1 Congential Disorders Abnormal communication between a pulmonary artery or arteriole and a pulmonary vein or venule. Rare Usually congenital, rarely acquired (traumatic) CT, CTA. Round or lobulated opacity surrounded by normal-appearing tissue; lesions with larger caliber feeding and draining vessels typically have a vascular pedicle extending toward the hilum. Findings are similar to radiography and include a round or lobulated lesion Round or lobulated lesion with a vascular pedicle. Usually the lesion is an asymptomatic incidental finding; hypoxemia and signs of heart failure occur only with a high shunt volume Balloon embolization, coiling, or resection. In Osler–Weber–Rendu disease the course and prognosis depend on the underlying disorder. Diagnosis Fig. 1.1 AVM in Osler– Weber–Rendu disease. CT (MIP) shows multi-locular tortuous and expanded vascular structures with shunt connections in the periphery that were not visualized on the chest radiograph to this degree of detail.
Arteriovenous Malformation (AVM)
Definition
 Epidemiology
Epidemiology
 80–90% occur in the setting of hereditary hemorrhagic telangiectasia (Osler–Weber–Rendu disease).
80–90% occur in the setting of hereditary hemorrhagic telangiectasia (Osler–Weber–Rendu disease).
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
 Sporadic, usually solitary
Sporadic, usually solitary  Osler–Weber–Rendu disease usually involves multiple lesions
Osler–Weber–Rendu disease usually involves multiple lesions  An arterial feeder and draining vein are usually present.
An arterial feeder and draining vein are usually present.
Imaging Signs
 Modality of choice
Modality of choice
 Radiographic findings
Radiographic findings
 CT findings
CT findings
 The vascular relationship is often demonstrated only on cine mode, in which the diagnosis can be made by interactive observation
The vascular relationship is often demonstrated only on cine mode, in which the diagnosis can be made by interactive observation  Plain scans show density values
Plain scans show density values  Enhancement typical of vascular structures occurs after contrast administration.
Enhancement typical of vascular structures occurs after contrast administration.
 Pathognomonic findings
Pathognomonic findings
Clinical Aspects
 Typical presentation
Typical presentation
 One-third of patients have a history of transient ischemic attack or stroke (venous thrombi) or cerebral abscesses (bypassing of the pulmonary capillary filter).
One-third of patients have a history of transient ischemic attack or stroke (venous thrombi) or cerebral abscesses (bypassing of the pulmonary capillary filter).
 Therapeutic options
Therapeutic options
 Course and prognosis
Course and prognosis
 What does the clinician want to know?
What does the clinician want to know?
 Location
Location  In Osler–Weber–Rendu disease it may be advisable to obtain CT scans of carriers in the family for early detection of pulmonary arteriovenous malformation.
In Osler–Weber–Rendu disease it may be advisable to obtain CT scans of carriers in the family for early detection of pulmonary arteriovenous malformation.
Differential Diagnosis
Pulmonary nodule | – Does not show enhancement typical of vascular structures – Feeding vessels are not functionally expanded in contrast to AVM |
Tips and Pitfalls
Can be misinterpreted as a pulmonary nodule or suspected malignancy.
Selected References
Langer R, Langer M. Value of CT in the diagnosis of pulmonary arteriovenous shunts. Cardiovasc Intervent Radiol 1984; 7: 277–279
White RI et al. Pulmonary arteriovenous malformations: diagnosis and transcatheter embolotherapy. J Vasc Interv Radiol 1996; 7: 787–804
Shunt
Definition
 Epidemiology
Epidemiology
Most common causes include defect with left-to-right shunt, atrial septal defect, ventricular septal defect, and patent ductus arteriosus.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Left-to-right shunt increases the volume of blood in the pulmonary circulation  Atrial septal defect is a low-pressure shunt with volume overload; it leads to increased vascular resistance in the pulmonary circulation with pulmonary arterial hypertension only after a long time
Atrial septal defect is a low-pressure shunt with volume overload; it leads to increased vascular resistance in the pulmonary circulation with pulmonary arterial hypertension only after a long time  Ventricular septal defect is a high-pressure shunt with rapidly increasing vascular resistance and pulmonary arterial hyper-tension; shunt flow reverses when pressure is equalized (Eisenmenger reaction)
Ventricular septal defect is a high-pressure shunt with rapidly increasing vascular resistance and pulmonary arterial hyper-tension; shunt flow reverses when pressure is equalized (Eisenmenger reaction)  Patent ductus arteriosus is a high-pressure shunt with hemodynamic effects similar to ventricular septum defect.
Patent ductus arteriosus is a high-pressure shunt with hemodynamic effects similar to ventricular septum defect.
Imaging Signs
 Modality of choice
Modality of choice
Echocardiography, MRI.
 Radiographic findings
Radiographic findings
Findings are positive only where shunt volume exceeds 40%; the findings then include a prominent pulmonary artery segment as well as prominent lung arteries with a slender aorta  Pulmonary vascular structures are enlarged
Pulmonary vascular structures are enlarged  Normal or slightly widened heart silhouette
Normal or slightly widened heart silhouette  Abrupt changes in vascular caliber and signs of right heart strain only occur with pulmonary arterial hypertension
Abrupt changes in vascular caliber and signs of right heart strain only occur with pulmonary arterial hypertension  Ventricular septal defect and patent ductus arteriosus are associated with enlargement of the left atrium, and patent ductus arteriosus with a dilated ascending aorta.
Ventricular septal defect and patent ductus arteriosus are associated with enlargement of the left atrium, and patent ductus arteriosus with a dilated ascending aorta.
 MRI findings
MRI findings
Visualizes shunt location and morphology  Allows estimation of shunt volume (quantification of blood flow in the ascending aorta and pulmonary trunk).
Allows estimation of shunt volume (quantification of blood flow in the ascending aorta and pulmonary trunk).
 Pathognomonic findings
Pathognomonic findings
Prominent central and peripheral vascular structures.
Clinical Aspects
 Typical presentation
Typical presentation
Shunts with minimal hemodynamic effects are often asymptomatic or minimally symptomatic  Clinically relevant shunts lead to right heart failure in atrial septal defect and left heart failure in ventricular septal defect.
Clinically relevant shunts lead to right heart failure in atrial septal defect and left heart failure in ventricular septal defect.
 Therapeutic options
Therapeutic options
Early correction.
 Course and prognosis
Course and prognosis
Prognosis is good with early correction  Unfavorable with pulmonary arterial hypertension and Eisenmenger reaction.
Unfavorable with pulmonary arterial hypertension and Eisenmenger reaction.
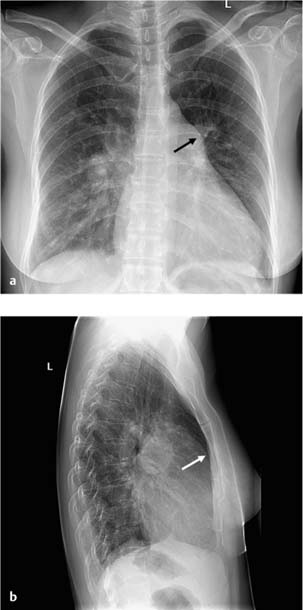
Fig. 1.2 Atrial septal defect (ostium secundum) with a 60% left-to-right shunt in a 41-year-old woman. The plain chest radiographs show a widened heart silhouette with signs of right heart strain (prominent pulmonary trunk and broad area of contact between the anterior wall of the heart and the sternum) and a conspicuously narrow aorta. In contrast, the hila are prominent with increased pulmonary vasculature without signs of redistribution.
 What does the clinician want to know?
What does the clinician want to know?
Shunt location and morphology  Shunt volume
Shunt volume  Valvular and ventricular function
Valvular and ventricular function  Signs of heart failure.
Signs of heart failure.
Differential Diagnosis
Increased cardiac output | – Hyperthyroidism – Polycythemia – Hypervolemia |
Tips and Pitfalls
Defects with “small” shunt volume (< 50%) are not detectable on plain radiographs.
Selected References
Baron MG, Book WM. Congenital heart disease in the adult. Radiol Clin North Am 2004; 42: 675–690
Steiner RM, et al. Congenital heart disease in the adult patient: The value of plain film chest radiology. J Thorac Imaging 1995; 10: 1–25
Wang ZJ et al. Cardiovascular shunts: MR imaging evaluation. Radiographics 2003; 23: 181–194
Scimitar Syndrome
Definition
Anomalous, vertically coursing right pulmonary vein, often associated with other congenital malformations: Pulmonary venolobar syndrome  Congenital hypoplastic lung
Congenital hypoplastic lung  Pulmonary hypoplasia with atypical pulmonary venous drainage
Pulmonary hypoplasia with atypical pulmonary venous drainage  Pulmonary sequestration.
Pulmonary sequestration.
 Epidemiology
Epidemiology
Rare (2 : 100 000).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree