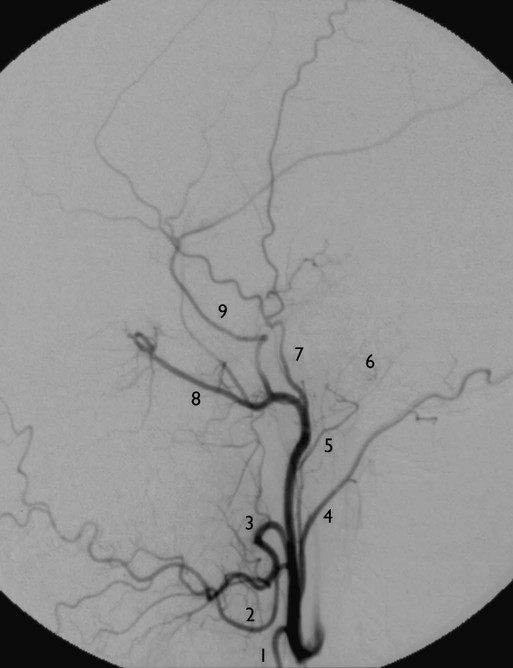
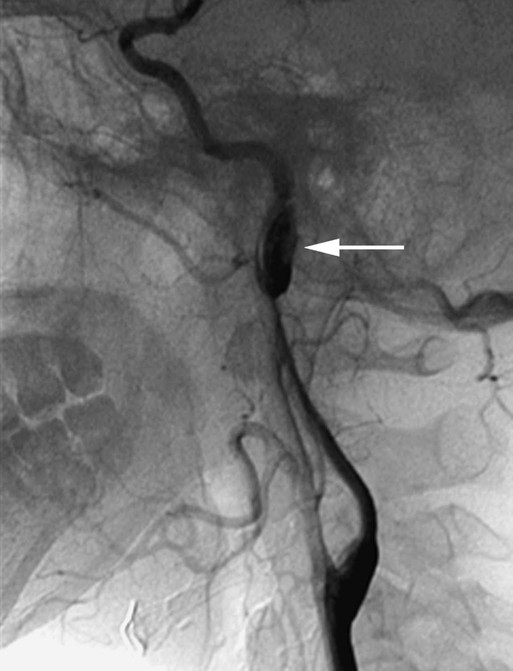
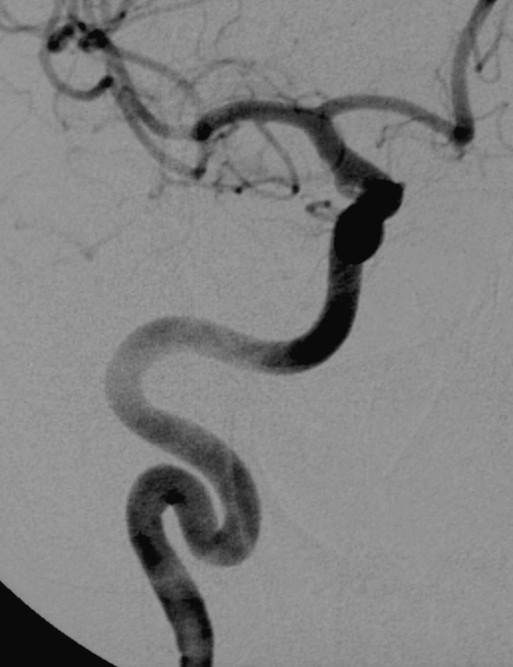
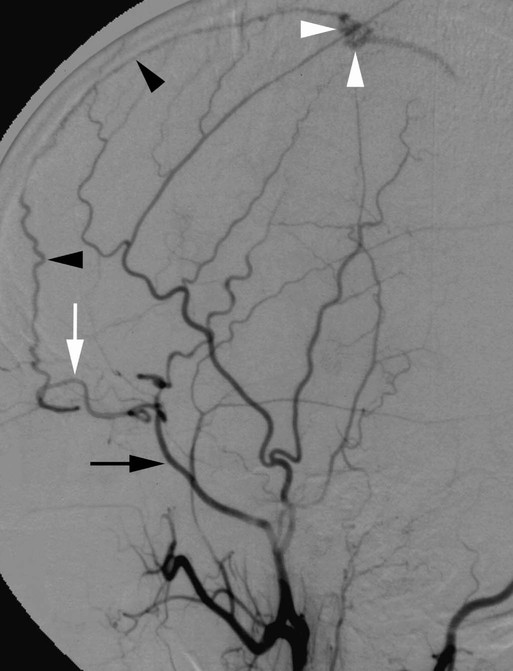
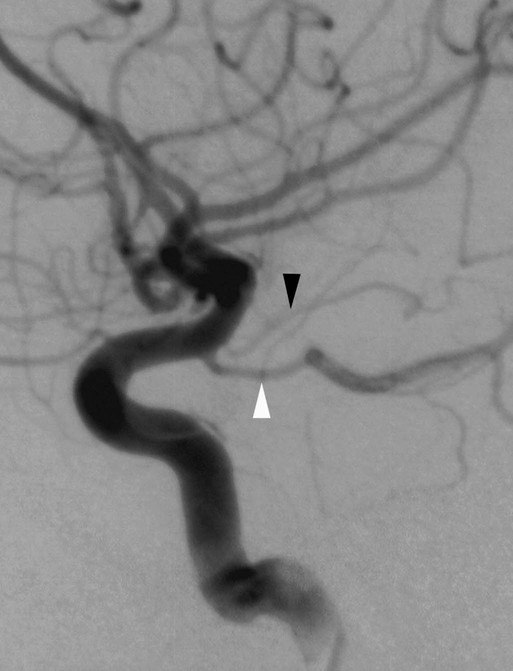
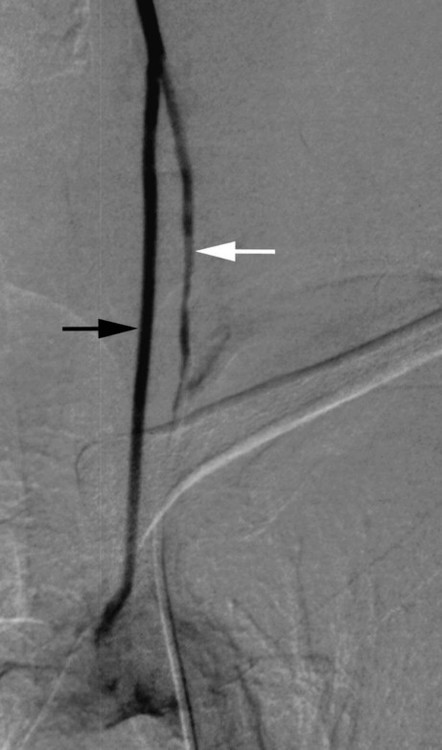
Diego San Millán Ruiz, Bradley P. Barnett and Philippe Gailloud The anatomy of the intracranial arterial system is discussed in detail in the following sections, which have been organized into the anterior and posterior circulations, the CW, and major branches of the anterior and posterior circulations (Table 87-1). TABLE 87-1 The left and right common carotid arteries (CCAs) have a different origin pattern. The right CCA generally arises from the brachiocephalic trunk (also known as the innominate artery). When the brachiocephalic trunk is absent—for instance, in the presence of an aberrant right subclavian artery (SubcA), or arteria lusoria—the right CCA comes directly from the aortic arch. Rarely, the right and left CCAs originate from a common trunk called a bicarotid trunk, a pattern usually observed in association with an aberrant right SubcA. The left CCA generally originates directly from the aortic arch, in between the brachiocephalic trunk and left SubcA. The left CCA is therefore usually longer than the right. A common origin for the left CCA and the brachiocephalic trunk is observed in approximately 13% of cases.1 This variation is commonly referred to as a “bovine arch,” a misnomer because the typical bovine arch consists of a single aortic trunk that provides all the supraaortic branches.2 In about 9% of cases, the left CCA arises from the brachiocephalic trunk itself.1 Rarely, the left CCA may share a common origin with the left SubcA and form a left brachiocephalic artery.3 Although the CCA does not normally have branches, variations may include variant origins of the superior thyroid, ascending pharyngeal, and vertebral arteries (Fig. 87-1). In rare instances, bronchial arteries can arise from the proximal portion of the CCA.4 The carotid bifurcation is most commonly located at the level of the superior border of the thyroid cartilage between the C3 and C5 vertebral levels, but extreme positions ranging from C1 to T4 may be encountered. Intrathoracic bifurcations are rare but represent a potential pitfall during angiography, when the ICA or external carotid artery (ECA) may be unintentionally catheterized because of their low origin. Intrathoracic carotid bifurcations may be more frequent in patients with Klippel-Feil anomaly.5 Both carotid bifurcations are generally found at the same level (28%) or within one vertebral level (65%).6 Immediately distal to the bifurcation, the ICA is lateral and posterior to the ECA. The ICA then bends medially to reach the outer opening of the carotid canal at the skull base, whereas the ECA ascends laterally toward the parotid gland, where it divides into its terminal branches. The ICA may infrequently arise medial (4%) or posteromedial (8%) to the ECA.7 The carotid bulb is a normal widening of the carotid bifurcation that extends from the distal CCA to the proximal ICA. It may also involve the proximal ECA. The ECA divides into numerous branches along its course between the carotid bifurcation and its termination in the maxillary and superficial temporal arteries in the parotid gland region. The classic ECA description includes eight main branches (described later) that supply the superior aspect of the thyroid gland, the viscerocranium (soft and bony structures of the face), the scalp, and a large part of the neurocranium (skull and meninges) (Fig. 87-2). Because of the existence of an extensive collateral network, selective embolization with occlusion of branches of the ECA or the ECA itself is generally well tolerated. Connections between the ECA and ICA or VA are often referred to as “dangerous anastomoses.” These anastomoses may play an important role as sources of collateral supply in patients with steno-occlusive disorders, but they also represent important pitfalls during embolization procedures within the ECA territory. These dangerous collateral pathways include (1) anastomoses between external carotid branches (mainly from the facial, maxillary, and superficial temporal arteries) and branches of the distal ICA, including the OA, inferior-lateral trunk, and meningohypophyseal trunk, and (2) anastomoses between external carotid branches (mainly the occipital artery) and muscular branches of the VA. The eight branches of the ECA are as follows: 1. The superior thyroid artery principally supplies the superior pole of the ipsilateral thyroid lobe. The superior and inferior thyroid arteries are connected through a bilateral anastomotic network that can play an important role in collateral cerebral supply.8 The superior thyroid artery also vascularizes the larynx (superior and inferior laryngeal arteries), as well as the infrahyoid and sternocleidomastoid muscles. 2. The lingual artery arises between the superior thyroid and facial arteries, although in about 20% of cases it forms a common trunk with the facial artery (linguofacial trunk). The lingual artery gives off branches for the hyoid bone, the muscles forming the floor of the mouth, the sublingual gland (sublingual branch), and the muscles of the tongue (deep lingual artery). 3. The facial artery courses over the body of the mandible toward the angle of the mouth and then ascends toward the medial epicanthus (angular artery), where it anastomoses with branches of the OA. The facial artery has numerous branches including the ascending palatine artery (for the tonsils, soft palate, and oropharynx), artery of the submandibular gland, submental artery, inferior and superior labial arteries (for the lips), lateral nasal branch, and angular artery (for the eyelids). Through its connection with the OA, the facial artery may provide collateral flow to the ICA in cases of severe stenosis or occlusion of the ICA. This pathway can be demonstrated by sonography or angiography as reversal of flow within the OA. 4. The ascending pharyngeal artery supplies the pharynx, palate, and tympanic cavity (inferior tympanic artery). Its terminal branches are meningeal arteries for the posterior fossa (clivus and posterior surface of petrous bone) that enter the cranium through the foramen lacerum, foramen jugulare, or hypoglossal canal. These branches may also participate in collateral supply of the distal ICA. 5. The posterior auricular artery ascends posteriorly between the auricular cartilage and the mastoid process. It may arise as a common trunk with the occipital artery. It gives rise to several muscular branches for surrounding muscles (digastric, stylohyoid, and sternocleidomastoid muscles), the parotid gland, and the auricle. It also provides a small stylomastoid branch that enters through the stylomastoid foramen into the facial canal and ends in the tympanic cavity. 6. The occipital artery courses over the mastoid process toward the suboccipital region and divides into terminal branches at the level of the external occipital protuberance. It provides a sternocleidomastoid branch, an auricular artery (with a meningeal branch entering the cranium through the mastoid foramen), and a descending branch to the suboccipital region. The latter branch is connected to the vertebral and deep cervical arteries and constitutes the suboccipital carrefour or “knot of Bosniak,” an important source of collateral supply in cases of steno-occlusive disease involving the VA or ICA.9 At the same time, this anastomotic network represents a significant pitfall during embolization procedures involving the occipital artery (dangerous anastomosis), and one has to be particularly vigilant for transient opacification (sometimes visible on one frame only) of a portion of the VA during selective occipital angiography. The terminal branches of the occipital artery supply the scalp of the occipital region. 7. The maxillary artery originates behind the neck of the mandible and courses through the pterygomaxillary fissure into the pterygopalatine fossa. The maxillary artery has numerous branches: • The deep auricular artery, which often arises with the anterior tympanic artery, courses through the parotid gland and pierces the cartilaginous or bony wall of the external acoustic meatus. It supplies the outer surface of the tympanic membrane and the temporomandibular joint. • The anterior tympanic artery enters the tympanic cavity through the petrotympanic fissure and supplies the tympanic membrane. • The middle meningeal artery is the largest branch of the maxillary artery. It takes a short vertical extracranial course before it enters the middle cranial fossa through the foramen spinosum. It then takes a characteristic horizontal course anteriorly and laterally toward the pterion. A posterior branch arises in the middle cranial fossa and courses along the inner surface of the temporal and parietal bones. An anterior branch reaches the pterion, where it divides into lateral and medial branches. The lateral branch courses along the inner surface of the frontal bone toward the vertex. The medial branch courses under the lesser sphenoid wing and anastomoses with a recurrent branch of the lacrimal artery (branch of the OA), usually through the meningolacrimal foramen. In some cases, a branch of the middle meningeal artery or the entire artery may arise from the OA (Fig. 87-3). Conversely, the OA may originate partially or completely from the middle meningeal artery and enter the orbit through the superior orbital fissure (see later discussion). The clinical importance of the latter variant lies in the potential risk for blindness during endovascular procedures within the ECA territory. • The accessory meningeal artery may arise from the middle meningeal artery or from the maxillary artery directly. Despite its name, its main supply is to the pterygoid and tensor veli palatini muscles, with a meningeal contribution representing only about 10% of its territory.10 The meningeal branch, which is inconstant, enters the middle cranial fossa through the foramen ovale and supplies the dura adjacent to the sella turcica and trigeminal ganglion. • The inferior alveolar artery enters the mandibular foramen and courses with the inferior alveolar nerve through the mandibular canal. One of its terminal branches, the mental branch, crosses the mental canal and anastomoses with the submental and inferior labial arteries (branches of the facial artery). • The anterior and posterior deep temporal arteries, the pterygoid branches, and the masseteric and buccal arteries supply the muscles of mastication and the buccinator muscle. • The posterior superior alveolar artery originates (like all the following branches) from the pterygopalatine segment of the maxillary artery, either directly or from a common trunk with the infraorbital artery. It supplies the mucosa of the maxillary sinus and the teeth. • The infraorbital artery enters the orbit through the inferior orbital fissure, runs forward along the roof of the maxillary sinus within the infraorbital canal (along with the infraorbital nerve), and exits the skull through the infraorbital foramen. It supplies the mucosa of the maxillary sinus, the cheek, lower eyelid, upper lip, lacrimal sac, upper incisors and canine teeth, and the side of the nose. It anastomoses with the facial artery and posterior superior alveolar artery. • The descending palatine artery courses down the pterygopalatine canal and gives off a large anterior branch, the greater palatine artery, that crosses the greater palatine foramen, runs forward along the alveolar border of the hard palate, crosses through the incisive canal, and then anastomoses with the sphenopalatine artery, thus supplying the mucosa of the palate, the palatine glands, and the gums. Lesser palatine branches from the descending palatine artery descend into the lesser palatine canals and supply the soft palate and palatine tonsils. • The sphenopalatine artery supplies the nasal mucosa after passing through the sphenopalatine foramen. The sphenopalatine artery is the targeted vessel in superselective embolization for epistaxis.11 In patients with inflammation of the nasal cavity (e.g., those with a common cold), a prominent mucosal blush with early venous drainage toward the superior ophthalmic vein and cavernous sinus may be observed and represents a diagnostic pitfall. • The artery of the pterygoid canal, or the vidian artery, extends backward along the pterygoid canal with the vidian nerve into the cartilage of the foramen lacerum. It supplies the upper part of the pharynx and auditory tube and the tympanic cavity through a small tympanic branch. • The pharyngeal artery leaves the pterygopalatine fossa through the pharyngeal canal and supplies the upper part of the nasopharynx and auditory tube. • The artery of the foramen rotundum anastomoses with branches of the inferior lateral trunk through the foramen rotundum. 8. The superficial temporal artery arises within the parotid gland, crosses the zygomatic process, where its pulsations may be felt anterior to the auricle, and then divides into terminal anterior (frontal) and posterior (parietal) branches supplying the muscles, integument, and pericranium of these regions. The transverse artery of the face arises from the superficial temporal artery in the parotid gland and crosses forward between the zygomatic arch and parotid duct to the soft tissues of the cheek. The ICA arises from the carotid bifurcation, most frequently around the C3-C5 vertebral level. The ICA is divided into cervical, petrous, cavernous, and supraclinoid (or cisternal) segments. The course of its proximal cervical segment is closely related to that of the internal jugular vein (IJV) and vagus nerve; it follows a more or less straight trajectory from its origin to the outer opening of the carotid canal. The sharp transition between the mobile distal portion of the cervical ICA and its fixed petrous segment at the skull base represents a zone at risk for traumatic injuries such as arterial dissection12 (Fig. 87-4). Marked but smooth sinuosity of the cervical ICA, which may even lead to a 180-degree turn, can be seen in individuals of any age, including young children, and constitutes an anatomic variant. This variant, classically termed coiling, more frequently involves the distal portion of the cervical ICA13 (Fig. 87-5). Coiling does not generally produce significant lumen narrowing but seems to represent a risk factor for arterial dissection.14 In contrast, the irregular tortuosity that predominates in the proximal portion of the cervical ICA develops with advancing age (generally after 50 years), arteriosclerosis, and high blood pressure. It is often termed kinking, especially when associated with arterial hypertension, in which case it acquires a classic “lead-pipe” appearance (Fig. 87-6). The cervical portion of the ICA does not normally give off angiographically detectable branches. Its average caliber is about 6 mm, and in the absence of unusual secondary branches, it remains constant throughout its course.15 Unusual branches of the cervical ICA include the ascending pharyngeal artery (8%) and less frequently the occipital artery (<0.1%). The so-called aberrant course of the ICA in which it crosses the middle ear cavity is in fact a collateral pathway established between the ICA and ECA branches in the case of cervical ICA agenesis.16 The branches involved are the inferior tympanic branch of the ascending pharyngeal artery and the caroticotympanic branch of the ICA. An aberrant ICA is a potential hazard during middle ear surgery. Constitutional ICA hypoplasia or agenesis may be differentiated from acquired lesions (e.g., atheromatous occlusion, dissection, and even congenital thrombosis) by looking at the caliber of the carotid canal on a CT scan. An absent or narrowed carotid canal suggests the constitutional nature of the ICA agenesis or hypoplasia. Acquired or congenital absence of an ICA is associated with a higher incidence of cerebral aneurysms, probably because of increased collateral flow through vessels such as the anterior communicating artery (AComA).17 The cavernous segment provides numerous branches usually described as “trunks,” although they often arise separate from the ICA. The meningohypophyseal trunk originates from the superior and posterior aspect of the ICA at the junction between the C5 and C4 cavernous segments (ascending and horizontal segments) (Fig. 87-7). Its branches include (1) the inferior hypophyseal artery, which is responsible for the angiographic blush of the posterior lobe (neurohypophysis) (Fig. 87-8); (2) the medial clival artery, also known as the dorsal meningeal branch of the ICA, which anastomoses with clival branches of the ascending pharyngeal artery; (3) the marginal tentorial artery (called the artery of Bernasconi and Cassinari when it vascularizes a tentorial meningioma), which courses along the free margin of the tentorium cerebelli; and (4) the basal tentorial artery, which runs laterally along the petrous edge. The inferolateral trunk (or inferior cavernous artery of Parkinson) comes off the lateral and inferior aspect of the ICA (see Fig. 87-8). Its branches include (1) the artery of the foramen rotundum (anastomosis with the anterior deep temporal artery), (2) the artery of the foramen ovale (anastomosis with the accessory middle meningeal artery), (3) the artery of the foramen lacerum (anastomosis with the carotid branch of the ascending pharyngeal artery), (4) the lateral clival artery, and (5) anastomotic branches to the OA (deep recurrent OA) and middle meningeal artery. The inferior capsular and anterior capsular arteries of McConnell arise from the C5 and C4 segments of the cavernous ICA, respectively.18 The capsular arteries do not contribute significantly to vascularization of the gland itself but send branches to the floor of the sella turcica. They are not usually angiographically detectable. The supraclinoid or cisternal portion of the ICA (C2 and C1 segments) courses cranially until it bifurcates into the ACA and MCA within the carotid cistern. Immediately after crossing the dural ring, the ICA provides several superior hypophyseal arteries that vascularize the posterior end of the optic nerves, optic chiasm, pituitary stalk, and anterior lobe of the hypophysis.18 Three important arteries branch off the supraclinoid ICA: the OA, the PComA, and the AChoA. The posterior communicating artery (PComA) is discussed in the CW section. The OA is divided into intracranial, intracanalicular (within the optic canal), and intraorbital segments. Its origin is located on the intradural portion of the ICA in 89% of cases, but it may also be extradural on the cavernous portion or within the dural wall of the cavernous sinus itself.13 The OA presents numerous anastomoses with branches of the facial, maxillary, and superficial temporal arteries. A particularly interesting connection is established between the recurrent meningeal branch of the lacrimal artery and the orbital branch of the middle meningeal artery. This anastomosis corresponds to a remnant of the primitive orbital artery and allows an explanation for two clinically significant anatomic OA variants: the OA providing the middle meningeal artery and a complete or partial middle meningeal origin of the OA (Fig. 87-9). Exceptional variants of the OA include origin from the ACA (persistent ventral OA)19,20 and from the BA.21 The OA has numerous branches, as summarized in Table 87-2. TABLE 87-2 The AChoA is a small (0.5-1.5 mm) but functionally important artery that originates from the posterior surface of the ICA in the vast majority of cases, 2 to 4 mm distal to the origin of the PComA (Fig. 87-10). The AChoA usually arises as a single trunk but may be duplicated or triplicated. It courses through the carotid, crural, and ambient cisterns (cisternal segment), enters the choroidal fissure, and terminates within the choroidal plexus of the temporal horn (plexal segment), which it supplies in conjunction with the posterior lateral choroidal artery. There is a reciprocal relationship between the territories vascularized by the AChoA, PComA, PCA, and MCA. The AChoA supplies the uncus, anterior hippocampal and dentate gyri, posterior medial amygdala, and tail of the caudate nucleus through its uncal branch. Branches from the cisternal segment of the AChoA supply the inferior aspect of the optic chiasm and posterior two thirds of the optic tract, part of the globus pallidus, the cerebral peduncles, genu of the internal capsule, substantia nigra, red nucleus, and the ventral anterior and ventral lateral thalamus. The plexal segment supplies the choroid plexus of the temporal horn, part of the lateral geniculate body, the posterior limb and retrolenticular portion of the internal capsule, and the optic radiations. The VA generally originates from the posterior superior aspect of the first segment of the SubcA as the first branch of the SubcA. The VAs are frequently asymmetric, the left VA being dominant in 60% of cases and the right one in 20%. Possible variations in the origin of the VA include direct origin from the aortic arch (most frequently on the left side), from a common trunk with other subclavian branches (e.g., thyrocervical trunk), or from the CCA. The latter case occurs most frequently on the right and is usually associated with an ipsilateral aberrant SubcA (arteria lusoria). Dual origin of the VA can occur, generally from the SubcA and aortic arch on the left side or from the SubcA and innominate artery on the right side (Fig. 87-11). These dual origins may mimic VA dissection.22
Craniocervical Vascular Anatomy
Craniocervical Arteries
Acronym
Expanded
ACA
Anterior cerebral artery
AChoA
Anterior choroidal artery
AComA
Anterior communicating artery
AG
Arachnoid granulation
AICA
Anterior inferior cerebellar artery
BA
Basilar artery
BVR
Basal vein of Rosenthal
CCA
Common carotid artery
CS
Cavernous sinus
CW
Circle of Willis
ECA
External carotid artery
ICA
Internal carotid artery
ICV
Internal cerebral vein
IJV
Internal jugular vein
IVVP
Internal vertebral venous plexus
MCA
Middle cerebral artery
OA
Ophthalmic artery
PCA
Posterior cerebral artery
PComA
Posterior communicating artery
PICA
Posterior inferior cerebellar artery
PTA
Persistent trigeminal artery
SubcA
Subclavian artery
SCA
Superior cerebellar artery
SMCV
Superficial middle cerebral vein
SSS
Superior sagittal sinus
VA
Vertebral artery
VAVP
Vertebral artery venous plexus
VG
Vein of Galen
WS
Vertebral venous system
Anterior Circulation
Common Carotid Artery
Carotid Bifurcation
External Carotid Artery
Internal Carotid Artery
Intracranial Segments of Internal Carotid Artery
Group
Branches
Ocular
Central retinal artery
Ciliary arteries
Collateral branches for optic nerve (cranial nerve II)
Orbital
Lacrimal artery
Muscular arteries
Arteries for periosteum and areolar tissue
Extraorbital
Posterior/anterior ethmoidal arteries
Supraorbital/supratrochlear arteries
Medial palpebral, dorsal nasal arteries
Vertebrobasilar System
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Craniocervical Vascular Anatomy