Algorithm 18.1 Basic surgical and radiological anatomy of the abdominal wall
Abdominal wall architecture and structure include the skin, superficial fascia, subcutaneous fat tissues, and muscular layers. The deepest aspect is limited by extraperitoneal fat [1].
The muscle groups can be divided according to the region of interest in anterior and posterolateral groups. The anterior group consists of the rectus abdominis muscle, the external and internal oblique muscles, and the transversus abdominis muscle [2].
The posterolateral abdominal wall includes the following: latissimus dorsi, quadratus lumborum, erector spinae (sacrospinalis), and other paraspinal muscles [3].
In general, all muscle groups are separated from the peritoneum by the transversalis fascia and by extraperitoneal fat [4].
Also, surgically, the inferior and lateral aspects of the anterior abdominal wall include two adjacent but anatomically distinct areas: the inguinal canal and the femoral triangle [3].
Inferiorly, the pelvic floor limits the pelvis.
Anterior Abdominal Wall
The anterior abdominal wall is composed of multiple muscles and their associated aponeuroses, fasciae, fat, and skin [3]. Laterally, three muscle layers are identified, which run obliquely to each other [4].
The paired rectus abdominis muscles originate on the pubis inferiorly and insert on the ribs superiorly [3]. At the lateral margin of the rectus abdominis muscles is the linea semilunaris, where the aponeurosis serves as an insertion for the lateral musculature. The semicircular line is defined as a posterior sheath located between the umbilicus and the pubis and has a concavity oriented toward the pubis [1, 3, 4].
Above this line, the internal oblique aponeurosis divides into a posterior lamina and a anterior lamina. The posterior lamina joins the transversus abdominis aponeurosis and forms the posterior rectus sheath [1]. The anterior rectus sheath results from the fusion of the anterior lamina and the external oblique aponeurosis. The external oblique aponeurosis forms the external lamina of the anterior sheath, below the semicircular line. Fusion of the internal oblique and transversus abdominis aponeuroses forms the internal lamina of the anterior sheath [1, 3, 4].
The posterior surface of the rectus muscles is covered by the transversalis fascia, below the semicircular line. The midline linea alba represents a decussation of these fibers [3, 5].
The external oblique muscle originates on the lower eight ribs and runs obliquely, from superior to inferior, and inserts inferiorly into the rectus sheath [6].
Deep to the external oblique muscle is the internal oblique muscle with fascicles that are oriented obliquely to the external oblique, arising from the iliac fascia (deep to the lateral half of the inguinal ligament, in the anterior two-thirds of the iliac crest), and in the lumbodorsal fascia. It inserts into the rectus sheath, and in the lower ribs and cartilages superiorly [6].
The transversus abdominis muscle is the most internal muscle of the anterolateral abdominal wall musculature and its orientation is transverse. It arises from the lateral iliopubic tract, the iliac crest, the lumbodorsal fascia, and the lower six ribs. It fuses with the internal oblique aponeurosis to become the posterior rectus sheath [7]. The inferior aspect of this muscle forms the transversus abdominis aponeurotic arch as the upper edge of the inguinal ring and above the medial floor of the inguinal canal [8].
The innominate fascia overlies the external oblique muscle. The transversalis fascia forms the envelope of the abdominal cavity [9].
Posterolateral Abdominal Wall Region
The quadratus muscle originates in the iliac crest and the iliolumbar ligament, between the iliac crest and the fifth lumbar transverse process. It then inserts along the 12th rib [10].
The psoas muscle arises from vertebrae T12 through L5 and passes downward under the inguinal ligament to insert on the lesser trochanter [7, 8, 11].
The posteroinferior serratus muscle originates from the lumbodorsal fascia and inserts along the four lower ribs [10].
The sacrospinalis muscle runs along the spinous processes for the entire length of the spine [11].
The latissimus dorsi muscle originates on the posterior third of the iliac crest, the spinous processes of the sacral and lumbar vertebrae and the lumbodorsal fascia, inserting in the intertubercular groove of the humerus [11].
The superior lumbar triangle of Grynfeltt-Lesshaft is bounded superiorly by the 12th rib, the posterior lumbocostal ligament, and the posteroinferior serratus muscle; inferiorly by the superior border of the internal oblique muscle; and posteriorly by the lateral border of the sacrospinalis muscle. The deep margin of the superior lumbar triangle is the transversus abdominis muscle, and the superficial margin is the latissimus dorsi muscle [7, 8, 11].
Inguinal Canal
The inguinal canal is a major complex structure arising out of the abdomen, through the anterolateral musculature, and is simply the medial half of the thickened lower free edge of the external oblique aponeurosis, which curls back on itself and forms a gutter. The canal contains the spermatic cord in males and the round ligament in females [9, 12].
These structures pass through the deep inguinal ring, which is an opening in the transversalis fascia, lateral to the inferior epigastric artery emerging through the external oblique aponeurosis at the superficial inguinal ring [7–9].
Each fascial layer from the lateral musculature of the abdominal wall provides a laminar covering for the spermatic cord, from the outermost to innermost: (a) external spermatic fascia (derived from external oblique aponeuroses), (b) cremaster muscle and fascia (derived from internal oblique and transverse muscles), and (c) internal spermatic fascia (derived from transverse fascia).
Femoral Triangle
The major feature of the femoral triangle is the femoral sheath. The sheath is the condensation of the deep fascia (fascia lata) of the thigh and contains, from lateral to medial, the femoral artery, femoral vein, and femoral canal. The femoral canal is a space medial to the vein that allows for venous expansion and contains a lymph node (node of Cloquet). Other features of the femoral triangle include the femoral nerve (lateral) and the great saphenous vein [7–9].
The boundaries of femoral triangle are the inguinal ligament (superior), medial border of the long adductor muscle (medial), the medial border of the sartorius muscle (lateral), and the iliopsoas, pectineal, and long adductor muscles (floor) [7, 8, 14].
Key Points (Anatomy)
(a)
Muscles of the abdominal wall can be divided into anterior and posterolateral.
(b)
Clinicians usually divide the inguinal region in two different anatomical areas: the inguinal canal and the femoral triangle.
(c)
The internal oblique aponeurosis divides into a posterior and an anterior lamina. The posterior lamina joins the transversus abdominis aponeurosis and forms the posterior rectus sheath. The anterior rectus sheath results from fusion of the anterior lamina and the external oblique aponeurosis. The external oblique aponeurosis forms the external lamina of the anterior sheath below the semicircular line.
(d)
The posterior rectus sheath ends at the arcuate line approximately 2 cm below the umbilicus.
Imaging Techniques and Protocols
Multidetector CT (MDCT) and MRI are considered the best imaging modalities for evaluation of abdominal wall pathology (Table 18.1). Although associated with ionizing radiation, MDCT is considered accurate, less expensive, and widely available and currently is the modality of choice for noninvasive assessment of abdominal wall pathology. Ultrasound, in selected cases, can be used as the primary imaging tool due to its low cost and greater availability.
Table 18.1
Classification of abdominal wall pathology
Hernias | Complications of hernias | Neoplastic pathology | Non-neoplastic pathology |
|---|---|---|---|
Congenital or acquired | |||
Inguinal hernias | Benign | Abdominal wall abscess | |
Direct, indirect, and femoral | Bowel obstruction | Fibromatosis | Hematoma |
Ventral hernias | Incarceration | Lipomas | Endometrioma |
Umbilical and paraumbilical | Strangulation | Neurofibromas | Varicose veins |
Epigastric and hypogastric | Trauma | Hemangiomas | |
Lateral/spigelian | Lymphangiomas | ||
Incisional and parastomal hernias | Postsurgical complications | Malignant | |
Lumbar hernias | Hernia recurrence | Primary | |
Superior or inferior | Fluid collections | Soft tissue sarcomas | |
Infection | Secondary | ||
Miscellaneous hernias | Mesh-related complications | Metastases | |
Obturator, sciatic hernias | Direct spread | ||
Narath’s, Richter’s, Littre’s, Amyand’s, Laugier’s hernias |
Radiography
Uncomplicated small abdominal wall hernias have no major representation on conventional radiographs. In some cases, including those with large wall defects or large hernia sacs, wall hernias may be visible. In these cases, air-, fluid-, or stool-filled loops are seen in abnormal locations in the abdomen, most frequently in the inguinal or in the umbilical area [15, 16].
MDCT
Computed tomography clearly demonstrates the anatomical site of the hernia sac, the content, and any bowel complications due to incarceration or strangulation [2, 7, 16–20]. It can distinguish hernias from masses of the abdominal wall, such as tumors, hematomas, abscesses, undescended testes, and aneurysms, and can provide information about the presence of complications such as incarceration, bowel obstruction, volvulus, and strangulation [6].
Because of the widespread availability of MDCT, its shorter acquisition times, greater coverage, and superior image resolution, it is considered pivotal to assess patients with suspected wall hernias [8]. Moreover, three-dimensional information and multiplanar reformat images provide excellent anatomical depiction of the abdominal wall anatomy, as well as useful information for surgical planning. CT is considered the imaging modality of choice for evaluation of postsurgical patients [7].
Key Points (MDCT Technical Aspects)
(a)
Because most of pathological conditions of the abdominal wall are incidental findings, supine axial imaging is typical. Thin reconstructions (1 mm) improve diagnostic capabilities of MDCT.
(b)
Postural maneuvers are recommended (e.g., prone or lateral decubitus patient positioning) and maneuvers to increase intra-abdominal pressure (e.g., straining, Valsalva maneuver) can help outline small hernias.
(c)
Intravenous administration of contrast is recommended to assess vascular supply and possible complications (strangulation, incarceration). Positive oral contrast is not mandatory and water may be used.
(d)
Recommended values are as follows: IV contrast 75 cc at an injection rate between 2 and 4 cc/s. Imaging acquisition at 40–70 s. Table speed is 10 mm/s. Collimation 2.5 mm. Thin (1–3-mm) reformatted images routinely obtained.
MR
Factors such as need of patient’s cooperation to reduce artifacts, reduced availability, inherent high cost, and long acquisition time, as well as more consolidated and widespread knowledge and experience on CT than MRI, limit the role of this technique in evaluating patients with suspected abdominal wall hernias [4, 21–23].
Ultrasound
Although ultrasound is highly operator dependent, it is a relatively inexpensive, noninvasive, and widely available imaging tool [24]. Abdominal wall evaluation using ultrasound requires high-frequency linear probes and, when necessary, flotation pads, to achieve best resolution and avoid the “bang effect” of direct transducer placement on the skin [25]. Ultrasound allows dynamic evaluation (e.g., during Valsalva maneuvers), to confirm herniation of intra-abdominal content through the wall defect [7, 25].
Abdominal Wall Hernias
Abdominal wall hernias include inguinal, femoral, obturator, umbilical, spigelian, epigastric, lumbar, ventral, incisional, and miscellaneous hernias (Fig. 18.1). All abdominal hernias consist of a peritoneal sac that protrudes through a weakness or defect in the muscular layers of the abdomen. The defect may be congenital or acquired [26–28].
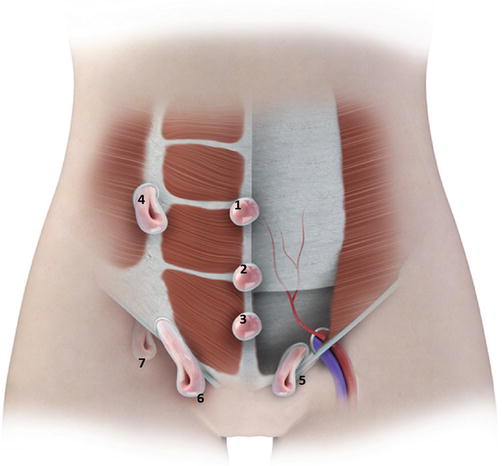
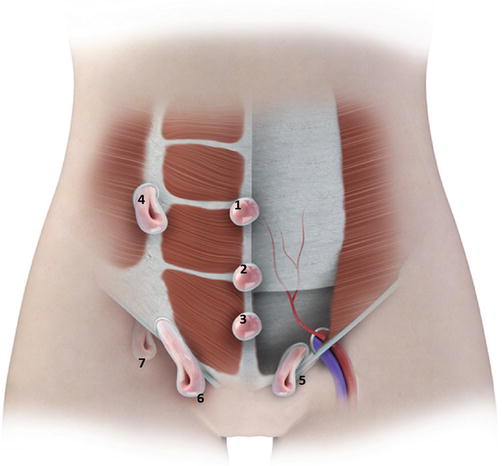
Fig. 18.1
Diagram demonstrating a panoramic view of the anterior abdominal wall, depicting the different types of abdominal wall hernias. 1 supraumbilical hernia. 2 umbilical hernias. 3 infraumbilical hernia. 4 spigelian hernia. 5 femoral hernia. 6 indirect inguinal hernia. 7 direct inguinal hernia
Prevalence and Definitions
Abdominal wall hernias are a common clinical problem especially in elderly patients because of the weakness of the abdominal wall and conditions that increase intra-abdominal pressure. The estimated incidence of abdominal wall hernias in persons older than 65 years of age is 13 per 1,000 [29].
Moreover, abdominal wall hernias represent a frequent imaging finding in the abdomen, and thus, their actual prevalence and distribution are not accurately reflected in the literature [7].
Algorithm 18.2 Distribution of abdominal wall hernias
Algorithm 18.3 Main abdominal wall hernias and key diagnostic findings
Inguinal Hernias
Inguinal hernias represent the most common type of abdominal wall hernias and include direct, indirect, and femoral. Inguinal hernias are located above the inguinal ligament and can be differentiated in contrast studies by their location medial to the epigastric artery (direct) or lateral to these vessels (indirect) [30]. Femoral hernias are below the inguinal ligament. Approximately 80 % of abdominal wall hernias are inguinal and only 5 % are femoral [19].
Indirect Inguinal Hernias
In children, indirect inguinal hernias are related with the persistence of the peritoneal-vaginal process, which is a continuation of the peritoneum in the inguinal canal (Fig. 18.2), formed when the testicle descends from intraperitoneal to intrascrotal location and is obliterated shortly after birth [31]. This process allows the passage of the hernia sac into the external inguinal ring, through the inguinal canal (Fig. 18.3). In men, the sac may extend into the scrotum by the spermatic cord, and in women follows the course of the round ligament. In adults, indirect inguinal hernias occur more frequently due to weakness and dilatation of the internal inguinal ring [32].
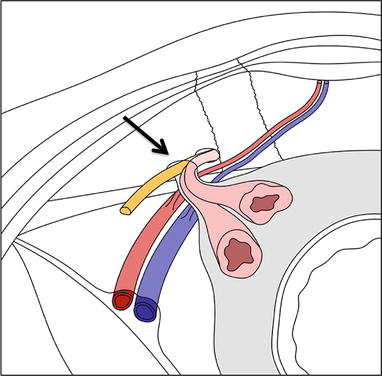
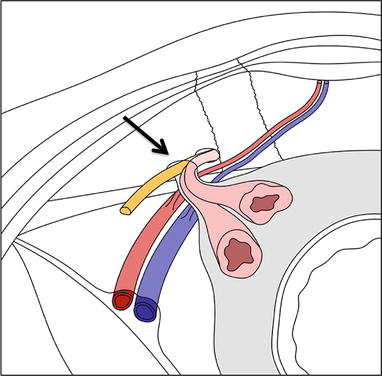
Fig. 18.2
Indirect inguinal hernia. Diagram demonstrating inner vision of the anterior abdominal wall depicting an indirect inguinal hernia. The hernia sac protrudes through the internal inguinal ring (arrow), located lateral to the epigastric vessels
Fig. 18.3
Axial MR T2W image (a) and coronal reformat MDCT image (b) demonstrating indirect inguinal hernias (arrows)
Direct Inguinal Hernias
Direct inguinal hernias occur more frequent in adult men and often are bilateral [32]. They often protrude through potential weakness sites such as the triangle of Hesselbach, which is located in the posterior wall of inguinal canal and is formed laterally by the inferior epigastric artery, inferiorly by the inguinal ligament, and medially by the margin of the anterior rectus sheath (Fig. 18.4) [33]. They are characterized by a wider neck and are less prone to incarceration when compared to indirect and femoral hernias (Fig. 18.5) [7].
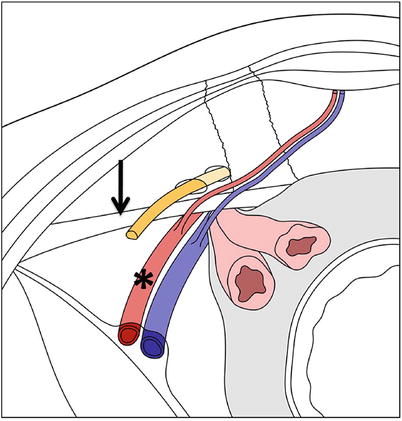
Fig. 18.4
Direct inguinal hernia. Diagram demonstrating inner vision of the anterior abdominal wall depicting a direct inguinal hernia. The hernia sac protrudes through the Hesselbach’s triangle, limited by the inferior epigastric vessels, lateral wall of the rectus abdominis muscle (asterisk), and the inguinal ligament (arrow)
Fig. 18.5
Contrast-enhanced (oral and IV) MDCT axial (a) and coronal (b) images demonstrating direct inguinal hernia with bowel content (arrows). MDCT coronal (c, d) images in different patients demonstrating direct inguinal hernias with fluid-filled peritoneal content (arrows). On image C, there is fat stranding, finding that may indicate incarceration
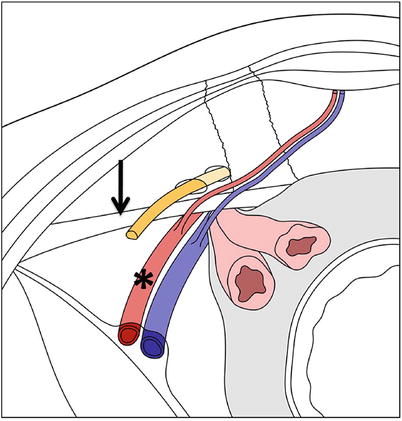
Fig. 18.6
Femoral hernia. Diagram demonstrating inner vision of the anterior abdominal wall depicting a femoral hernia. The hernia sac protrudes through the femoral canal medial to the femoral vessels (asterisk) and inferior to the inguinal ligament (straight arrow)
Femoral Hernias
Femoral hernias occur more commonly in women [34], usually on the right side, and are less common than inguinal hernias. They arise from a defect in the transversalis fascia insertion at the pubis, which protrudes through the femoral ring and canal, usually medial to the femoral vein and the posteroinferior inguinal ligament (Figs. 18.6 and 18.7) [35]. Intestinal strangulation is common, due to the narrowness and rigidity of the femoral canal [36].
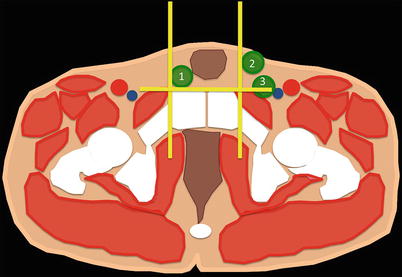
Fig. 18.7
MDCT axial (a) and coronal (b) images demonstrate fat-containing femoral hernia sac (arrows)
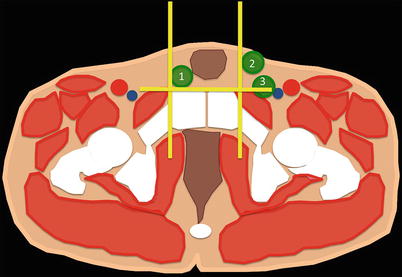
Fig. 18.8
Scheme representing a axial CT image at the level of the pubic tubercle. The pubic tubercle is easily seen on CT and corresponds to the anteroinferior insertion of the inguinal ligament. Orthogonal planes are delineated tracing a line perpendicular to the pubic tubercle (anterior-posterior line, yellow) and parallel to this structure (transverse line, yellow). Inguinal hernias are situated above the ligament and should be located entirely anterior (direct inguinal hernia-2) or partially anterior to (indirect inguinal hernia-1) the transverse line. Femoral hernias (3) are situated below the ligament and can only be located posterior to the drawn transverse line. These hernias are always located lateral to the anterior-posterior orthogonal line
The Pubic Tubercle Method in Differentiating Inguinal Hernias by Cross-sectional Imaging Techniques
From the surgical perspective, it is important to differentiate between inguinal and femoral hernias, since management changes. For this reason, some authors have suggested that such differentiation can be done by cross-sectional imaging, based on the relationship of the hernia sac with the pubic tubercle, as is the medial insertion site of the inguinal ligament [37]. Two recent studies corroborate this hypothesis [35] stating that inguinal hernias, anatomically located above the ligament, must be located entirely above (direct inguinal hernia) or partially above (indirect inguinal hernia) to the orthogonal lines drawn through the pubic tubercle on axial images. If the sac is located lateral to the tuber and if there is venous compression, the findings suggests a femoral hernia (Fig. 18.8).
Ventral Hernias
Ventral hernias include all hernias of the anterior and lateral abdomen (other than inguinal).
Anterior Wall Defects
Umbilical and Paraumbilical Hernias
Umbilical hernias and paraumbilical hernias are usually congenital and can result from lack of closure of the physiological abdominal defect [20], which occurs at the tenth week of gestation when abdominal contents return to the abdominal cavity. Additional cause includes the incomplete closure of the ring after umbilical cord clamping. The closure of the umbilicus involves the production of circumferential granulation tissue, which results in fusion of the skin and formation of a single layer of fascia and peritoneum. When the merge is incomplete, there is a weak spot in this region through which these hernias protrude [1]. Many umbilical hernias are identified at birth, but continuous formation of granulation tissue leads to its complete closure by age four. These kinds of hernias are usually small and rarely present with incarceration (Fig. 18.9). Acquired anterior hernias typically present in adults with a history of obesity, multiparity, or increased intra-abdominal pressure and are more prone to strangulation [1]. Paraumbilical hernias are protrusions through the linea alba in the region of the umbilicus and are associated with diastases of the rectus abdominis muscles (Fig. 18.10).
Fig. 18.9
Axial (a) and sagittal (b) MDCT reformat images demonstrating bowel-containing (a) and fat-containing (b) umbilical hernias (arrows)
Fig. 18.10
Axial (a) and sagittal (b) MDCT reformat images demonstrating paraumbilical hernia partially containing bowel (a) and fat-containing sac (arrows). Axial T2W MR image (c) demonstrating paraumbilical hernia containing bowel (arrows)
Epigastric and Hypogastric Hernias
Usually associated to defect in the fascia that forms the linea alba [20], the epigastric hernia is located between the umbilicus and xiphoid process and the hypogastric hernias are located below the umbilicus. Strangulation and incarceration are common in all hernias of the midline (Fig. 18.11).


Fig. 18.11
Sagittal MDCT reformat image demonstrating epigastric hernia with fat-containing sac (arrow)
Lateral Wall Defects
Spiegel hernias protrude through a defect in the fibrous union between the rectus muscle and the fascia of transverse and oblique muscles, known as the semilunar line which extends from the ninth costal cartilage to the symphysis pubis (Fig. 18.12) [38]. These hernias are associated with a high risk of strangulation and incarceration (Fig. 18.13) and must be distinguished from intraparietal hernias, in which the hernia sac is located between the different muscle layers (Fig. 18.14) [39, 40].
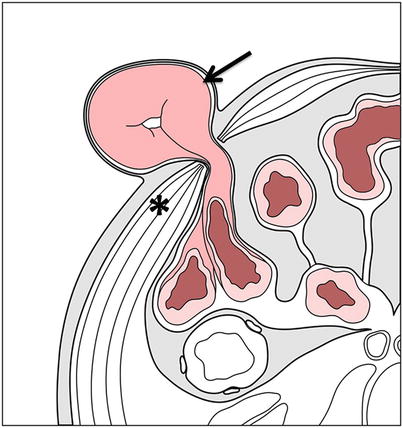
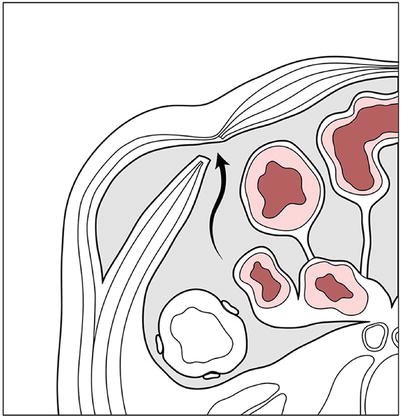
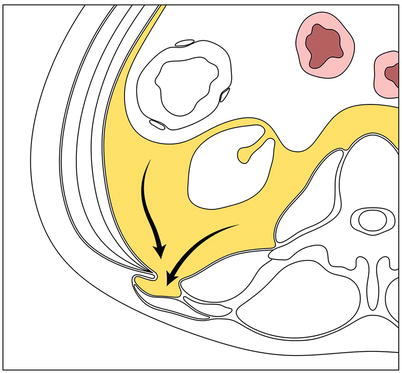
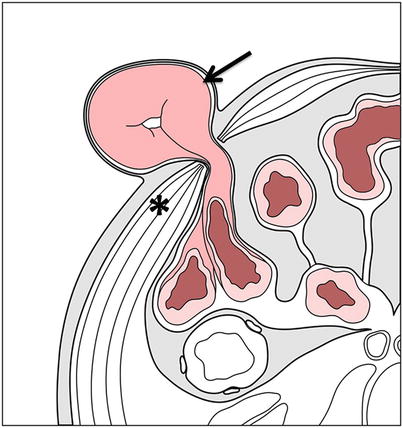
Fig. 18.12
Complete spigelian hernia. Diagrammatic axial view of the abdomen through the level of the umbilicus depicting a complete spigelian hernia (arrow). As in incomplete hernias, the hernia sac protrudes through the linea semilunaris. However, in complete hernias, the hernia sac protrudes through the complete thickness of the wall musculature (asterisk)
Fig. 18.13
Axial (a) and coronal (b) MDCT reformat images demonstrating bilateral spigelian hernias with fat-containing sacs (arrows)
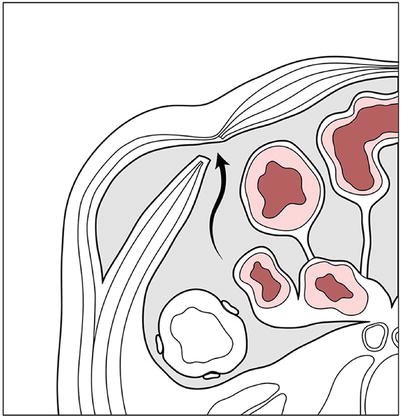
Fig. 18.14
Interparietal spigelian hernia. Diagrammatic axial view of the abdomen through the level of the umbilicus depicting an interparietal spigelian hernia. Note the hernia sac (curved arrow) protruding through the linea semilunaris without exiting into the subcutaneous tissue, herniating between the internal and external oblique muscles
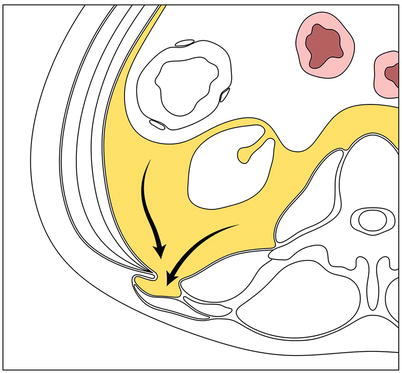
Fig. 18.15
Superior lumbar hernia. Diagrammatic axial view of the abdomen through the superior lumbar triangle. Note the hernia sac (curved arrows) containing retroperitoneal fat herniating through the superior lumbar triangle, bordered by the internal oblique muscle anteriorly, the 12th rib superiorly, and the erector spinal muscle posteriorly
Lumbar Hernias
Lumbar hernias may arise spontaneously or secondary to surgery or trauma. They occur in the superior lumbar triangle (Grynfeltt-Lesshaft) (Fig. 18.15) or less frequently in the lower lumbar triangle (Petit) [41]. Although these hernias may contain bowel, omentum, kidneys, spleen, or the stomach, strangulation is rare given that most of the times, these hernias have a wide neck (Fig. 18.16) [8, 42].
Fig. 18.16
Axial (a) and coronal (b) MDCT reformat images demonstrating left lumbar hernia with bowel-containing sac (arrows)
Incisional Hernias
Incisional hernias and parastomal hernias occur after a surgery involving the abdominal wall. They occur between 0.5 % and 13 % of patients [8]. Parastomal hernias refer to the protrusion of abdominal contents around an ostomy. They may contain long portions of bowel and are associated to intestinal obstruction (Fig. 18.17) [8, 43].
Fig. 18.17
Axial (a) and coronal (b) MDCT reformat images demonstrating incisional hypogastric hernia with bowel-containing sac following hysterectomy (arrows). Coronal MDCT reformat image (c) demonstrating incisional infraumbilical hernia with bowel-containing sac. There is mild fat stranding (arrow) suggestive of incarceration
Miscellaneous Hernias
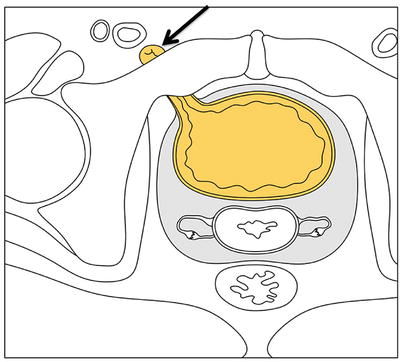
Fig. 18.18
Obturator hernia. Diagrammatic axial view of the pelvis depicting an obturator hernia. The hernia sac (arrow) protrudes through the obturator foramen
Obturator Hernia
Ussually caused by an acquired defect in the obturator membrane allowing protrusion of bowel contents through the obturator canal adjacent to the obturator vessels (Fig. 18.18). Occurs more frequently in thin and older women, who usually have groin pain radiating to the knee due to compression of the obturator nerve (Howship-Romberg sign) or secondary to bowel obstruction [8, 44]. Sciatic hernias occur through the greater sciatic foramen, are rare, and tend to present with complications (Fig. 18.19).
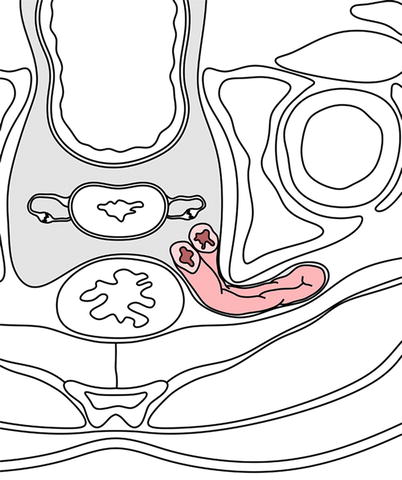
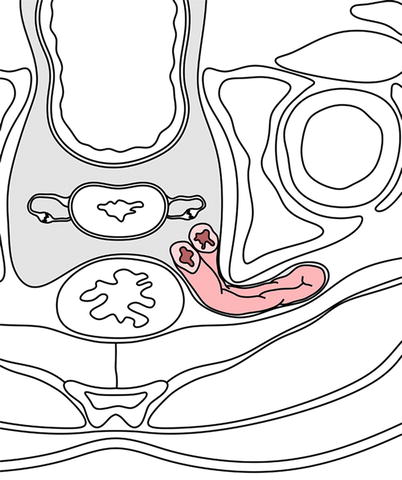
Fig. 18.19
Sciatic hernia. Diagrammatic axial view of the pelvis depicting a sciatic hernia. The hernia sac (arrows) protrudes through the greater sciatic foramen. Note posterior displacement of the piriform muscle, which also exits through the sciatic foramen
Narath’s Hernia
Richter’s Hernia
Littre’s Hernia
Amyand’s Hernia
Amyand’s hernia refers to the presence of the cecal appendix within an inguinal hernia (Fig. 18.20) [8, 45, 46].
Fig. 18.20
Coronal MDCT reformat images (a and b) demonstrating an inguinal hernia containing the cecal appendix (Amyand’s hernia, arrow). There is mild fat stranding (arrows) suggestive of incarceration. No acute appendicitis is noted; however, the incarceration is causing intestinal obstruction (arrowheads)
Laugier’s Hernia
Key Points (Abdominal Hernias)
(a)
Inguinal hernias – most frequent wall hernias
(b)




Direct inguinal hernias – lateral to epigastric vessels, most common in children
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree