Coronary Artery Disease
The definition of coronary artery disease is not uniform. Often any atherosclerotic plaque that is present in the coronary system, even if completely asymptomatic, will be labeled as coronary artery disease. Most physicians use the term if at least one flow-limiting stenosis is present, and the typical threshold assumed for a flow-limiting stenosis is a diameter reduction of 50%. Finally, some physicians argue that the term coronary artery disease should be reserved for individuals who have clinical symptoms because of the presence of coronary artery stenoses.
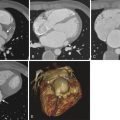
Similarly, there is no immediate relationship between the buildup of atherosclerotic plaque and narrowing of the coronary lumen, and not even a uniform understanding of the term stenosis ( Fig. 38-1 ). When coronary atherosclerotic plaque develops, it is usually accompanied by a process called “remodeling,” which expresses the fact that the overall vessel cross section typically dilates to compensate for the plaque volume. Rather large plaques can be present without substantial luminal narrowing. Thus the degree of stenosis when assessed by angiography (“luminal stenosis”) will often be relatively mild, because the lumen is only slightly narrowed. However, if the lesion is visualized in cross section, for example by histologic examination or tomographic imaging (intravascular ultrasonography or corresponding reformats in cardiac computed tomography [CT]), the degree of stenosis that is obtained by comparing the area of the entire vessel cross section to the area of the remaining lumen can be substantial.

If, on the other hand, the process of remodeling fails to compensate for the growing plaque, the coronary artery lumen will be narrowed substantially, and angiographically detectable luminal stenosis is the consequence. Hence the degree of stenosis determined by investigating the coronary lumen will typically be less than stenosis determined by comparing vessel cross section to luminal cross section.
Detection of Coronary Artery Disease—Ischemia Versus Anatomy
It is important to note that clinically there are two different concepts for the detection of coronary artery stenoses in patients. On one hand, tests that determine ischemia or wall motion abnormalities during stress are often used (such as nuclear perfusion imaging, stress magnetic resonance imaging or stress echocardiography). It is important to note that the functional consequences of stenoses are not uniform and are difficult to predict. Even stenoses of more than 50% luminal reduction are not always associated with downstream ischemia, and the degree of stenosis is a relatively poor predictor of ischemia. Inducible ischemia has been demonstrated to be of prognostic significance, and clinical guidelines suggest ischemia testing as the first step in the workup of coronary artery disease. If no ischemia is present, there is relatively little to gain from revascularization, and hence further testing is generally not suggested.
Another method of diagnosing coronary artery disease is direct visualization of the coronary artery system and coronary stenoses, which is possible through invasive coronary angiography and coronary CT angiography ( Fig. 38-2 ). Recently it has also become possible to use volumetric magnetic resonance imaging sequences for coronary imaging. Some applications exist in the context of coronary anomalies and Kawasaki disease, but coronary magnetic resonance imaging is not clinically used at the moment in patients with known or suspected coronary atherosclerotic disease.

Coronary Artery Imaging by Invasive Angiography and Computed Tomography
Invasive Coronary Angiography
In the vast majority of cases, invasive coronary angiography will be used to visualize the coronary arteries and detect coronary artery stenoses. It is an invasive procedure but relatively safe and with very few contraindications. A vascular access is required, which is typically between 4 French (Fr) and 6 Fr. The transfemoral access is used most frequently, but transradial procedures enjoy increasing popularity. Approximately 20 to 100 mL of iodinated contrast agent is required. Two main aspects speak for invasive coronary angiography as compared to CT angiography for the detection of coronary artery stenoses: the accuracy, for clinical purposes, can be considered to be close to 100%, and the method fails in almost no patients. If performed, a diagnostic result is almost completely certain, except for extremely infrequent cases with access site problems or inability to engage the coronary arteries because of massive aortic enlargement or ectopic position of the coronary ostia. Potential disadvantages include the invasiveness, relatively high cost, and somewhat limited availability because not every hospital and practice has cardiac catheterization services.
Invasive coronary angiography will be the method of choice in all patients in whom it is questionable whether CT angiography will provide artifact-free images, either because of patient characteristics such as heart rate or obesity with poor breath-holding capability (see later discussion) or because of suspected very diffuse and severe coronary atherosclerosis. Further, invasive coronary angiography offers the possibility for immediate intervention. Hence it is the method of choice in patients with a high pretest likelihood of disease, whether based on clinical presentation or previous positive stress test results. In most cases, diagnostic coronary angiography can be immediately followed by revascularization.
Coronary Computed Tomography Angiography
Coronary CT angiography is a reasonable alternative to invasive coronary angiography if the clinical suspicion of stenoses is not very high (and hence the likelihood that revascularization will be required is low). Some further prerequisites should be fulfilled, including the availability of adequate hardware and software for coronary CT imaging. Importantly, the performing physician and staff should have sufficient expertise in data acquisition and interpretation, and patient characteristics should make a fully evaluable CT angiography examination highly probable ( Table 38-1 ). The lack of any invasiveness, immediate ambulation, and lower cost are advantages of CT angiography as compared to invasive coronary angiography. The availability of coronary CT angiography as a noninvasive test has renewed interest in using direct anatomic visualization as a first-line diagnostic tool for coronary artery disease (as opposed to ischemia testing). However, the fact that not all stenoses produce ischemia (and hence not all stenoses require revascularization) has to be kept in mind. The threshold for noninvasive visualization of the coronary arteries should not be set too low.
| Institutional Characteristics |
|
| Patient Characteristics |
|
Scenarios that Require Diagnosis of Coronary Artery Disease
Clinically five major scenarios raise the question of the presence, extent, and distribution of coronary atherosclerosis and stenoses and may be reasons to visualize the coronary arteries:
- 1.
Stable chest pain
- 2.
Acute chest pain and acute coronary syndromes
- 3.
Impaired left ventricular function
- 4.
Risk stratification in asymptomatic individuals
- 5.
Imaging of the coronary arteries in the context of coronary interventions (percutaneous coronary revascularization)
The majority of patients in whom imaging of the coronary arteries is considered are those with suspected coronary artery disease because of symptoms that occur during exercise (stable chest pain) or at rest (acute chest pain).
Problem Solving
Stable Chest Pain
Patients with stable chest pain typically report angina or shortness of breath when they exercise, but complaints vary substantially and can be rather nonspecific, especially in some patient groups such as diabetic patients. It is important to note that even in the presence of symptoms, the pretest likelihood of coronary stenoses being present varies substantially. Pretest likelihood is low in young persons and in women, and it is high in older persons and in men. Table 38-2 provides an estimate of pretest likelihood of coronary artery stenoses depending on age, sex, and typicality of symptoms.
| Age (yr) | Sex | Nonanginal Chest Pain (%) | Atypical Angina (%) | Typical Angina (%) |
|---|---|---|---|---|
| 30-39 | Male | 4 | 34 | 76 |
| Female | 2 | 12 | 26 | |
| 40-49 | Male | 12 | 51 | 87 |
| Female | 3 | 22 | 55 | |
| 50-59 | Male | 20 | 65 | 93 |
| Female | 7 | 31 | 73 | |
| 60-69 | Male | 27 | 72 | 94 |
| Female | 14 | 51 | 86 |
The preferred clinical approach in patients with stable chest pain and suspected coronary artery disease is to perform a stress test to assess myocardial ischemia. The choice of stress testing (single photo emission CT [SPECT] myocardial perfusion imaging, magnetic resonance myocardial perfusion, stress echocardiography, or exercise electrocardiography [ECG]) will depend on local preference and patient characteristics. If stress test results are positive and indicate a relevant extent of ischemia, invasive coronary angiography is typically recommended to clarify the presence and extent of coronary artery stenoses. Medical management, percutaneous coronary intervention, and bypass surgery are treatment options when coronary artery stenoses are found.
Coronary CT angiography can be used to visualize the coronary arteries and detect coronary artery stenoses. However, its use has to be carefully considered. One important consideration is the pretest likelihood of disease. When pretest likelihood for coronary artery disease is high, catheter-based invasive coronary angiography is the preferred test because it provides the option for immediate revascularization. On the other hand, when pretest likelihood is low, coronary CT angiography may be appropriate because it has a high negative predictive value and therefore allows the clinician to reliably rule out coronary artery stenoses. A second consideration of major importance is the question whether the patient is a suitable candidate for coronary CT angiography, will provide diagnostic image quality, and, especially if young, can be imaged with reasonably low radiation exposure. Table 38-3 lists situations in which coronary CT angiography is considered appropriate for the identification of stable coronary artery disease, according to expert consensus.
| Clinical Situation | Appropriateness |
|---|---|
| Nonacute Symptoms Possibly Representing an Ischemic Equivalent—No Stress Test Done | |
| ECG interpretable and able to exercise | |
| Uncertain |
| Appropriate |
| Inappropriate |
| ECG uninterpretable or unable to exercise | |
| Appropriate |
| Appropriate |
| Uncertain |
| Prior ECG Exercise Test | |
| Normal but continued symptoms | Appropriate |
| Abnormal | |
| Inappropriate |
| Appropriate |
| Inappropriate |
| Prior Stress Imaging Procedure | |
| Equivocal | Appropriate |
| Uncertain |
| Inappropriate |
| Appropriate |
| New or Worsening Symptoms With a Past Stress Imaging Study | |
| Appropriate |
| Uncertain |
| Patient With Previous Revascularization by CABG | |
| Appropriate |
| Inappropriate |
| Uncertain |
| Patient With Previous Revascularization by PCI | |
| Inappropriate |
| Uncertain |
| Appropriate |
| Inappropriate |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree