Cranial CT
Many cranial CT (CCT) examinations can be performed without injection of contrast medium: For instance, the differential diagnosis (DD) of cerebral bleeding versus infarction in patient with sudden onset of neurologic deficits does not require the administration of contrast medium. However, intravenous injection of contrast medium is necessary to detect an impaired blood-brain barrier (BBB) as found in tumors, metastases or inflammations.
Selection of the Image Plane
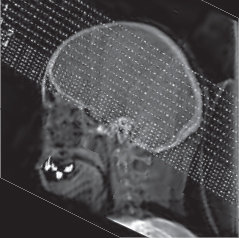
The desired image planes parallel to the orbitomeatal line are selected on the sagittal localizer image (topogram) ( Fig. 26.1 ). This is a readily reproducible line drawn from the supraorbital ridge to the external auditory meatus, allowing reliable comparison with follow-up CT examinations. The posterior fossa is scanned in thin sections (2-3 mm) to minimize beam hardening artifacts, and the supratentorial brain above the pyramids in thicker sections (5 mm).
The images are displayed as seen from below (caudal view) and consequently are laterally reversed, i.e., the left lateral ventricle is on the right and vice versa. Only CTs obtained for neurosurgical planning are often displayed as seen from above (right = right) since this cranial view corresponds to the neurosurgical approach for cranial trepanation.
Systematic Interpretation
Each examiner is free to find a preferred sequence for reviewing the images. This means that the examiner can choose between several acceptable approaches and is not restricted to a “one and only” strategy. However, staying with a consistent arrangement of the images to be interpreted has the advantage that fewer findings are overlooked, especially by the novice. The checklist below just contains recommendations that can serve as good guideline for the novice.
First, the size of the ventricles and extracerebral CSF spaces has to be evaluated to exclude a life threatening space-occupying process right away. Hereby, the patient’s age has to be considered because of age-related widening of the CSF spaces. Any blurring of the grey-white matter junction as manifestation of cerebral edema should be looked for (see below). If a pathologic change is suspected, the adjacent sections should be inspected to avoid any misinterpretation due to a partial volume effect (see Fig. 29.1 and Fig. 52.2 ).
Always use the legends on the front cover flap for this chapter. The listed numbers apply to all head and neck images. The subsequent pages provide you with a survey of the normal anatomy, followed by normal variants and the most frequent pathologic findings.
Checklist for Reading Cranial CT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree