Clinical Presentation
The patient is a 72-year-old male whose chief complaint is left mid back pain. He states it has been going on for approximately 2 weeks. He says it is a sharp pain in the middle of his back that is elicited by certain types of movements, sneezing, coughing, or getting up from a chair. There is no clear history of trauma. He is afebrile. Recent laboratory evaluations including white blood cell count, C-reactive protein, and sedimentation rate are normal.
Imaging Presentation
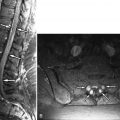
Sagittal T1 and fat-saturated T2-weighted magnetic resonance (MR) images of the thoracic spine reveal decreased T1 and increased T2 signal intensity symmetrically involving the anterior endplates of a mid thoracic level with mild anterior disc height loss compatible with type 1 vertebral endplate disease (VED) ( Fig. 18-1 ) .

Discussion
Signal changes in the vertebral endplates and marrow are commonly seen on MR imaging of the spine. Three patterns/types were originally described by DeRoos in 1987 and later became known to the general radiology population as Modic changes. VED, particularly type 1, has been demonstrated to be strongly associated with back pain.
VED type 1 has been described as disruption and fissuring of the endplate with regions of degeneration, regeneration, and vascular granulation tissue. VED type 2 has been described as disruption of the endplates with increased reactive bone and granulation tissue, and the hematopoetic elements in the vertebrae are replaced by abundant fat (yellow marrow). VED type 3 is presumed to be related to bone sclerosis.
The prevalence of VED in patients with degenerative disc disease of the lumbar spine ranges between 19% and 59%, with types 1 and 2 being the most common and type 3 being more rare. VED is most commonly seen at the L4-5 and L5-S1 levels and appears to increase with advancing age. VED is uncommon in asymptomatic individuals. Weishaupt and colleagues demonstrated a presence of VED in less than 10% of asymptomatic volunteers ages 20 to 50 and only one case of type 1 VED in 300 patients.
Several theories have been proposed as to the pathogenesis of VED. One theory suggests that VED is caused by a bacterial infection of the disc and another that microtraumas/fractures occur in the endplate. Each of these can predispose the endplate and marrow to inflammatory change. Type 1 changes have a similar appearance to inflammation on MR imaging (MRI). Histologic and biochemical analyses support type I changes being an inflammatory condition. During surgery, Ohtori removed the endplates of 14 patients with low back pain and VED types 1 and 2, and 4 patients without VED. Markers of inflammation, specifically tumor necrosis factor (TNF) and protein gene product (PGP) 9.5 were significantly higher in the endplates of those with VED as opposed to those without; 86% of the VED patients had PGP 9.5 as opposed to none of the controls. TNF was found in both the study group and the control group, but was significantly higher in the VED group and significantly higher in type 1 patients when compared with type 2 patients. Whether or not the patient has VED, very few PGP 9.5 fibers were present in the vertebral marrow and no TNF was observed in the marrow. The presence of these proinflammatory substances could explain why VED causes pain and why patients with type 1 VED are more strongly associated with pain. Rannou and colleagues studied highly sensitive C-reactive protein (hsCRP) in groups of patients without VED, with VED type 1, and with VED type 2 and found the levels of this highly sensitive marker of low grade inflammation to be significantly higher in the type 1 group than in those in the type 2 group or in those without VED. This would further suggest that type 1 changes may reflect inflammation.
Many studies portend that type 1 VED is unstable and that type 1 changes may increase in size, convert to type 2 changes, or go back to normal in a short time. Mitra and colleagues showed an improvement in low back pain symptoms on conversion from type 1 to type 2 or to normal. Type 2 changes tend to remain stable for much longer.
Imaging Features
Plain radiographs and computed tomography (CT) images are very insensitive to the early changes of VED (types 1 and 2). These imaging modalities can detect the endplate sclerosis of type 3 VED. Nuclear medicine bone scan will demonstrate nonspecific increased radiotracer uptake in an area of active bone turnover and thus will be most intense with type 1 VED ( Fig. 18-2 ) and less so with type 2 or type 3. Fluorodeoxyglucose positron emission tomography (FDG-PET) imaging does not demonstrate increased activity in areas of VED; however, this modality can be used to distinguish between severe discogenic vertebral endplate degenerative changes from vertebral osteomyelitis. MRI is the imaging modality of choice for detecting and diagnosing VED; however, because VED is not a fast-acting process, it would be inappropriate to follow patients with VED with short-term MRI examinations. VED appears as bands of signal intensity that are parallel to the vertebral endplates.
- 1
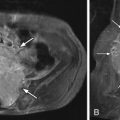
MR imaging of type 1 VED demonstrates signal intensity that reflects its inflammatory nature: decreased T1 signal intensity, increased T2 signal intensity, and usually pronounced enhancement. There may also be linear enhancement of the intervertebral disc ( Fig. 18-3 ) .

Figure 18-3
Type 1 Vertebral Endplate Disease (VED), MR Image.
Sagittal T1 ( A ), fat-saturated T2 ( B ) and post-contrast, fat-saturated T1 ( C ) images. L1-2 vertebral endplates are of decreased T1 signal intensity, increased T2 signal intensity, and enhanced consistent with its inflammatory nature. The T2 abnormality can be obscured by normal fatty marrow if a fat-saturated pulse sequence is not used.
- 2
MR imaging of type 2 VED demonstrates signal intensity that reflects its fatty nature: increased T1 signal intensity, increased T2 signal intensity, and usually without evidence of enhancement ( Fig. 18-4 ) .