Cystic Fibrosis
Gerald F. Abbott, MD
Key Facts
Terminology
Cystic fibrosis (CF): Hereditary disorder that affects gene regulating chloride transport
Accounts for up to 25% of adult cases of bronchiectasis
Imaging Findings
Diffuse bronchiectasis with predominant involvement of upper lobes
Right upper lobe often 1st and most severely affected
Airways primary site of pathology in CF
Bronchial wall thickening earliest finding
Bronchiectasis most common finding; diffuse involvement, usually predominant in both upper lobes
Hyperinflation early finding; may be reversible initially, then permanent (100%)
CT more sensitive to deterioration in clinical status than pulmonary function tests
Role of CT tempered by large life-time radiation dose
Top Differential Diagnoses
Allergic Bronchopulmonary Aspergillosis
Immotile Cilia Syndrome
Tuberculosis
Clinical Issues
Patients with mild disease may be asymptomatic and not diagnosed until adulthood
Diagnostic Checklist
CF in any adult with unexplained bronchiectasis
TERMINOLOGY
Abbreviations and Synonyms
Cystic fibrosis (CF), mucoviscidosis
Definitions
Hereditary disorder that affects gene regulating chloride transport
Production of abnormal secretions from exocrine glands (salivary and sweat glands, pancreas, large bowel, tracheobronchial tree)
Thick viscous secretions affecting multiple organs, primarily lungs and pancreas
Accounts for up to 25% of adult cases of bronchiectasis
IMAGING FINDINGS
General Features
Best diagnostic clue: Diffuse bronchiectasis with predominant involvement of upper lobes
Patient position/location
Predominant abnormalities in upper lobes
Right upper lobe often 1st and most severely affected
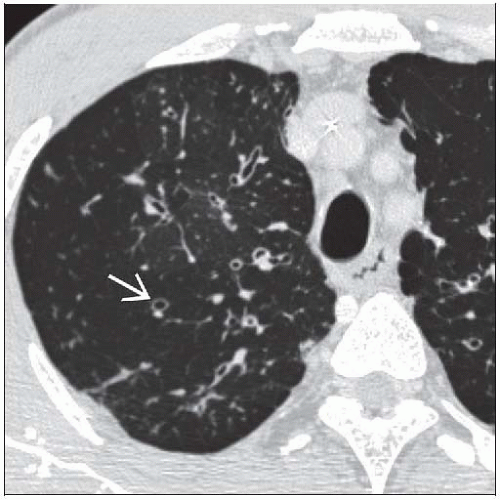
CT Findings
Airways
Primary site of pathology in CF
Bronchial wall thickening earliest finding
Due to inflammation or infection of airway wall; precedes development of bronchiectasis
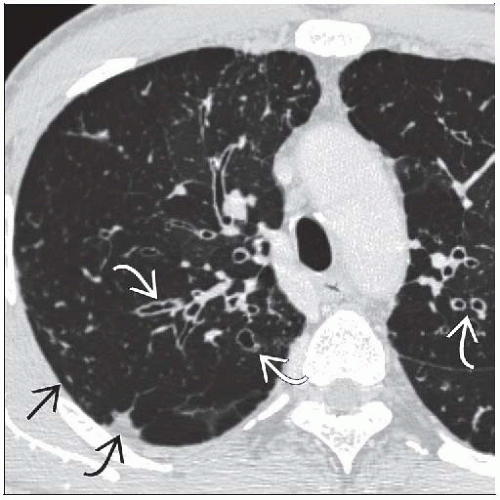
Bronchiectasis most common finding; diffuse involvement, usually predominant in both upper lobes
Mucous plugging manifests as centrilobular nodular, tubular, and V- or Y-shaped (tree-in-bud) opacities
Lung
Air-trapping
Hyperinflation is early finding; may be reversible initially, then permanent (100%)
Mosaic lung attenuation
Recurrent areas of consolidation
May represent superimposed pneumonia or atelectasis and retained secretions distal to bronchial obstruction
Cystic or bullous changes may occur, typically subpleural in upper lobes (predisposes to pneumothorax) in end-stage disease
Cardiac
Acute increase in heart size (cor pulmonale; ominous clinical sign)
Pulmonary arterial hypertension in end-stage disease
Associated findings
Mild lymphadenopathy (reactive) common
Pleural effusions uncommon
Evolution
Early
Mild bronchial wall thickening
Regional (lobular) air-trapping
Centrilobular nodules (from mucus plugging in peripheral airways)
Moderate progression
Increased bronchial wall thickening
Development of cylindrical bronchiectasis
Increased air-trapping (segmental to lobar)
End-stage
Progression to varicose or saccular bronchiectasis
More proximal mucus plugging
Chronic lobar collapse
Correlation with pulmonary function
Dissociation between progressive structural damage evidenced by CT and stable or improved pulmonary function tests in many patients
CT more sensitive to deterioration in clinical status than pulmonary function tests
Scoring systems: Bhalla and others
Shown to have good interobserver agreement
No consensus yet as to which is most appropriate for evaluating new therapies or monitoring disease
Radiographic Findings
Radiography
Less sensitive for earliest changes in CF
Primary role is longitudinal assessment
Angiographic Findings
Bronchial artery embolization for hemoptysis
Imaging Recommendations
Best imaging tool
Chest radiography every 2-4 years recommended by Cystic Fibrosis Foundation
Annually for those with frequent infections or declining lung function
CT role currently being defined
Now being used as outcome measure for therapeutic trials
Protocol advice
Role of CT tempered by large life-time radiation dose
1st CT often in childhood
Chest CT average dose of 6 mSv
Radiation dose reduction important
Incremental CT vs. volumetric scans (reduces dose 8x)
Lower mAs to 20 (reduces dose 10x from typical mAs of 200)
DIFFERENTIAL DIAGNOSIS
Allergic Bronchopulmonary Aspergillosis
Central upper lobe predominant bronchiectasis
History of asthma, often eosinophilia
10% of patients with CF have allergic bronchopulmonary aspergillosis (ABPA)
Immotile Cilia Syndrome
Not upper lobe predominant
Dextrocardia or situs inversus; sinusitis also common
Postinfectious Bronchiectasis
Usually unilateral, lobar, or sublobar; often lower lobe (except for tuberculosis)
Williams-Campbell Syndrome
Rare; congenital deficiency of cartilage in subsegmental bronchi
Bronchiectasis limited to 4th-6th generation bronchi
Tuberculosis
Reactivation can produce upper lobe volume loss; bronchiectasis in 50%
Often associated with calcifications in pulmonary granulomas and hilar mediastinal lymph nodes
Ankylosing Spondylitis
Upper lobe bronchiectasis and cystic lung disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree