Community Acquired Pneumonia
Jud W. Gurney, MD, FACR
Key Facts
Imaging Findings
Best diagnostic clue: Focal parenchymal abnormality in patient with fever
If initial radiograph normal in patient strongly suspected of having pneumonia, repeat radiograph in 24 hours or do CT
Centrilobular nodules in patchy distribution: Most helpful finding distinguishing infectious vs. noninfectious disease
All patients > 40 years old (or younger smokers) should have follow-up until resolution
50% resolution 2 weeks; 66% 4 weeks; 75% 6 weeks
Mortality associated with 2 radiographic abnormalities: Bilateral pleural effusions and multilobar disease
Top Differential Diagnoses
Cardiogenic Pulmonary Edema
Hemorrhage
Hypersensitivity Pneumonitis
Pathology
Offending organism cultured in < 50%
Clinical Issues
No individual or combinations of signs and symptoms from history and physical examination can reliably confirm or refute presence of pneumonia
Diagnostic Checklist
Diagnosis based on culture (grayscale image does not substitute for Gram stain)
TERMINOLOGY
Definitions
Community acquired pneumonia (CAP): Lung infection that occurs outside hospital setting
IMAGING FINDINGS
General Features
Best diagnostic clue: Focal parenchymal abnormality in patient with fever
Imaging Recommendations
Best imaging tool: Radiographs usually suffice, CT use increasing to reduce diagnostic uncertainty
Protocol advice
Indications for chest radiograph: Fever, cough, sputum production, coarse crackles
If initial radiograph normal in patient strongly suspected of having pneumonia, repeat radiograph in 24 hours or do CT
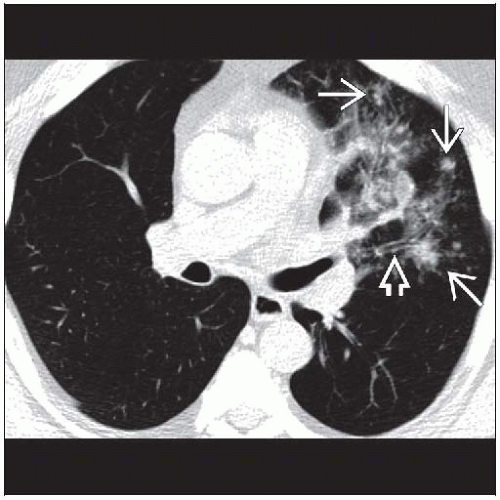
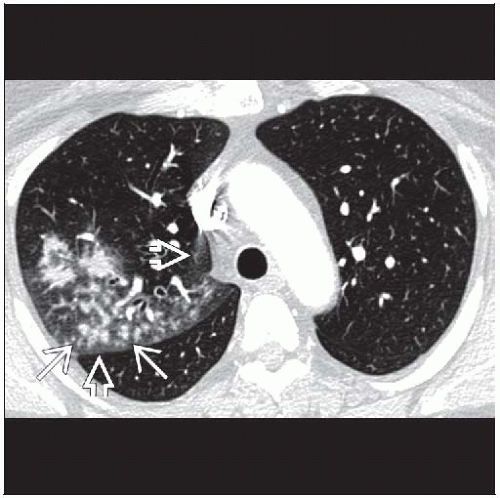
CT Findings
More sensitive (˜ 100%) than radiographs (50-70%)
More expensive and increased radiation dose
HRCT patterns: Frequency in bacterial vs. atypical (mycoplasma and viral) pneumonia
Centrilobular clustered nodules
Bacterial 10%, viral & mycoplasma 66%
Patchy distribution: Most helpful finding distinguishing infectious vs. noninfectious disease
Lobular consolidation
Bacterial 33%, mycoplasma 85%, uncommon in viral pneumonia
Segmental consolidation
Bacterial 75%, mycoplasma 40%
Lobular ground-glass opacities
Bacterial 10%, viral & mycoplasma 60%
Crazy-paving pattern
Bacterial 30%, viral & mycoplasma 15%
Bronchovascular bundle thickening
Bacterial 55%, viral & mycoplasma 70%
Ground-glass halo around consolidation
Bacterial 45%, viral & mycoplasma 30%
Inner zone of lung
Bacterial 33%, viral & mycoplasma 85%
Pleural effusions
Bacterial 40%, viral & mycoplasma 20%
Lymphadenopathy uncommon (3%) in any community acquired pneumonia
Radiographic Findings
High sensitivity: May not have visible abnormality in
Immunocompromised, especially if neutropenic
Dehydration: Controversial; rare if it exists at all
Typical distribution segmental consolidation: Unilateral or bilateral
Significant interobserver variability in pattern recognition
May have nearly any pattern from ground-glass, interstitial, to consolidation
Pattern not diagnostic of organism; single organism may cause multiple patterns
Poor agreement between readers for pattern of disease, presence of air bronchogram, bronchial wall thickening
Good to excellent agreement between readers for pleural effusion, extent of radiographic abnormalities
Lobar vs. bronchopneumonia
Pathologic designation; difficult to reliably identify on radiographs
Unusual patterns
Hyperinflation common with viral pneumonia (due to obstruction of distal airways)
Lobar enlargement with bulging fissures: Klebsiella pneumonia
Round pneumonia more common pattern in children
Pneumatoceles
Develop later in course of pneumonia (classically in S. aureus), may persist for months, resolve spontaneously
Hilar adenopathy
Rare, limits differential: Tuberculosis, mycoplasma, fungi, mononucleosis, measles, plague, tularemia, anthrax, pertussis
Complications
Cavitation: Suggests bacterial disease (S. aureus, Gram-negative bacteria, anaerobes)
Empyema
Reactive parapneumonic effusions in 20-60%
Up to 5% go on to empyema
Suspect empyema if effusion enlarging or becomes loculated
Resolution
Delayed with advancing age and involvement of multiple lobes
Faster resolution in nonsmokers and outpatients
All patients > 40 years old (or younger smokers) should have follow-up until resolution
2% of hospitalized patients with CAP will have bronchogenic carcinoma
50% of these cancers diagnosed on initial chest radiograph
50% diagnosed as failure of resolution on follow-up
Expected time table
50% see resolution in 2 weeks; 66% in 4 weeks; 75% in 6 weeks
Mortality associated with 2 radiographic abnormalities: Bilateral pleural effusions and multilobar disease
Recurrent pneumonia
10-15% of hospitalized patients with CAP have recurrence within 2 years
Same location suggests bronchial obstruction or aspiration as etiology
Different location in otherwise healthy patient, evaluate for immunodeficiency
DIFFERENTIAL DIAGNOSIS
Cardiogenic Pulmonary Edema
Cardiomegaly and pleural effusions
Consolidation usually gravitationally dependent
Smooth septal thickening
Hemorrhage
Patients usually anemic and often have hemoptysis
Aspiration
May have predisposing condition such as esophageal motility disorder
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree