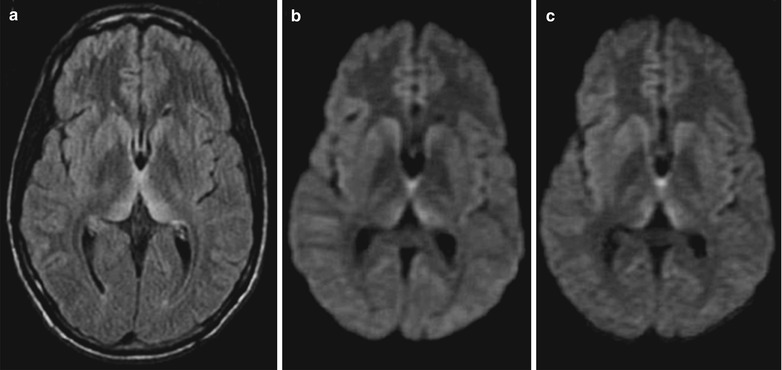
Fig. 11.1
CJD. (a–i) MRI T2WI, FLAIR, and DWI demonstrate abnormally increased high signal in the cerebral hemisphere cortex and bilateral caudate nucleus. (j–l) Basal ganglia multi-voxel medium echo MRS demonstrates decreased NAA, no abnormalities of Cr and Cho as well as no other abnormal metabolic peaks (Lac, Lip, Glx, AA) in the head of right caudate nucleus and anterior putamen
Case Study 2
A female patient aged 74 years complained of inaccuracy of right-hand gripping but strong holding since March 8. About 1 week later, her family member found that she had involuntary movements of her right hand and often gripped the upper corner of her clothes in a posture of right upper limb flexion. The involuntary movements could be reduced after she was urged to relax. Since March 25, she had slow speaking, difficulty saying long sentences, and short footstep paces, with complains of feeling downward sloping and thus difficulty walking. Meanwhile, her involuntary movements of her right upper limb further aggravated, with a twist posture of anterior rotation and dorsiflexion during attacks. Sometimes her head and neck leaned rightward with increased tension, with attacks during sleeps. Her family complained for her of irritation during attacks and muscular tension, which could be relieved after she was urged to relax. Since the onset, her conditions had continuously progressed. She had been diagnosed in a local hospital with cerebral infarction and had received therapies for improving blood circulation and nourishing nerves. Since April 5, she had been hospitalized in another hospital. Meanwhile, the patient experienced cognitive decline, slow response, decreased comprehension, and irritation. Her family member complained for her of paroxysmal myoclonus of the both upper limbs, which was common during sleeps. During her hospitalization, she also experienced difficulty urination, and she had to try hard for urination. Head CT scanning demonstrated calcification of bilateral basal ganglia, and head MRI demonstrated strips of high signal in the left occipital and parietal cortex. Experts at Department of Neurology in Huashan Hospital were invited for a consultation, with a suspected diagnosis of Parkinson’s disease. Since April 6, she had been given Madopar, but with no significant efficacy. The patient experienced further aggravated involuntary twist and stiffness of her limbs, with further cognitive decline and inability to live independently. On April 14, she began to experience difficulty walking and inability of independent walking. On April 15, she was admitted in our hospital. By physical examination, T is 37 °C, P 80 per minute, R 20 per minute, and BP 150/80 mmHg. She had good consciousness, slight nervousness, keeping answers appropriate to the point, clear and slightly low speaking, and poor orientation, calculation, and comprehension. The diameter of her double pupils was 3.0 mm, with light relex positive, movement of both pupils good, and K-F ring positive. Her right upper limb had increased muscular tension, with proximal muscle strength of both upper limbs 5− and grip strength of both hands 5, bilateral biceps reflex (++), triceps reflex (++), patellar tendon reflex positive, muscle strength of the left lower limb 5−, and muscle strength of the right lower limb 5−. In addition, the Romberg sign positive and inability waking in straight line. By CSF examination, cerebrospinal fluid is light yellow and clear, with red blood cells positive by microscopy and nucleated cell count 2 × 106/L; Pandy test negative; protein 221 mg/L, glucose 3.43 mmol/L, chloride 130 mmol/L, and bacterial culture of cerebrospinal fluid negative. By EEG, highly abnormal demonstrations were found, with frequent slow waves with sharp waves, sharp-slow waves, and triphasic waves, which were obvious in the right temporal lobe. The clinical diagnosis was CJD.
Fig. 11.2
CJD encephalopathy and brain atrophy. (a–d) MRI demonstrates abnormally increased signal in the cerebral cortex, widened and deepened sulci (Note: Case 1 and 2 as well as corresponding figures are provided by Tang YH at Ruijin Hospital, Shanghai, China.)
Case Study 3
A female patient aged 72 years had left hemiplegia.
Case Study 4
A female patient aged 57 years was after dura mater transplantation, 7 weeks after the onset of progressive dementia and right hemiplegia.
Case Study 5
A female patient aged 59 years was admitted to our hospital due to progressive dementia, speaking influency and walking instability for 4 months. She began to experience memory loss, declined attention, and accompanied walking instability 4 months ago. She sustained obvious cognitive impairment with inability to recognize her family members as well as accompanying dysphasia, limb stiffness, and incontinence 3 months ago. By physical examination, consciousness is good, indifferent, poor calculation and memory, impaired articulation, and difficulty in language use. Her pupils are equal in size, equally round with a diameter of about 3.0 mm, sensitive to light. She had no mouth corner deflexion, tongue sticking in the middle, and no abnormalities in limb muscle strength, muscle tension, and tendon reflex. By finger-nose test and heel-knee-tibia test, a little bit unsteady and inaccurate. Meningeal irritation sign negative. By CSF examination, 14-3-3 protein positive. By PRNP gene sequence analysis, (1) E200K mutation; (2) M/M type in polymorphism of the 129 amino acids. By dynamic EEG, triphasic spike and slow wave complex. The clinical diagnosis was gCJD. Death occurred 2 months after the diagnosis was defined.
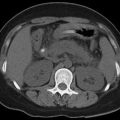
Fig. 11.3
gCJD. (a) Plain CT scanning demonstrates symmetric slight low density lesions in the head of bilateral caudate nucleus and putamen, with poorly defined boundaries. (b, c) MRI demonstrates symmetrical slight long T1 long T2 signals in the bilateral caudate nucleus and putamen, with well-defined boundaries. (d, e) FLAIR and DWI demonstrate symmetric high signal of the above lesions. (f) Contrast MR imaging demonstrates no enhancement of the above lesions (Note: The case and figures were provided by Chen LH and Lu Y at First Affiliated Hospital of Nanyang Medical College, Nanyang, Henan, China.)
Case Study 6
A patient aged 18 years.