, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
Abstract
In this chapter, we will introduce tips to aid in lumbar spine MR interpretation. We will also explain imaging findings of common spine disorders associated with back pain and lumbar radiculopathy, such as herniated intervertebral disk, spinal stenosis, spondylolysis, facet joint arthrosis, as well as alignment disorders such as spondylolisthesis, kyphosis, and scoliosis.
In this chapter, we will introduce tips to aid in lumbar spine MR interpretation. We will also explain imaging findings of common spine disorders associated with back pain and lumbar radiculopathy, such as herniated intervertebral disk, spinal stenosis, spondylolysis, facet joint arthrosis, as well as alignment disorders such as spondylolisthesis, kyphosis, and scoliosis.
2.1 Lumbar Spine MR in Patients with Back Pain: What Should We Focus on?
To interpret spine MR in patients complaining of pain, it is best to start by screening the sagittal images. On T2-weighted sagittal images, the three anatomic areas of the central canal, spinal cord, and intervertebral disks should be reviewed carefully. On T1-weighted sagittal images, bone marrow signal abnormality should be carefully reviewed with reference to the signal of the intervertebral disks. Any focal or diffuse low signal intensity of the bone marrow on T1-weighted sagittal images could suggest bony pathology. Following the sagittal images, the axial images are then reviewed from caudal to cranial and vice versa, comparing with the corresponding levels on the sagittal images. On T2-weighted axial images, the relationship of the posterior margin of the intervertebral disks with the dural sac and nerve roots should be carefully defined to identify a herniated disk. Common mistakes include missing superior migration of herniated disks into the foraminal or extraforaminal zones and inferior migration of herniated disks into the subarticular zones. On T1-weighted axial images, the course of the descending nerve roots from the dural sac to the neural foramina should be traced, to identify nerve root anomalies such as a conjoined nerve root (Song et al. 2008).
Table 2.1
Special areas to focus on lumbar spine MR interpretation
T2-weighted sagittal images | Central canal, spinal cord, intervertebral disks |
T1-weighted sagittal images | Bone marrow signal alteration |
T2-weighted axial images | Posterior margin of intervertebral disks, central canal, subarticular zones, foraminal–extraforaminal zones |
T1-weighted axial images | Course of nerve roots, posterior margin of intervertebral disks |
Recent articles suggest that lumbar imaging for low back pain without clinical evidence of a serious underlying condition does not improve clinical outcome (Modic et al. 2005; Chou et al. 2009). One prospective study showed no cases of malignancy in 1,170 patients under the age of 50 presenting without a history of cancer, weight loss, an evidence of systemic illness, or a history of failure to improve with conservative therapy (Deyo and Diehl 1988). The American College of Radiology considers spine imaging appropriate only when there are red flag features that suggest an underlying systemic disease, in the face of progressive neurologic deficits, or cauda equina syndrome (Bradley 2007). The American Pain Society and American College of Physicians further emphasize that imaging should be recommended only when the patient with radiculopathy is a candidate for therapeutic intervention, such as epidural steroid injection or surgery (Chou et al. 2007).
Common spine disorders associated with back pain or lumbar radiculopathy include herniated intervertebral disks, spinal stenosis, spondylolysis, spondylolisthesis, kyphosis, scoliosis, facet joint arthrosis, and Baastrup’s phenomenon.
Table 2.2
Common spine disorders associated with back pain and lumbar radiculopathy
Herniated intervertebral disks |
Spinal stenosis |
Alignment disorders such as spondylolisthesis, kyphosis, and scoliosis |
Facet joint arthrosis |
Baastrup’s phenomenon |
Annular fissure, disk degeneration |
2.2 Herniated Intervertebral Disk
A combined task force of the American Society of Spine Radiology, the American Society of Neuroradiology, and the North American Spine Society presented recommendations defining terminology of herniated intervertebral disks in the lumbar spine (Fardon and Milette 2001). According to the recommendations, a herniated intervertebral disk is defined as a “localized displacement of disc material beyond the disc space.” “Localized” is defined as displaced disk material involving less than half of the circumference of the disk on axial images. The margin of the disk is determined by the outline of the adjacent vertebral bodies excluding osteophytes.
Herniated intervertebral disks are further divided into protrusions and extrusions based upon the shape of the displaced disk. A protrusion is a disk herniation where the distance between the edges at the base of the displaced disk material is larger in all planes than the maximal distance between the edges of the displaced disk. An extrusion refers to a disk herniation where the maximal distance between the edges of the displaced disk is larger than the distance between the edges at its base in any plane.
The location of the displaced disk material is classified as central, subarticular (lateral recess), foraminal (pedicular), or extraforaminal (far lateral) zones on the axial plane. The central and subarticular zones are divided in the sagittal plane by the medial edge of the facet joint. The subarticular and foraminal zones are divided in the sagittal plane by the medial edge of the pedicle. The foraminal and extraforaminal zones are divided in the sagittal plane by the lateral edge of the pedicle. In the sagittal or coronal planes, the location of disk material may also be classified as being at the suprapedicular, pedicular, infrapedicular, or disk levels.
In some cases, the herniated disk material may show higher signal on T2-weighted images than the parent disk, which can be a cause of decreased detectability; thus careful tracing of the posterior margin of the intervertebral disk is required to locate the herniated disk.
If the herniated disk is sequestrated from the parent disk, it can be misdiagnosed as an epidural tumor. The features differentiating a herniated disk from an epidural tumor include (1) associated protrusion involving the base of the adjacent intervertebral disk, (2) T2 low signal intensity within the disk material, and (3) rim-like enhancement of the disk material.
The relationship of the herniated disk and adjacent nerve roots can be described as being in contact, deviated, or compressed (Pfirrmann et al. 2004). The numbering of the nerve roots may be confusing in the lumbar spine, as the descending root in the epidural space will exit through the neural foramen of the lower vertebral level. For example, at the L4–5 disk level there are two pairs of nerve roots outside the dural sac; the L4 nerve roots are located in the foraminal or extraforaminal zones bilaterally, while the L5 nerve roots are located in the central or subarticular zones bilaterally. Thus a herniated disk located at the L4–5 central or subarticular zones may compress upon the L5 nerve roots (and not L4 nerve roots), while a herniated disk at the L4–5 foraminal or extraforaminal zones may compress upon the L4 nerve roots.
Radiculopathy is mainly caused by perineural inflammation due to the herniated disk, rather than from nerve root compression itself. Radiculopathy implies the presence of objective signs of neural dysfunction including motor weakness, hypesthesia/paresthesia, or diminished deep tendon reflexes. Radiculopathy is typically accompanied by intermittent, lancinating, electrical, or burning radiating pain (Del Grande et al. 2012).
2.3 Spinal Stenosis
Spinal stenosis is a degenerative disorder where there is narrowing of the central canal, lateral recesses, or neural foramina, with resultant nerve root or spinal cord compression. The most common symptoms in patients with lumbar spinal stenosis are back pain (95 %), claudication (91 %), leg pain (71 %), weakness (33 %), and voiding disturbances (12 %) (Amundsen et al. 1995). Claudication is a clinical condition where patients experience lower leg pain and the feeling of weakness during walking. Spinal stenosis is a common cause of claudication (neurogenic claudication). Vascular compromise (especially arterial insufficiency to the legs) can be another cause of claudication (vascular claudication).
Common descriptors used for determining central canal stenosis include the dural sac anteroposterior (AP) dimension and the dural sac cross-sectional area. Dural sac AP dimensions of less than 10 mm or dural sac cross-sectional areas of less than 100 mm2 constitute stenosis (Maus 2012). A recent article (Lee et al. 2011) suggested that central canal stenosis in the lumbar spine can be diagnosed when there is obliteration of the ventral subarachnoid space on axial and sagittal images and may be graded as mild, moderate, or severe according to the degree of CSF obliteration and nerve root clumping. With mild central canal stenosis, the nerve roots remain separate inside the dura without clumping. In moderate central canal stenosis, there is some clumping of the nerve roots inside the dural sac. Severe central canal stenosis occurs when there is a single bundle of nerve roots visualized inside the dural sac due to severe clumping.
Lumbar foraminal stenosis can be graded according to the obliteration of perineural fat in the neural foramen and associated nerve root compression (Lee et al. 2011). Mild, moderate, and severe lumbar foraminal stenoses are defined as follows: mild foraminal stenosis when there is perineural fat obliteration in one direction such as AP or superior–inferior, moderate foraminal stenosis when perineural fat obliteration occurs in two or more directions, and severe foraminal stenosis when there is nerve root compression or morphological changes of the nerve root due to compression.
2.4 Alignment Disorders (Spondylolisthesis, Scoliosis, Kyphosis)
Alignment disorders such as spondylolisthesis, scoliosis, and kyphosis can be a source of back pain and occasionally a cause of radiating pain or claudication due to resultant spinal stenosis. Spondylolisthesis is a condition where there is anterior displacement of a vertebral body relative to the vertebral body below, while retrolisthesis refers to the condition in which the vertebral body is displaced posteriorly relative to the vertebral body below.
Spondylolisthesis can be graded as follows: the anteroposterior (AP) diameter of the superior surface of the lower vertebral body is divided into quarters, with grades I to IV spondylolisthesis assigned to slips involving up to one, two, three, or four quarters of the upper vertebra, respectively. The causes of lumbar spondylolisthesis are congenital (dysplastic), isthmic (spondylolytic), degenerative, traumatic, pathological, and iatrogenic (Butt and Saifuddin 2005). The two most common causes of spondylolisthesis are spondylolysis (spondylolytic spondylolisthesis) and facet joint degeneration (degenerative spondylolisthesis). Spondylolysis is a disorder where there is a defect involving the pars interarticularis. The pars interarticularis is the part of vertebral posterior element between the superior and inferior articular processes. Spondylolysis is most commonly seen at the L5 level and can be a cause of spondylolisthesis in cases of bilateral involvement. In spondylolytic spondylolisthesis, both neural foramina can often be narrowed, but the central canal is usually widened as the lamina and spinous process are not displaced anteriorly. On the contrary, in degenerative spondylolisthesis caused by facet joint degeneration, the central canal is severely narrowed in most cases. Degenerative spondylolisthesis is thought to be the end result of segmental instability.
Degenerative lumbar scoliosis refers to the condition in which asymmetric disk degeneration and facet arthrosis result in abnormal curvature of the lumbar spine. In such cases, patients can complain of low back pain and radiculopathy due to foraminal stenosis. In degenerative lumbar scoliosis, foraminal stenoses can be unilateral and asymmetric, e.g., involving left L1–2, left L2–3, right L4–5, and right L5–S1.
Atrophy of the back muscles and facet arthrosis can also result in lumbar kyphosis (lumbar degenerative kyphosis = LDK). Standing lateral plain radiographs are essential for diagnosing LDK, with kyphotic alignment of the lumbar spine curvature demonstrated. On MR, there is severe fatty atrophy of the back muscles.
2.5 Degenerative Changes of the Posterior Elements (Facet Joint Arthrosis, Baastrup’s Phenomenon)
The facet joint is a true synovial joint and like other joints is susceptible to the same degenerative changes, namely, joint space narrowing, osteophyte formation, subchondral sclerosis, subchondral cyst formation, joint effusion, and synovial cyst formation. Facet joint degeneration (facet arthrosis) is a common source of back pain in the elderly; it is the main cause of degenerative spondylolisthesis with central canal stenosis causing radiating pain and claudication and occasionally a cause of lateral recess stenosis due to osteophytes. Ventral synovial cysts from the facet joints can compress upon the descending nerve roots, which can be a cause of radiculopathy. In case of epidural cystic mass, the clues to consider synovial cyst are (1) degenerative change in the adjacent facet joint, (2) communication with joint effusion or joint space, and (3) old age.
Interspinous pseudoarthrosis and cyst formation can also occur secondary to close approximation of the spinous processes. This formation has been termed Baastrup’s phenomenon (Malfair and Beall 2007). Redundancy of the interspinous ligament may extend into the posterior aspect of the central spinal canal, resulting in effacement of the retrothecal fat pad and posterior narrowing of the spinal canal because of the redundant posterior ligamentous soft tissues. When the posterior degenerative changes are severe, an adventitial bursa may form and occasionally may communicate with the facet joints. Interspinous bursae or hypertrophic degenerative changes can extend anteriorly from the interspinous space and result in canal stenosis
Forget Me Nots!
On T2-weighted sagittal images, the three anatomic areas of the central canal, spinal cord, and intervertebral disks should be reviewed carefully.
On T1-weighted sagittal images, evaluation of bone marrow signal abnormality should be carefully reviewed with reference of the signal of the intervertebral disks.
Features differentiating herniated disks from epidural tumor include (1) protrusion at the base of the adjacent intervertebral disk, (2) T2 low signal intensity of the disk material, and (3) rim-like enhancement of the disk material.
Spinal stenosis of the lumbar spine can be graded by the degree of CSF obliteration (for central canal stenosis) and perineural fat obliteration (for foraminal stenosis).
The two most common causes of spondylolisthesis are spondylolysis (spondylolytic spondylolisthesis) and facet joint degeneration (degenerative spondylolisthesis).
The facet joint can show similar degenerative features to other synovial joints, including joint space narrowing, osteophytes, subchondral sclerosis, subchondral cyst, joint effusion, and synovial cyst formation.
2.6 Illustrations: Common Spine Disorders Associated with Back Pain
2.6.1 Schematic Illustrations of the Nomenclature for Disk Herniation
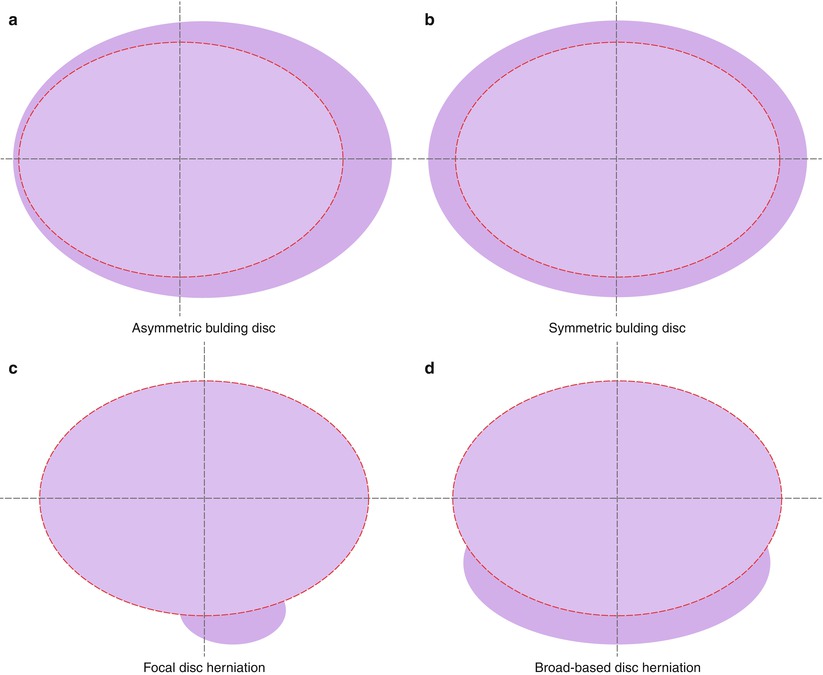
Fig. 2.1
Schematic illustrations for defining disk herniation. A herniated intervertebral disk is defined as a “localized displacement of disk material beyond the disk space.” The disk space is delineated by the outline of the adjacent vertebral bodies excluding osteophytes. “Localized” refers to displaced disk material involving less than half of the circumference of the disk as seen on axial images; thus (a, b) are not disk herniations, but represent bulging disks. (c, d) Are schematic illustrations of disk herniation with displaced disk material involving less than half of the circumference of the disk on axial images. A focal disk herniation (c) indicates disk herniation involving less than one quarter of the circumference of the disk, while a broad-based disk herniation (d) affects more than one quarter of the disk circumference (Published with kind permission of © HealthWave 2014. All Rights Reserved)
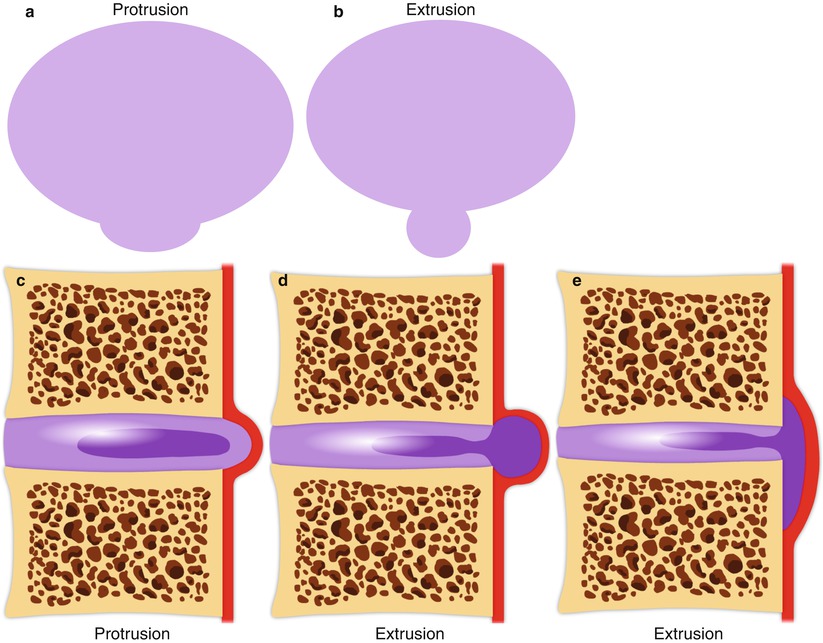
Fig. 2.2
Schematic illustrations of disk protrusion and extrusion. A herniated intervertebral disk is further classified as a protrusion or extrusion depending on the shape of the displaced disk. A protrusion is defined as when the distance between the edges at the base of the herniated disk is larger than the maximal distance between the edges of the displaced disk material in both axial and sagittal planes (a, c). An extrusion refers to a disk herniation where the maximal distance between the edges of the displaced disk is larger than the distance between the edges at its base in either axial or sagittal planes (b, d, e) (Published with kind permission of © HealthWave 2014. All Rights Reserved)
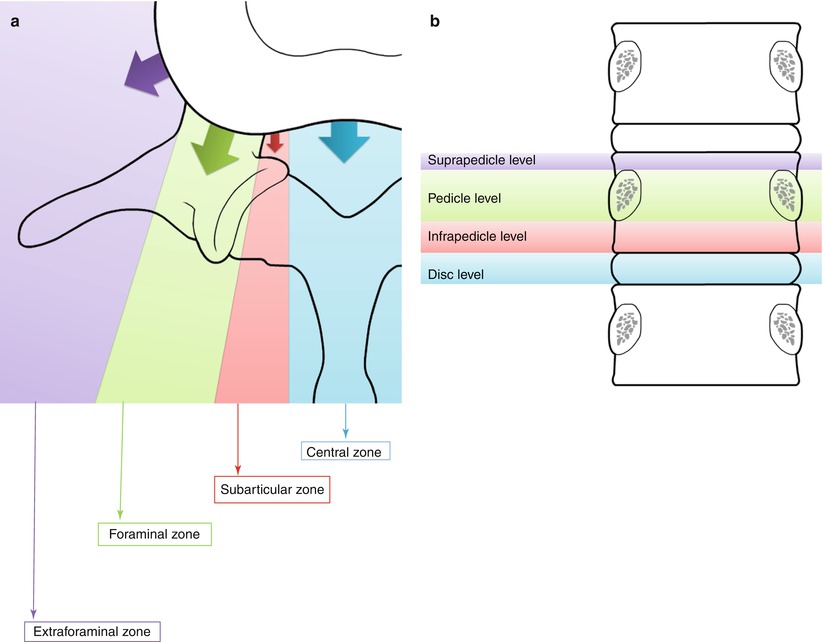
Fig. 2.3




(schema A11). Schematic illustrations describing the location of herniated disks. The location of disk material is classified as central, subarticular (lateral recess), foraminal (pedicular), or extraforaminal (far lateral) zones in the axial plane (a). The central and subarticular zones are divided by a sagittal plane along the medial edge of the facet joint. The subarticular and foraminal zones are divided by a sagittal plane along the medial edge of the pedicle. The foraminal and extraforaminal zones are divided by a sagittal plane along the lateral edge of the pedicle. On the sagittal or coronal planes, the location of disk material may also be described as being at the suprapedicular, pedicular, infrapedicular, or diskal levels (b) (Published with kind permission of © HealthWave 2014. All Rights Reserved)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree