CHAPTER 3 Coronary Anatomy
Multidetector CT has become an important tool for noninvasive evaluation of cardiovascular structures.1 With advances in multidetector CT technology, the role of imaging has progressed from detection and quantification of the calcium score on noncontrast CT to detection of luminal stenoses, and detection and characterization of plaque composition on coronary CT angiography.2,3 Basic knowledge of the normal coronary arterial anatomy is essential for evaluation and interpretation of cardiac CT studies. Properly performed, coronary CT angiography provides high spatial resolution, three-dimensional data for detailed visualization of the coronary arteries, which are typically small, and rapidly moving, and have tortuous and complex anatomic arrangements. The anatomy of the coronary arteries and their normal variants is well described using conventional coronary angiography. The cross-sectional nature of CT has the benefit, however, of more precisely displaying the spatial relationship of coronary arterial and venous anatomy with respect to adjacent cardiac structures.
Multidetector CT is a continually evolving technique that in recent years has been mainly used to evaluate the coronary arteries. Less attention has been paid to the coronary venous system until more recently.4,5 Evaluation of the cardiac venous anatomy is important for preprocedural planning of percutaneous resynchronization therapy and treatment of resistant ventricular arrhythmias. In this chapter, we discuss the detailed normal anatomy of the coronary arteries and their normal variants and the anatomy of the cardiac veins.
CORONARY ARTERIES
The definition of the abnormal versus normal anatomy of the coronary arteries presents a complex problem. Angelini and colleagues6,7 have proposed the following terms to define these categories: normal—any morphologic feature observed in greater than 1% of an unselected population; normal variant—an alternative, relatively unusual, morphologic feature seen in greater than 1% of the population; and anomaly—a morphologic feature (e.g., number of ostia, proximal course, termination) rarely encountered (<1%) in the general population. The normal coronary arteries and their variations can be described in terms of their ostia (with respect to their number, location, size, and angle of origination), the size and length of the coronary arteries, their proximal and mid course (intramyocardial bridging), arteriolar ramifications, and terminations.
NORMAL CORONARY ARTERY ANATOMY
There are two coronary arteries, the right coronary artery (RCA) and left coronary artery (LCA), which originate from their respective sinuses of Valsalva—the RCA from the right sinus of Valsalva and the LCA from the left sinus of Valsalva (Fig. 3-1). The right sinus of Valsalva is located anteriorly and the left sinus of Valsalva posteriorly and to the left. The third sinus of Valsalva, located posteriorly and to the right, does not give rise to a coronary artery, and is referred to as “noncoronary cusp/sinus.” There may be variations in the number, shape, and location of coronary ostia or origins of the coronary arteries, most of which are of no clinical significance.
The coronary ostia are usually located in the upper third of the respective sinus of Valsalva. Ostia located near the aortic valve commissures, ostia located in the posterior (noncoronary) sinus, and ostia showing a high takeoff are considered abnormal. The high takeoff of the coronary artery may reduce diastolic coronary artery blood flow, and the patient may become symptomatic.8 High takeoff of a coronary artery may result in a long intramural course which could be potentially pathologic (Fig. 3-2).
In terms of the number of the coronary ostia, two ostia are considered normal, one in the respective sinus for the RCA and LCA; however three or four are considered as normal variants, such as a separate origin of a conal branch from the aorta (prevalence 11.6%)9 or absence of the left main (LM) coronary artery with the left anterior descending artery (LAD) and left circumflex artery (LCX) having separate origins from the aorta. An absent LM is considered a benign anomaly. A separate origin of the sinus node artery from the aorta has a prevalence of 0.2%.9 The single coronary artery and ectopic origin of the coronary arteries from the aorta and pulmonary artery are considered as anomalous and are discussed in Chapter 33.
Right Coronary Artery
On axial images, the RCA arises from the right sinus of Valsalva, inferior to the origin of the LCA (Fig. 3-3). It courses anteriorly and inferiorly under the right atrial appendage along the right atrioventricular (AV) groove, toward the acute margin of the heart, where it turns posteriorly and inferiorly toward the crux of the heart and divides into the posterior descending coronary artery (PDA) and the posterolateral ventricular branch (PLB) (Fig. 3-4; see Fig. 3-3). The RCA supplies the right atrium, right ventricle, posterior third of the interventricular septum, and sinoatrial and AV nodes.
In 50% to 64% of the population, the conus branch arises as the first branch of the RCA (Fig. 3-5A).9 The conus may arise from the ostial RCA in 22.3% or separately from the aorta in 11.6% of the population (Fig. 3-5B).9 The conus branch courses anteriorly and to the right and supplies the pulmonary outflow tract. Rarely, this branch can arise from the LCA.
The sinoatrial nodal artery is the second branch that arises from the proximal RCA in 65.4%, immediately distal to the RCA origin (Fig. 3-6A). In 16.6% of cases, the sinoatrial nodal artery arises from the LCX (Fig. 3-6B); in 9.2%, it arises from the RCA and the LCX; in 0.2%, it arises from the LCX and the pulmonary artery; and in 0.2%, it arises directly from the aorta.9 This artery courses toward the superior vena cava near the cranial aspect of the interatrial septum.
The next branches of the RCA are the marginal branches that supply the right ventricular myocardium (see Figs. 3-3 and 3-4). The acute marginal artery comes off the acute margin of the heart and courses anteriorly and to the right, anterior to the right ventricle. The acute marginal branches supply the free wall of the right ventricular myocardium. In 10% to 20% of patients, an acute marginal branch runs on the diaphragmatic surface of the heart to supply the distal posterior interventricular septum. After the RCA gives off the acute marginal branches, it continues in the right AV groove toward the diaphragmatic aspect of the heart. At the crux of the heart, the RCA makes a U-turn and branches into the PDA and PLB (see Fig. 3-4).
The PDA is of variable size and runs along the diaphragmatic surface in the posterior interventricular groove toward the inferior septum. Short septal branches arising perpendicularly from the PDA supply the posterior third of the septum and can connect with the septal branches from the LAD to form a collateral circulation. The PLB runs in the posterior left AV groove and gives off multiple branches that supply the posterior and inferior wall of the left ventricle (see Fig. 3-4). The average angle between the PDA and PLB is 53 ± 27 degrees.10 Within 1 to 2 cm of the crux, the PLB runs on the diaphragmatic surface of the left ventricle parallel to the PDA to supply the posterolateral diaphragmatic surface of the left ventricle. Here the RCA can serve as a collateral for an occluded LCX. Also close to the crux of the heart, just distal to the PDA origin, the RCA gives rise to a small AV nodal artery that supplies the AV node of the conduction system (Fig. 3-7). The AV nodal artery arises from the LCX in a left dominant system.
Left Coronary Artery
On axial images, when scrolling from the cranial to caudal direction, the LCA or LM is the first coronary artery that is seen arising from the left sinus of Valsalva (Fig. 3-8). It courses to the left, beneath the left atrial appendage and posterior to the right ventricular outflow tract, before branching into the LAD and the LCX (Fig. 3-9). The LM varies in length from 5 to 25 mm (mean 13.5 mm), and its diameter ranges from 2 to 5.5 mm (mean 4 mm) (Fig. 3-10).7,11 In 543 patients, Cademartiri and colleagues9 reported a length of less than 1 cm in 41.6%, 1 to 2 cm in 47.3%, and greater than 2 cm in 7% of patients. Pflederer and coworkers10 examined average angles of coronary bifurcations in 100 patients at four branch points: LAD/LCX, LAD/first diagonal branch, LCX/first obtuse marginal branch (OM1), and PDA/right posterolateral branch. The average LAD/LCX angle was reported as 80 ± 27 degrees. The interobserver variability of bifurcation angle measurements by contrast-enhanced 16-slice multidetector CT was significantly better (r = 0.91) than invasive angiography (r = 0.62).10 A normal variation in the anatomy is a true trifurcation of the LM, when the middle branch between the LAD and LCX is called the ramus intermedius (RI).9,12 The LM may be absent in fewer than 1% of the population; in these cases, the LAD and LCX arise separately from the aorta.7
Left Anterior Descending Artery
The LAD runs anteriorly and inferiorly in the anterior interventricular groove to the apex of the heart, and supplies the anterior and anterolateral wall of the left ventricular myocardium and the anterior two thirds of the interventricular septum (Figs. 3-11 and 3-12; see Fig. 3-10). In approximately 82% of cases, the LAD curves around the cardiac apex to supply part of the inferior wall of the left ventricle. In 7%, it may not reach the apex of the heart, and in about 11% of cases, the LAD terminates in the distal anterior interventricular groove or even more proximally.13 In such cases, the distal territory may be supplied by an unusually long diagonal branch or by RCA branches that traverse the posterior interventricular groove or the inferior surface of the heart, a normal variant.14 This is one of the potential collateral routes if either the RCA or the LAD is occluded.
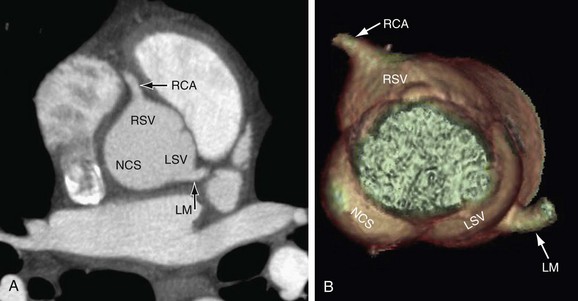
 FIGURE 3-1
FIGURE 3-1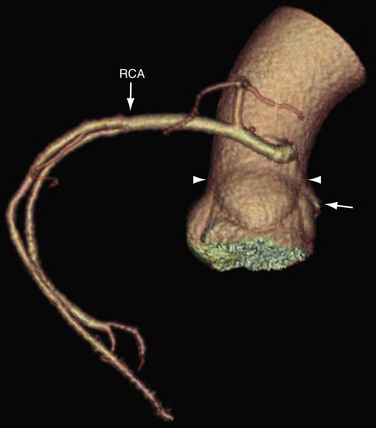
 FIGURE 3-2
FIGURE 3-2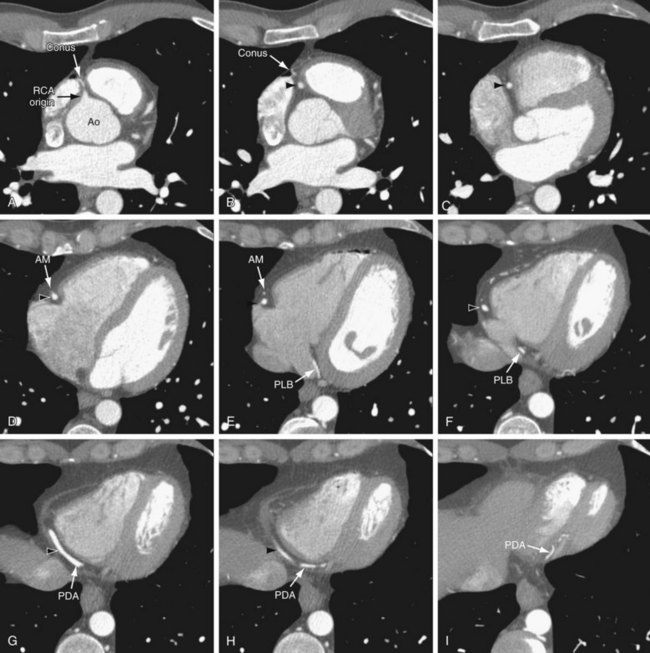
 FIGURE 3-3
FIGURE 3-3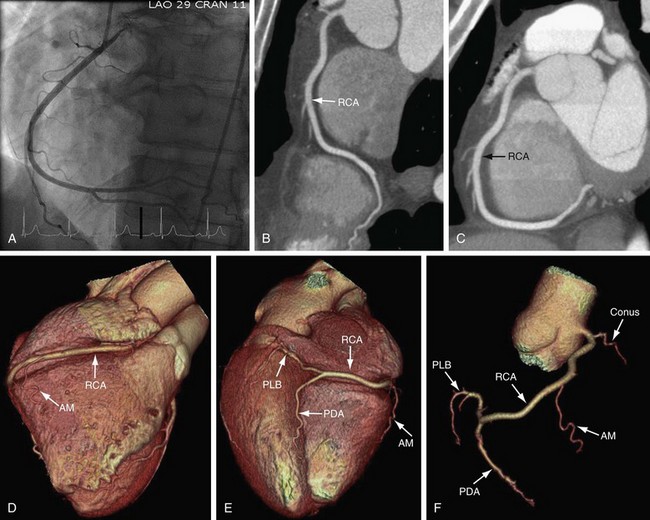
 FIGURE 3-4
FIGURE 3-4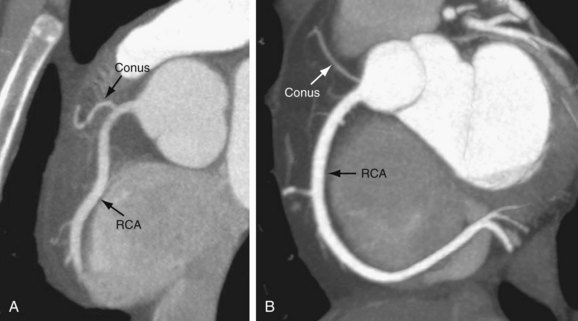
 FIGURE 3-5
FIGURE 3-5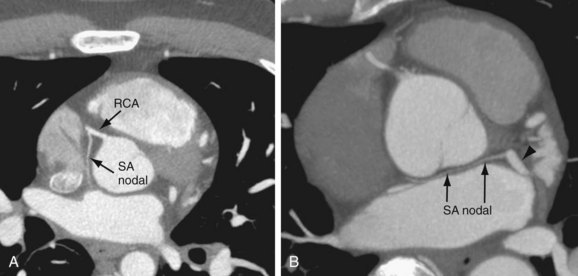
 FIGURE 3-6
FIGURE 3-6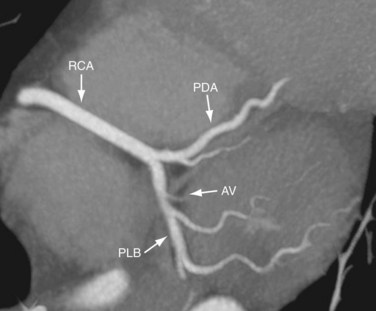
 FIGURE 3-7
FIGURE 3-7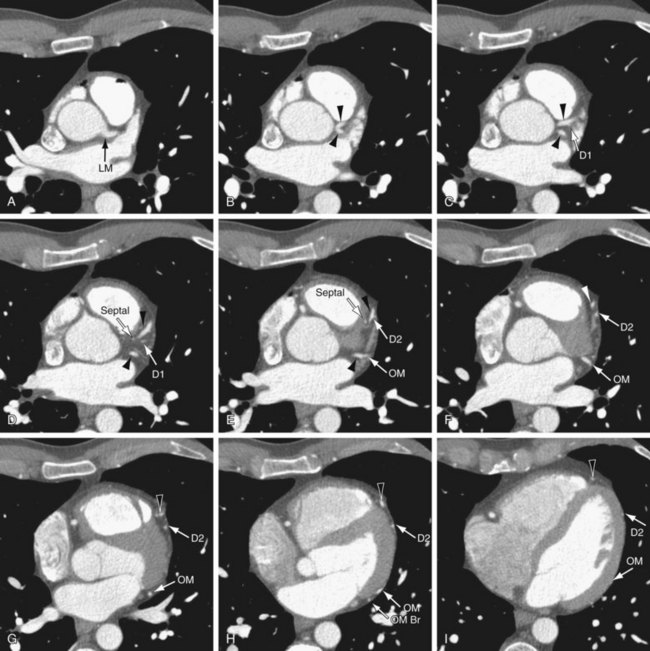
 FIGURE 3-8
FIGURE 3-8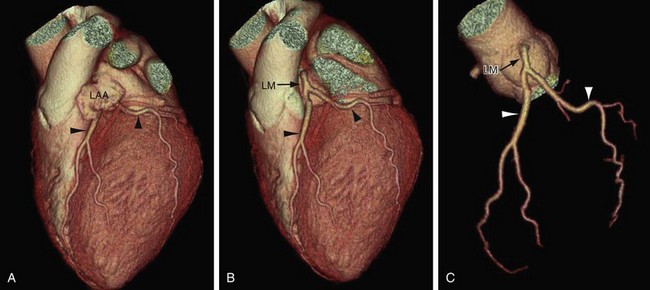
 FIGURE 3-9
FIGURE 3-9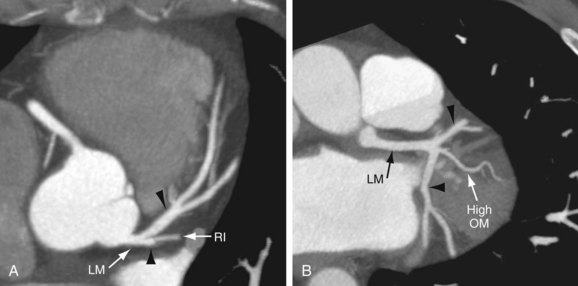
 FIGURE 3-10
FIGURE 3-10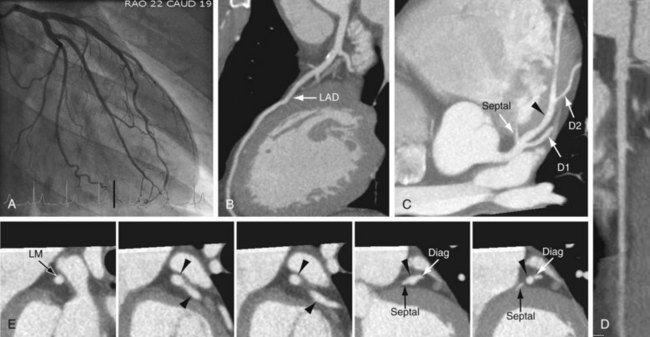
 FIGURE 3-11
FIGURE 3-11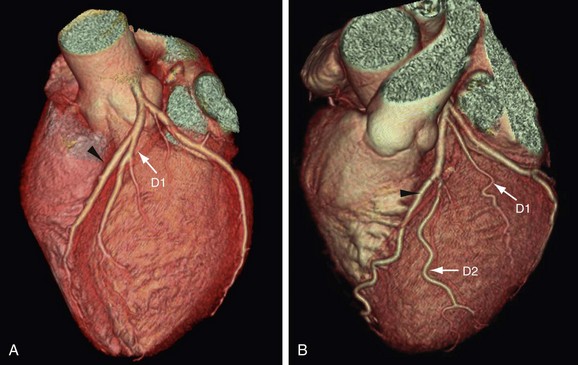
 FIGURE 3-12
FIGURE 3-12


