CHAPTER 115 Computed Tomographic Angiography of the Lower Extremities
Computed tomographic angiography (CTA) is at the forefront of noninvasive assessment of the peripheral arteries (CTA runoff).1 The advantage of CTA over catheter angiography is the absence of complications attributed to its more invasive predecessor, such as pseudoaneurysm and arteriovenous fistula.2 In addition, CTA requires a shorter stay for the patient, is less costly than catheter angiography, and has the potential to be more cost-effective than magnetic resonance angiography (MRA).3
With the aid of postprocessing tools now available, CTA is able to provide the interpreting physician and vascular surgeon with information concerning the site of obstruction, extent of vascular disease, and strategy for the appropriate type of vascular intervention.4
TECHNICAL REQUIREMENTS
An appropriate CTA protocol must provide both large field of view coverage and spatial resolution optimized for maximal contrast agent bolus enhancement of the arterial tree while minimizing ionizing radiation exposure and contrast agent dose.1
The individual requirements are as follows:
TECHNIQUES
Indications
By far, the most common indication is peripheral arterial disease (also known as peripheral arterial occlusive disease) in both the acute and chronic setting and in patients for follow-up and surveillance after surgical or percutaneous revascularization (Figs. 115-6 and 115-7).
Contraindications
Renal Impairment
The ultimate decision to administer an intravenous contrast agent is a shared one between the interpreting physician and the referring physician after informed consent of the patient in the event of renal impairment. The timing of dialysis in relation to the time of the scan is of importance. MRA is an option and may have to be performed without intravenous gadolinium-chelate contrast agent if the patient is at risk for development of nephrogenic systemic fibrosis (e.g., glomerular filtration rate less than 30 mL/min/1.73 m2).11
Orthopedic Hardware or High-Attenuation Object
Although it is not technically a contraindication, the artifact resulting from a high-attenuation object12 may obscure the artery of interest and limit the utility of the examination. Catheter angiography may be required because MRI may also be inflicted with significant artifact in such situations (Fig. 115-8).
Technique Description
Technique involves image acquisition and contrast agent administration.
Image Acquisition
Field of View
The field of view must answer the clinical question and provide information about associated vascular pathologic changes that would affect management. In the case of peripheral arterial occlusive disease, such as in patients with claudication, this involves the assessment of the abdominal aorta to assess the inflow and to exclude coexisting abdominal aortic aneurysm (Fig. 115-9).
An initial image through the abdomen and pelvis before the administration of the contrast agent is followed by arterial phase images from the celiac artery origin to the toes in a single acquisition. An immediate second acquisition is prudent through the calves, particularly with the newer scanners, in which outrunning of the contrast bolus can be a problem. Venous phase images are not routine and are obtained as clinically necessary. Breath-hold is required for the acquisition through the abdomen and pelvis.1,13
It is important to keep the patient’s knees and legs together, close to the isocenter. Excessive plantar flexion can erroneously depict occlusion of the dorsalis pedis and should be avoided.14
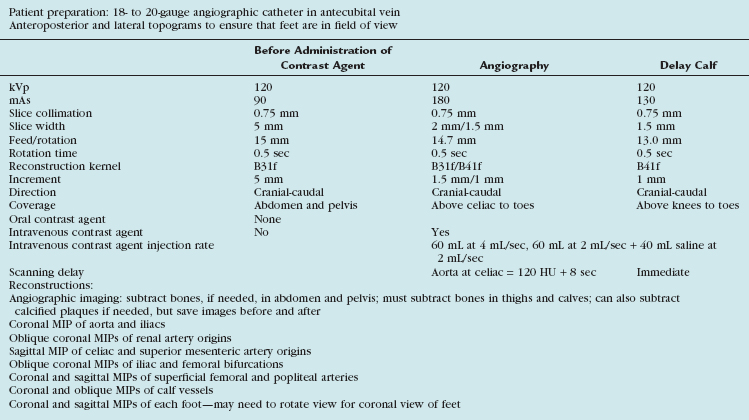
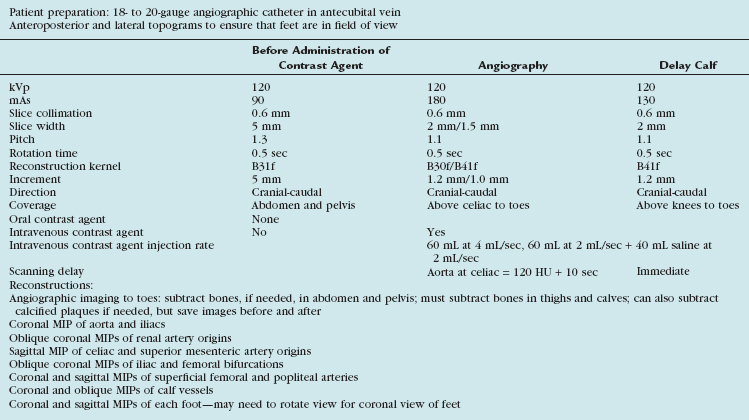
Scanning Protocols
The acquisition parameters depend on the number of detectors and are vendor specific (Tables 115-1 and 115-2). Regardless, the scan time should be such that the entire arterial tree of interest is covered in a reasonable time during which the arteries remain maximally opacified (i.e., in the first and single pass of contrast bolus). With the latest multidetector CT scanners, this does not involve a tradeoff between spatial resolution and z-axis coverage. With the 4-detector CT, a choice usually needs to be made, as will be explained.
Background Principles
Further discussion of this area involves recapitulation of some concepts.
Increasing the pitch results in the following:
A pitch greater than 1 broadens the slice sensitivity profile and in essence increases the effective section thickness.12
The optimal number of detectors that can provide sub-millimeter isotropic spatial resolution and coverage in a reasonable time without outrunning the bolus or incurring venous enhancement is 16 detectors. For proper visualization of the suprageniculate arteries in the absence of heavy calcification, a 4-detector scanner with 2.5-mm detector width can suffice. As a general rule, the larger the detector configuration, the lower the scanning pitch and the slower the gantry rotation speed.1

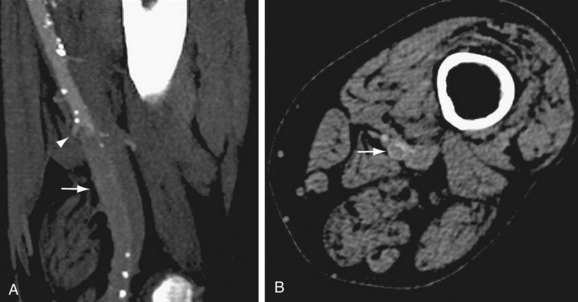
 FIGURE 115-1
FIGURE 115-1
 FIGURE 115-2
FIGURE 115-2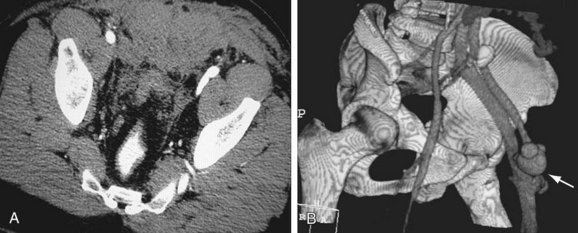
 FIGURE 115-3
FIGURE 115-3
 FIGURE 115-4
FIGURE 115-4
 FIGURE 115-5
FIGURE 115-5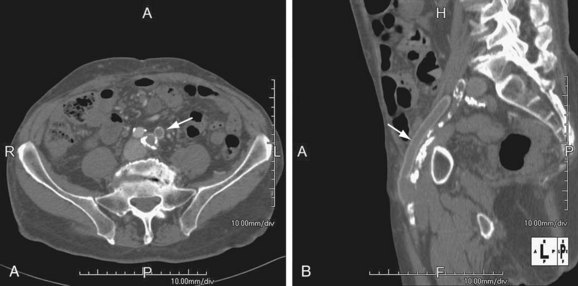
 FIGURE 115-6
FIGURE 115-6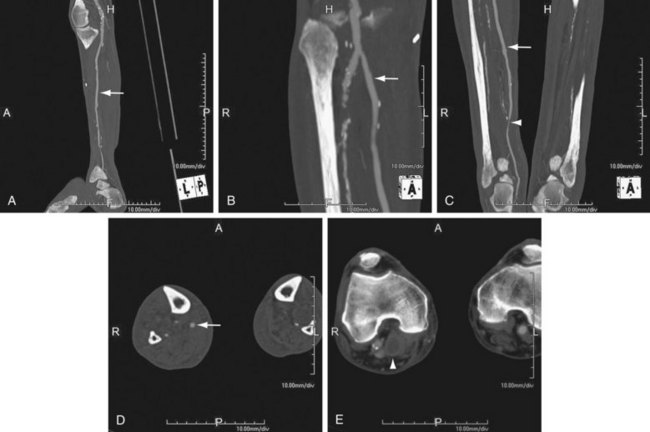
 FIGURE 115-7
FIGURE 115-7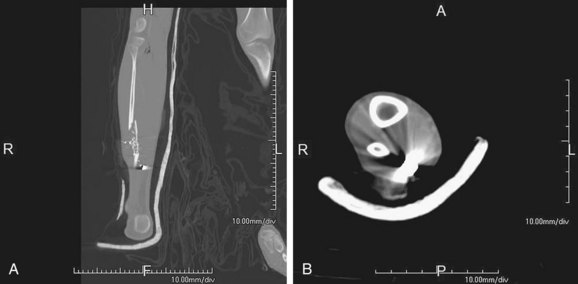
 FIGURE 115-8
FIGURE 115-8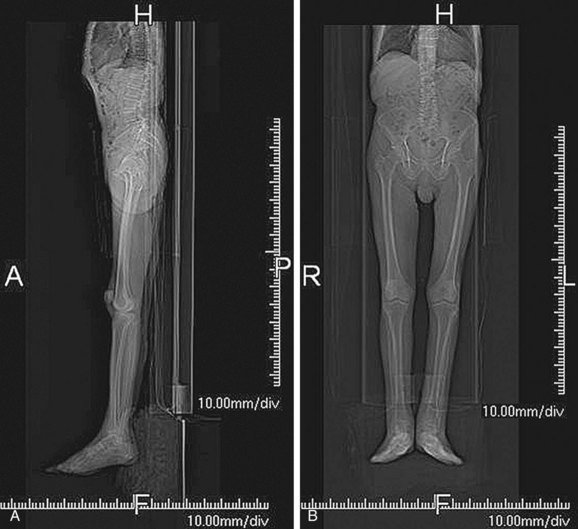
 FIGURE 115-9
FIGURE 115-9