Chapter 17 Cranial vault
Skull radiography has been in decline for many years. It is still in limited use for the investigation of some metabolic and bone disorders, and as part of the skeletal survey protocol for cases of suspected non-accidental injury (NAI). In cases of trauma, even where still used, fewer projections are recommended for a number of years – two rather than the ‘traditional’ three being advised.1
Why is this? The easy answer appears to be radiation protection – minimisation of dose.
In 1978 Eyes and Evans, in a study of 504 patients in two Liverpool teaching hospitals, found a very low yield of positive findings on plain skull radiographs, suggesting that they were of limited value in the management of patients with head injury.2 Both earlier and later studies in the USA agreed with these findings, the yield of fractures varying but with a low of 2.7% in agreement with the above UK study.3–5
Head injuries are the cause of around 700 000 hospital attendances each year in England and Wales.6 Imaging of the head injury patient is directed at detecting the nature of the underlying pathology; once this is accomplished the brain can be protected against greater damage. Optimal imaging is dependent on the nature of the injury, with evaluation of the brain normally being of paramount importance. The advent of computed tomography (CT) has had a massive impact on the diagnosis and treatment of traumatic head injury, allowing rapid non-invasive identification of both diffuse injury and surgically treatable lesions.
It should be noted that cervical spine injury is relatively common in comatose patients with head injury,7 hence it is important to exclude such an injury prior to mobilisation, the minimum examination being a high quality lateral examination C1–C7.
When the Royal College of Radiologists (RCR) guidelines were first produced, one purpose was to eliminate unnecessary skull radiographs, and they have been successful in reducing the number of skull images being performed. The current RCR guidelines6 adopt the Canadian CT head rule8 eliminating the need for radiography of the skull in trauma, except for where CT is unavailable, or in the case of NAI in children.
RCR guidance has been added to in the UK by guidance issued by the National Institute for Health and Clinical Excellence (NICE).9 Application of the Canadian Head CT Rule has been shown to be effective in the management of patients with minor head trauma, significantly reducing the amount of scans required in this group, but patients in the high- and medium-risk groups require CT.8
Given its ability to demonstrate bony detail as well as much greater detail of the underlying soft tissues within the cranial vault, CT is the investigation of choice in an increasing number of circumstances. Thus the use of skull radiography, particularly in trauma, has diminished greatly, but its use is not yet obsolete: indeed, in some countries skull radiography remains in widespread use.10 Consequently, it is still necessary for the radiographer to be competent in X-ray examination of the cranial vault.
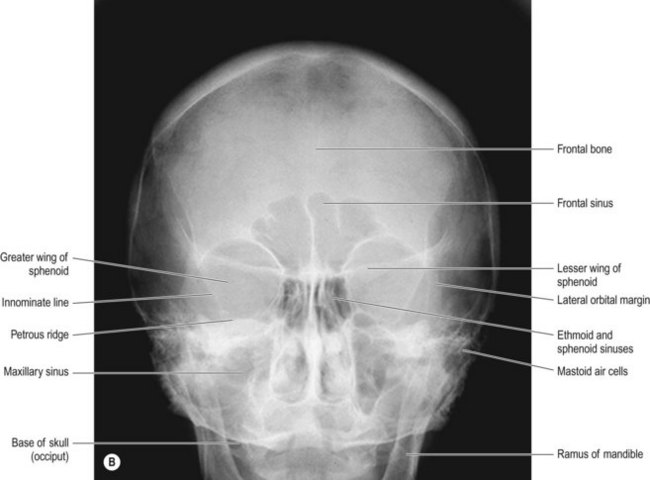
OF cranium (Fig.17.1A,B)
Image receptor (IR) is vertical; an antiscatter grid is employed
Positioning
• The patient is seated facing the IR, their forehead in contact with it
• The orbitomeatal baseline (OMBL) and median sagittal plane (MSP) are perpendicular to the IR. The MSP position can be checked by ensuring that the distances between both external auditory meati (EAMs) and the IR are equidistant
Beam direction and focus receptor distance (FRD)
There are a range of beam directions used, which affect the position of the petrous ridge on the image produced (see Ch. 16); 20° caudal angulation clears the ridge to the lowest border of the orbits and this angulation is probably that used most frequently, since it maximises the amount of vault shown above the maxilla
Criteria for assessing image quality
• Vertex of vault, inferior border of occiput, and the lateral margins of vault are demonstrated
• Superior border of petrous ridge shown level with superior orbital margins, if no angle is used. For techniques using beam angulation, the petrous ridge should appear halfway down the orbits for 10° caudal angle and at the bottom of the orbits for 20° angle
• Lateral borders of orbits equidistant from lateral borders of skull
• Sharp image showing the dense petrous ridge in contrast with the orbits and occiput, frontal bone in contrast with the adjacent air-filled sinuses
| Common errors | Possible reasons |
|---|---|
| Petrous ridge is seen above required level in relationship to orbits | Inadequate angle selected or OMBL used is incorrectly positioned (chin down too far) |
| Petrous ridge is seen below required level in relationship to orbits | Angle selected is too great or OMBL used is incorrectly positioned (chin not down enough) |
| Distance between lateral orbital margins is not equal | Rotation of the head; the orbit demonstrating the shortest distance between its lateral border and the lateral aspect of the vault coincides with the side towards which the head is rotated |