CHAPTER 21 Common surgical procedures of the gastrointestinal tract
Introduction
Gastrointestinal (GI) surgery is a vast topic encompassing many different techniques. These procedures can be performed by the traditional open surgery or more and more commonly laparoscopically (keyhole). Whether surgery is open or laparoscopic, the procedures should remain the same.
Upper gastrointestinal procedures
Cancer surgery
The principle of cancer surgery is to remove the tumor completely with histologically proven margins and the lymph nodes that drain the tumor. Histologically, completeness of tumor clearance from the resection margins is classified R0, R1and R2. An R0 resection is defined as one where all margins are histologically free of tumor. An R1 resection is defined as one in which microscopic residual disease has been left behind. An R2 resection is defined as incomplete resection with macroscopic residual disease.
Esophagectomy
Indication: esophageal cancers and occasionally benign esophageal strictures.
Main blood vessels divided: left gastric artery and esophageal arterial branches.
Subtotal gastrectomy
Area resected: the distal half to two thirds of stomach with the surrounding lymph nodes.
Main blood vessels divided: left and right gastric arteries, right gastroepiploic artery.
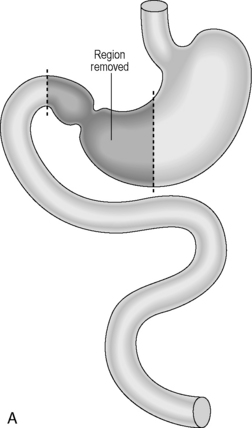
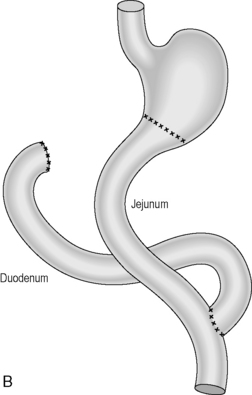
Reconstruction: historically, the continuity was usually reconstructed by carrying out a simple gastrojejunostomy. This can result in significant biliary reflux which can cause anastomotic ulcerations. A roux-en-Y reconstruction negates biliary reflux and is generally the preferred option of reconstruction (Figures 21.1A, 21.1B).
Total gastrectomy
Indication: gastric cancer located in the proximal part or body of the stomach.
Area resected: whole stomach and surrounding lymph nodes.
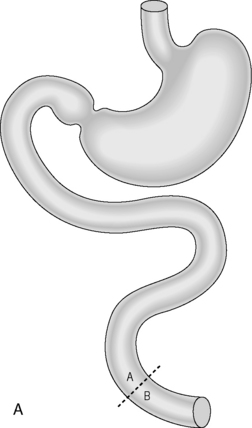
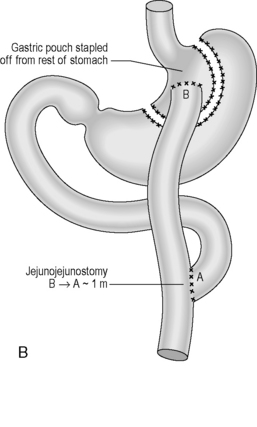
Reconstruction: A roux-en-Y reconstruction with or without a neogastric pouch. This is akin to a J-shaped ileoanal pouch (see ileoanal pouch) (Figures 21.2A, 21.2B and 21.3A, 21.3B).
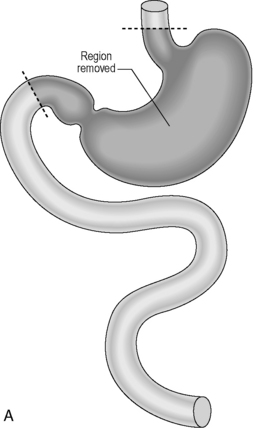
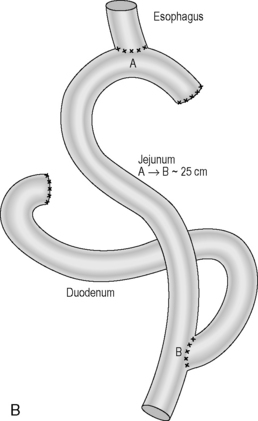
Figure 21.2 (A) Total gastrectomy, resection margins; (B) total gastrectomy, roux-en-Y reconstruction.
Benign surgery
Antireflux procedures
Indication: Gastro-esophageal reflux disease including repair of hiatus hernia.
Procedure: Performed laparoscopically, this procedure essentially consists of two parts:
Antireflux surgery has a number of variations; however, the two gold standard procedures were described by the German surgeon Rudolph Nissen (1896–1981) and the French surgeon Andre Toupet born in 1915. Nissen’s fundoplication is a complete (360 degrees) wrap with the fundus round the lower esophagus and Toupet’s fundoplication is one where the fundus wraps the posterior aspect of the lower esophagus, variations suggest between 180 and 270 degrees (Figures 21.4 A–F).
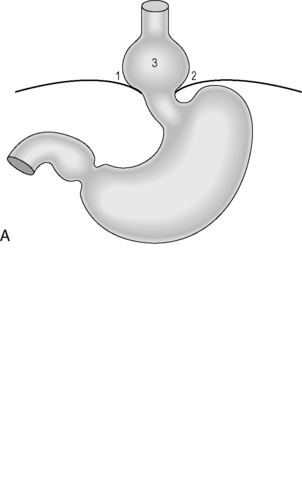
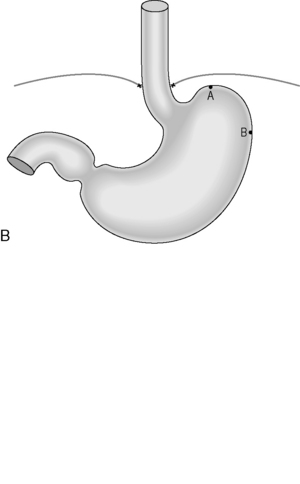
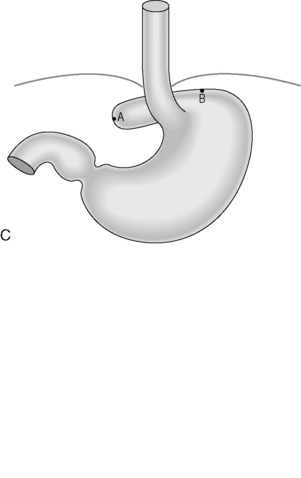
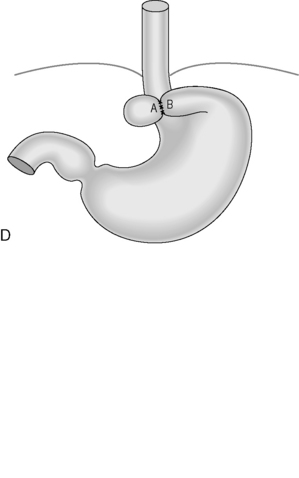

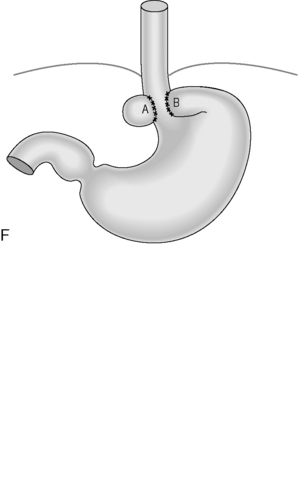
Figure 21.4 (A) Wide diaphragmatic hiatus (1–2), gastric herniation (3); (B) gastric herniation reduced and the hiatus repaired. A retro-esophageal tunnel is created to allow for fundoplication; (C) gastric fundus pulled through to the right of the esophagus; (D) the Nissen 360 degrees wrap created by suturing points ‘A’ and ‘B’; (E) Nissen wrap at barium swallow; (F) the alternative Toupet 270 degrees wrap can be created by suturing points ‘A’ and ‘B’ to the sides of the esophagus.
Main blood vessel divided: the short gastric vessels may be divided.
Heller’s myotomy
Procedure: this procedure is carried out laparoscopically. A longitudinal incision down to but not beyond the mucosa is made in the lower esophagus extending into the gastric cardia. The smooth muscle is parted preventing it from forming a ring when contracted. Many patients will suffer from gastro-esophageal reflux following this and a partial fundoplication is often performed to reduce this.
Main blood vessels divided: none.