Iain D. Morrison, Patrick McLaughlin, Michael M. Maher
Current Status of Imaging of The Gastrointestinal Tract
Imaging Techniques and Radiation Issues
In this section on abdominal imaging, the imaging approach and appearances of lesions in the areas of the oesophagus, stomach, small bowel, large bowel, peritoneum, liver, biliary system and pancreas are covered in their respective chapters. In this chapter the relative merits of different imaging investigation are discussed, with most emphasis being placed on their utility in the acute abdominal pain setting. Issues regarding the radiation dose will be discussed. This becomes increasingly relevant now that computed tomography (CT) is frequently deployed early on in the management of patients with acute abdominal pain.
The plain abdominal radiograph (AXR) was for generations the staple investigation in the acute abdomen. Now there are many situations where CT or ultrasound (US) should be the first imaging investigation after clinical assessment of the patient. There are still scenarios where the AXR is very useful, and these will be discussed together with advice on interpretation, which can be difficult.
The Plain Abdominal Radiograph
For non-acute situations, the relatively small yield of information from a plain radiograph does not justify the radiation dose that it entails. There are exceptions, such as in the follow-up of renal calculi and in assessment of bowel transit times in constipation.
In the situation of the acute abdomen, a supine abdomen radiograph and an erect chest radiograph (CXR) can be regarded as the basic standard radiographs. The erect CXR is invaluable in diagnosing visceral perforation since the X-ray beam is passing through any free gas under the diaphragm at an optimum angle, and at the correct exposure for visualisation. For this investigation the patient should ideally remain in the erect position for 10 min before radiography to allow time for any free gas to rise to the highest point, although this may not be achieved in practice. The supine radiograph should ideally be taken with an empty bladder, and should include the area from the diaphragm to the hernial orifices, which in practice means that the obturator foramina should be included.
Historically, an erect abdominal radiograph was performed additionally for the acute abdomen in order to assess the number and length of any fluid levels within bowel. This was thought to distinguish between obstruction and ileus. However, this distinction is highly unreliable, and evidence shows that the erect abdominal radiograph can be misleading.1 The erect CXR appearances can be confusing when looking for free peritoneal gas, as discussed later in this chapter. Occasionally a left lateral decubitus radiograph can clarify, since small amounts of gas can be seen over the liver if there has been a perforation.
In the acute abdominal setting, plain radiography should only be requested in situations where it is likely to yield useful and not misleading information. Plain radiography is useful in diagnosing perforation of a viscus, and for assessing bowel dilatation (the main valid indications; see Table 25-1). Plain abdominal radiography is not helpful in diagnosing the common inflammatory conditions of the abdomen such as appendicitis, diverticulitis, cholecystitis and pancreatitis. For this reason, plain radiography should be avoided in these situations unless there is the suspicion of perforation or bowel dilatation. Clinical assessment, US and CT all play a role in these inflammatory conditions.
Abnormal Gas Distribution
Pneumoperitoneum
When analysing a plain radiograph of the abdomen, it is important to be able to attribute all the gas to normal anatomical structures, namely viscera. There are numerous causes for gas in abnormal places; the most frequent is pneumoperitoneum, but other causes include gas in the retroperitoneum, gall bladder, biliary tree, liver, kidneys, bladder and abscesses.
The presence of free intra-abdominal gas almost always indicates perforation of a viscus, for instance a peptic ulcer. Other causes include obstruction, inflammatory conditions, bowel ischaemia and colonoscopy. About 70% of perforated peptic ulcers will demonstrate free gas, a phenomenon rarely seen in the case of a perforated appendix. Small amounts of gas are detectable under the right hemidiaphragm on an erect CXR, outlining the smooth surface of the liver clearly (Fig. 25-1), but on the left it can be difficult to distinguish free gas from stomach and colonic gas. The diaphragm is seen as a relatively thin structure outlined by gas below, and lung above. The gas under the right and left hemidiaphragms may join across the middle (cupola sign). There are many circumstances when interpretation of an erect CXR is difficult. Table 25-2 lists the most frequent situations when the radiologist or clinician may be fooled into thinking that there is a perforation (pseudo-pneumoperitoneum). A lateral decubitus radiograph can resolve the problem by demonstrating gas between the liver and the abdominal wall, but nowadays CT is usually requested when there is doubt. Since interpretation of the plain AXR can be unreliable, it is important to interpret the plain radiographic findings in the light of the clinical findings.

It is also important to be able to recognise the signs of pneumoperitoneum on supine AXRs, for example in patients being monitored for colitis. In many patients, particularly those who are unconscious, have suffered trauma, are old or are critically ill, perforation may be clinically silent as it is overshadowed by other serious medical or surgical problems. In around half of patients with a pneumoperitoneum, gas may be detectable on the supine radiograph.2 Almost half will have gas in the right upper quadrant adjacent to the liver, lying mainly in the subhepatic space and the hepatorenal fossa (Morrison’s pouch). Visualisation of both the outer and inner walls of a bowel loop is known as Rigler’s sign (Fig. 25-2). The bowel loops then take on a ‘ghost-like’ appearance. This sign can be difficult if several loops of bowel lie close together. The falciform or medial umbilical ligaments may be demonstrated by free gas lying on either side (Fig. 25-3). Air can be seen in the fissure for the ligamentum teres.3 The signs are listed in Table 25-3.
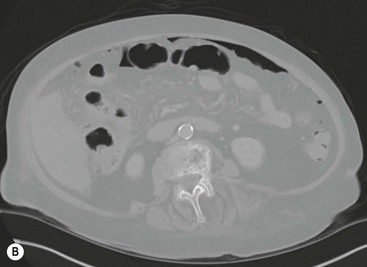
CT is the most sensitive investigation for the detection of free peritoneal gas. Small volumes of free peritoneal gas can be seen over the liver and anteriorly in the central abdomen. Tiny pockets of free gas can also be seen in the peritoneal recesses. In order not to miss small amounts of free gas, the images should be reviewed on broad window settings (Fig. 25-4).
There are a number of causes of pneumoperitoneum without peritonitis. These are listed in Table 25-4.
TABLE 25-4
Causes of Pneumoperitoneum without Peritonitis

Gas in Bowel Wall
If linear gas streaks are seen in the bowel wall, intestinal infarction should be suspected. Intestinal infarction is a most serious condition caused by thrombosis or embolism of the superior mesenteric artery. Other radiological signs are non-specific, consisting of slightly dilated loops of small bowel that may be gas-filled, or poorly seen when mainly fluid filled. The walls of the small-bowel loops may be thickened due to submucosal haemorrhage and oedema (Fig. 25-5). Free gas may be present if perforation has occurred. Intraluminal gas in the mesenteric veins or portal vein may be seen in advanced cases. These features can be readily demonstrated on CT.
Pneumatosis cystoides intestinalis is an uncommon condition consisting of cyst-like collections of gas in the walls of hollow viscera. The aetiology is unknown, but there is an association with obstructive airways disease. The left hemicolon is the most common site, and the term pneumatosis coli is used to describe it. Most patients are past middle age; symptoms include vague abdominal pain, diarrhoea, constipation and mucus discharge. The cysts vary in size from 1 to 3 cm and lie both in the subserosa and submucosa. The plain radiographic appearances are characteristic, the gas-containing cysts giving rise to an appearance quite different from normal gas shadows (Fig. 25-6). Intermittently and subclinically these cysts rupture, producing a pneumoperitoneum without evidence of peritonitis. It is important to recognise pneumatosis as the cause of the pneumoperitoneum in such cases so as to avoid an unnecessary laparotomy.
Gas in Retroperitoneum
Gas can escape into the retroperitoneum, and the causes for this include perforation of a posterior peptic ulcer, perforated sigmoid diverticular disease, colonoscopy and other iatrogenic causes. The gas may be best visible in the layers of the abdominal wall in the flanks, or around the kidneys (Fig. 25-7). Retroperitoneal gas can track superiorly into the mediastinum, and inferiorly into the buttock and thigh. Gas in the soft tissues of the left thigh is a classical site for gas from a diverticular perforation.
Gas in Other Organs
Gas may also be identified in the biliary tree, portal veins, renal collecting systems (emphysematous pyelonephritis, Fig. 25-8), pancreas (infected necrosis or abscess), gall bladder wall and urinary bladder.
Dilatation of Bowel
Dilatation of the bowel occurs in mechanical intestinal obstruction, paralytic ileus and air swallowing. The radiological differentiation of these different causes depends mainly on the size and distribution of the loops of the bowel, and clinical correlation is essential.
Gastric Dilatation
Gastric dilatation can be caused by many conditions. Mechanical gastric obstruction may be benign, malignant or from extrinsic compression. It often leads to a huge fluid-filled stomach that retains its gastriform shape with little or no bowel gas beyond. This compares with the normal small gastric air bubble, usually just enough for the stomach to be identified. Paralytic ileus (often referred to as acute gastric dilatation) occurs mostly in elderly people, usually associated with considerable fluid and electrolyte disturbance.
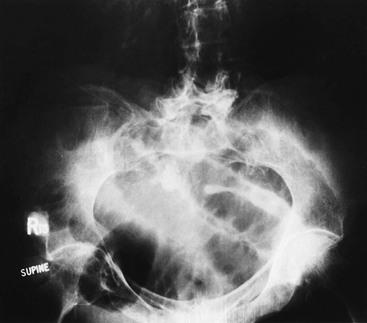
Gastric volvulus is relatively rare and may result from twisting of the organ around its longitudinal or mesenteric axis. There is usually a collapsed small bowel, and virtually no gas is seen beyond the stomach. The stomach loses its gastriform shape and becomes spherical (Fig. 25-9). If oral contrast medium is given, there may be complete obstruction in the lower oesophagus, or if contrast medium does enter the stomach, it may not pass beyond the obstructed pylorus. After resuscitation and intubation, large amounts of gas can be seen in a dilated stomach. This sometimes occurs after air swallowing alone.
Distinction between Small- and Large-Bowel Dilatation
When a radiograph shows dilated bowel it is important to try to determine whether it is small or large bowel, or both. Useful differentiating features include the size and distribution of the loops. Dilated small-bowel loops are usually more numerous and arranged centrally in the abdomen. The loops show a small radius of curvature and rarely exceed 5 cm in diameter. The small-bowel folds (valvulae conniventes) form thin, frequent complete bands across the bowel gas shadow, prominent in the jejunum but becoming less marked in the ileum. The valvulae conniventes are much closer together than colonic haustra and become thinner when stretched, but still remain relatively close together as the calibre of the small bowel increases (Fig. 25-10). If the small-bowel blood supply is compromised, however, and the bowel becomes oedematous or gangrenous, the valvulae conniventes may become thickened.
Problems in distinguishing the distal ileum from the sigmoid colon are relatively frequent as both may be smooth in outline and occupy a similar position, low in the central abdomen. Although haustra usually form thick incomplete bands across the colonic gas shadow, they sometimes form complete transverse bands, depending on the orientation of the loop. Haustra may be absent from the descending and sigmoid colon but can usually still be identified in other parts of the colon, even when it is massively distended.
Small-Bowel Dilatation
Small-bowel dilatation may be due to mechanical obstruction or paralytic ileus/pseudo-obstruction. In paralytic ileus there is no obstructing lesion. Small and large bowel may be dilated. Peritonitis and a postoperative abdomen are common causes, but there are many others including small-bowel ischaemia, metabolic disturbances, renal failure, drugs such as morphine and general debility. CT is valuable in determining whether there is an abrupt calibre change, which would point to a genuine small-bowel obstruction (SBO).
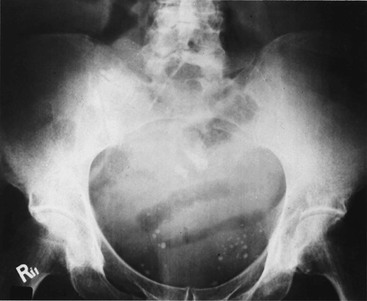
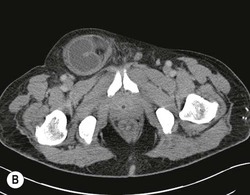
The causes of SBO are myriad, but can be largely divided into mural lesions (e.g. tumour, stricture due to Crohn’s disease, irradiation), luminal (bezoar, gallstone, Ascaris lumbricoides bolus, intussusception) and extrinsic (adhesions, hernia, volvulus, abdominal malignancy). In the developed world the most common cause of SBO is adhesions due to previous surgery, the obstruction being caused by a strangulated hernia in less than 10%.4 In the undeveloped world, however, nearly three-quarters of cases are caused by a strangulated hernia. Mechanical obstruction of the small bowel normally causes small-bowel dilatation, with an accumulation of both gas and fluid, and a reduction in the calibre of the large bowel. On the plain radiograph it is important to look for a hernia, which may be identified as a gas-filled viscus below the level of the inguinal ligament (Fig. 25-11). Visualisation of a hernia does not always mean that it is the cause of the SBO.
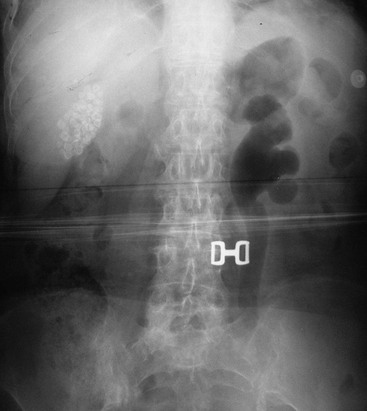
Dilated loops of small bowel are readily identified if they are gas-filled on the supine radiograph. The string of beads sign, caused by a line of gas bubbles trapped between the valvulae conniventes, is seen only when very dilated small bowel is almost completely filled with fluid, and is virtually diagnostic of SBO. In a proportion of patients with SBO, the plain radiograph appears normal or only equivocally abnormal, since the dilated loops are mainly fluid-filled. Completely fluid-filled loops are not easily identified on plain radiographs, but are readily seen on CT (Fig. 25-12). The plain AXR has a sensitivity of around 66% for SBO.5
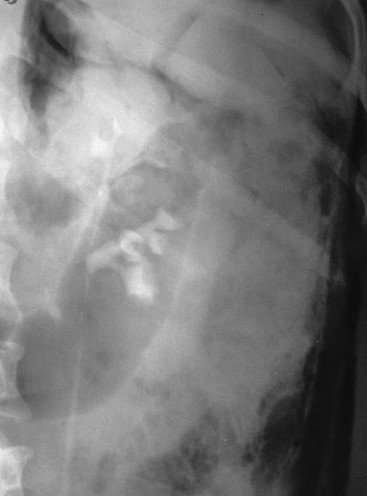
Where a gallstone is the cause of obstruction, this is known as gallstone ‘ileus’ (technically an obstruction, not an ileus). The gallstone passes into the duodenum by eroding the inflamed gall bladder wall. This condition is well known to clinicians, but relatively rare, accounting for about 2% of patients presenting with SBO. The diagnosis is frequently delayed or missed even though the characteristic radiological features of gallstone ileus are present in 38% of cases.6 Over half the patients will have plain radiographic evidence of intestinal obstruction, and about one-third will have gas present in the biliary tree (Fig. 25-13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree