasm is most often situated in the sigmoid colon and blind gut. In 1–3% of cases the lesion can have a multifocal character. The main ways of dissemination of the tumor process in CRC are via the lymphogenous, hematogenous and implantation routes. The hematogenous and implantation mechanisms of metastasis in cancers of the colon and rectum do not have significant differences. On the contrary, lymphogenous metastasis of the large intestine has its own specific features.
Stages of Lymphogenous Metastasis of Cancer of the Colon
Stage I – lesion of epicolic or paracolic lymph nodes
Stage II – lesion of intermediate or mesenteric lymph nodes
Stage III – lesion of paraaortic lymph nodes in the area of the root of mesocolon
As is known, lymph is accumulated in the lymphatic cistern situated at the level S1–2 and flows through the thoracic duct into the venous system in the area of the left venous angle, at the confluence of the subclavian and inner jugular veins, thus conditioning metastatic lesion of lymph nodes of the left supraclavicular (Virchow’s metastasis).
Lymphogenous metastasis in rectal cancer depends entirely on the localization of the primary pathologic formation.
Characteristics of Lymphogenous Metastasis of Cancer of the Rectum
In the case of supra-ampullary location of the tumor, its dissemination to lymph nodes occurs upwards along the superior rectal artery and from the root of inferior mesenteric vessels with involvement of retroperitoneal lymph collectors, most often paraaortic.
In the case of infra-ampullary location of the tumor, pararectal lymph nodes are affected, situated along the middle and inferior rectal arteries. During further dissemination of tumor process lymph nodes of the hypogastric area are involved.
Cancer of the anal section of the rectum is characterized by metastatic lesion of lymph nodes situated along inferior rectal arteries and of those of the hypogastric and inguinofemoral areas.
8.2 Methods of Diagnosis
The main methods of diagnosis of cancer of the large intestine are digital investigation of the rectum, procto(sigmoido)scopy, fibrocolonoscopy with target biopsy and irrigoscopy with “double” contrast. Radiological examination permits determination of the precise location of the malignant neoplasm, its size, relations with adjacent anatomic structures, and depth of lesion of the intestinal wall. Diagnostic accuracy of irrigoscopy is defined as 85–94%. Using transabdominal ultrasound (US) for detecting colorectal cancer is possible, but the detected signs are most often nonspecific. It is due to presence of gas in the intestine, which checks the passage of ultrasound waves. At the same time, it is the ratio of gas/tissue in the area of tumor, and not the extension of lesion, that is crucial in visualizing primary formations in the large intestine. This means that pathologic formation will be detected provided that the ratio of gas/tissue in the intestine changes in favor of the tissue, which is possible only in case of obstructing tumors.
The use of computed tomography (CT) for diagnosing malignant neoplasms of the large intestine is efficient only in late stages of the disease (T3 and T4). Consequently, using CT in CRC patients is suitable for determining tumor infiltration of surrounding anatomic structures and detecting signs of generalization of the malignant process. The main advantage of the method is its high resolving capacity (2–4 mm) and consequently possible visualization of small metastatic foci, including those in the liver. However, in case of subcapsular or subdiaphragmatic location of metastases, false-negative results may be obtained.
8.3 Staging
Clinical staging of the tumor process in cancers of the colon and rectum is implemented according to the international classification by the TNM system, which reflects three obligatory components: size and depth of invasion of the primary tumor, metastasis to regional and juxtaregional lymph nodes, and metastasis to distant organs (Edge 2010).
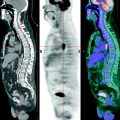
8.3.1 PET Diagnosis
Assessment by T Category
The diagnostic accuracy of positron emission tomography (PET) in detecting malignant neoplasms of the large intestine depends, as a rule, on the size of the primary tumor. So, sensitivity of the method in diagnosis of the late stages of the disease (T3–T4) may reach 92%. However, in the initial stages of tumor process this index does not exceed 56–64% (Cohade et al. 2003; Delbeke 1999; Meta et al. 2001). The widest spread causes of false-negative results are small size of pathologic formation and hypometabolism of 18F-fluorodeoxyglucose (18F-FDG) in malignant neoplasms of some morphologic kinds. For example, one should treat with caution negative 18F-FDG PET results in highly differentiated and mucinous adenocarcinomas. In these histological forms of tumors 18F-FDG PET sensitivity does not exceed 58% (Berger et al. 2000 and Abdel-Nabi et al. 1998).
Specificity of the method in diagnosis of colorectal cancer is relatively low and ranges within 66–71%. High uptake of radiopharmaceutical (RP) having a focal character may be observed in the area of benign villous polyps and in the projection of hemorrhoid boluses of the rectum. However, the most frequent cause of false-positive results is the physiologic uptake of RP in the intestinal wall due to its peristalsis. In these cases, the technique of delayed scanning of the region of interest can be used for determining the nature of detected changes. In case of physiologic uptake of RP in the intestinal wall in the delayed phase of the examination, the focus either will change its position because of intestinal peristalsis or will completely disappear.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree