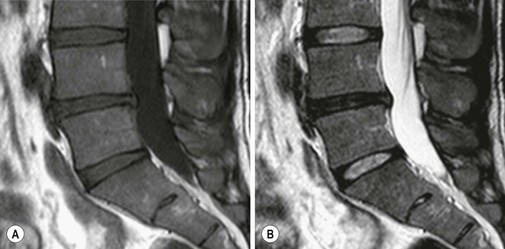
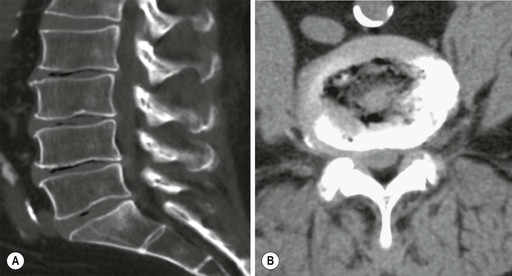
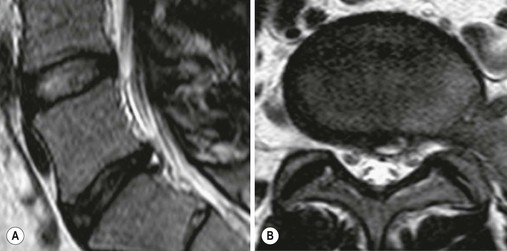
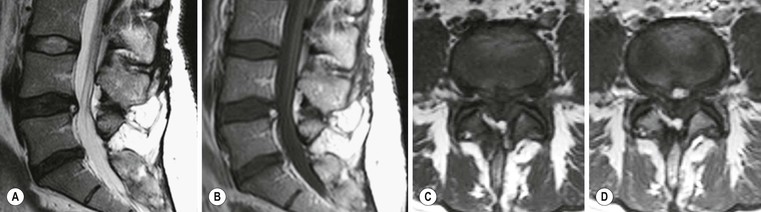
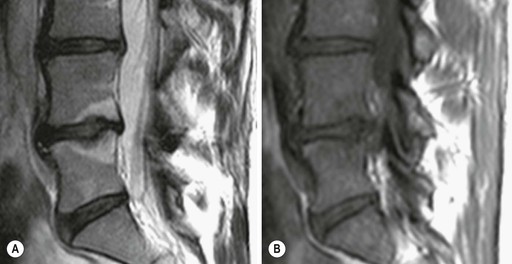
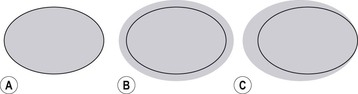
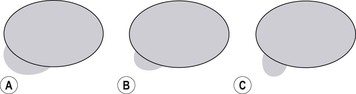
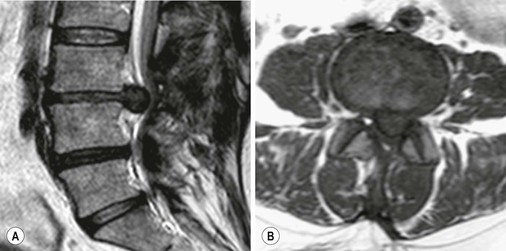
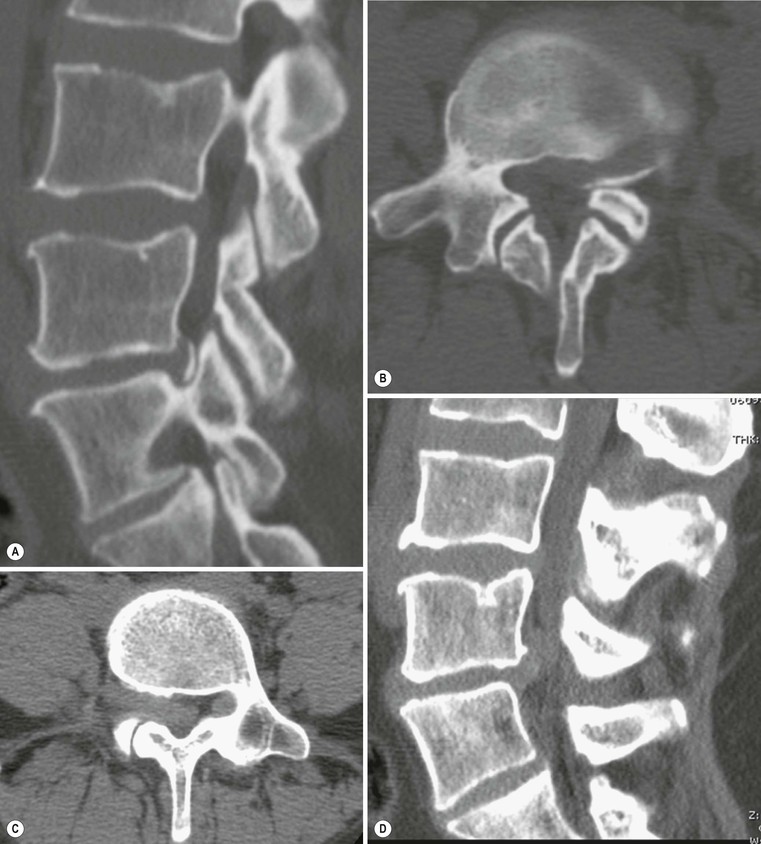
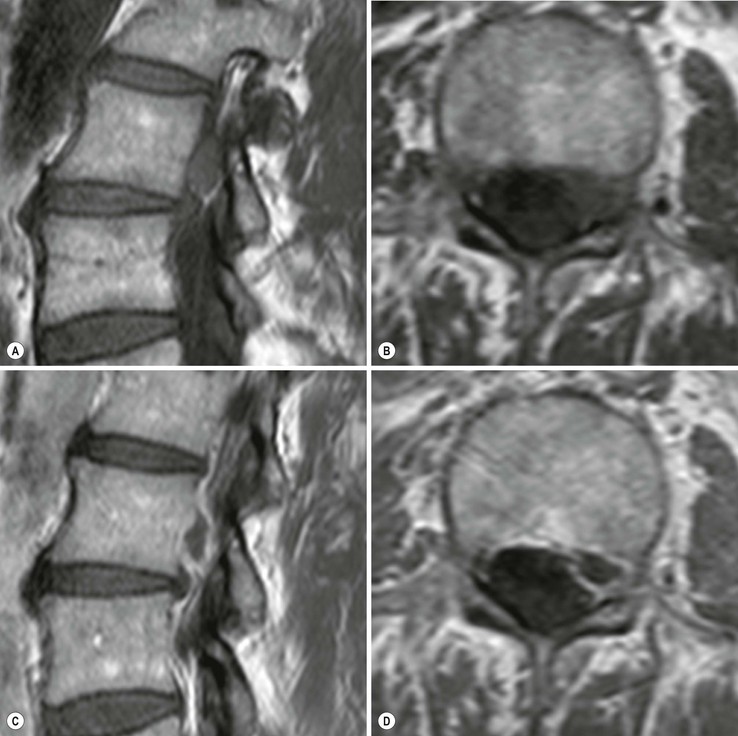
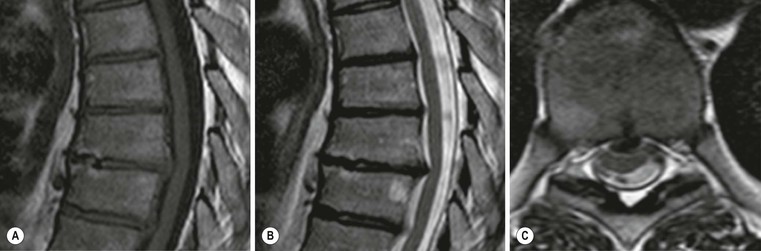
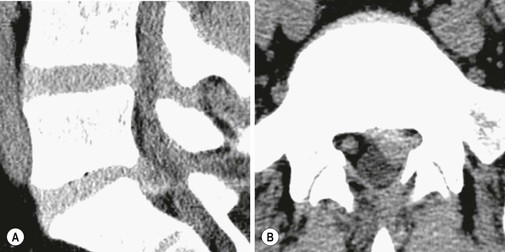
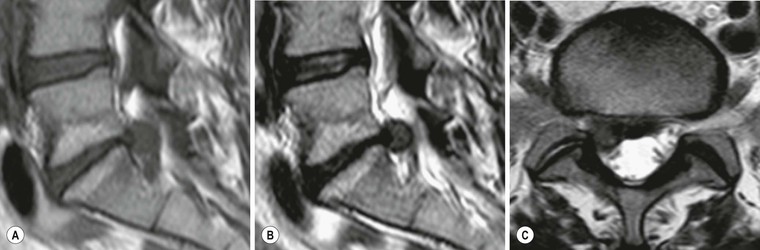
Paul M. Parizel, Thomas Van Thielen, Luc van den Hauwe, Johan W. Van Goethem The spine is a complex anatomical structure composed of vertebrae, intervertebral discs and ligaments. All of these structures may undergo degenerative and morphological changes with age. The intervertebral discs form the connection between two adjacent intervertebral bodies and have two main functions: allowing movement of the spine and to serve as shock absorbers. Movement at a single level is limited; the combined movement of multiple levels allows a significant range of motion. The cervical and lumbar spine, compared with the thoracic spine, has relative more disc height so the motion in these parts is greater. In the posterior region the facet joints play an important role in the cause of neck and low-back pain. Facet joint syndrome is a range of symptoms that cannot be linked to a single nerve root pattern. Since the first description of a ‘ruptured disc’ by Mixter and Barr in 1934 with monoradiculopathy,1 the terminology to grade and report degenerative disease of the spine has been controversial and confusing. Some nomenclature systems are based on description of the observed morphology of the disc contour while others include the pathological, clinical and anatomical features. Cross-sectional imaging is based on other definitions and concepts compared to myelography or discography.2 In 2001 a new nomenclature was proposed by the Combined Task Forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology which consists of a classification system for the reporting on imaging studies based on pathology.3 In this chapter we shall follow the general classification of disc lesions as proposed by the Combined Task Forces. The general classification as proposed by Milette is given in Table 55-1.4 TABLE 55-1 General Classification of Disc Lesions The Combined Task Forces reserved the term ‘normal’ for young discs that are morphologically normal, without signs of disease, trauma or ageing. The normal appearance of an intervertebral disc, however, is age-related due to biochemical and anatomical changes which result in a variable appearance on MRI.5 In infants and young children, the intervertebral disc is prominent relative to the height of the adjacent vertebral bodies. With increasing age the disc volume decreases. The transition between the nucleus pulposus and the annulus is sharp and becomes less distinct with age.6 In young adults the disc contour coincides with the margins of the adjacent vertebral endplates. On MR imaging the normal adult disc has a low to intermediate signal on T1-weighted images and a high signal intensity on T2-weighted images relative to the bone marrow in the adjacent vertebral bodies.6 On T2 the bright nucleus pulposus is indistinguishable from the inner annulus. The normal adult endplates, the outer annulus fibrosus and the ligamentous structures are hypointense on T1 and T2. The outer annulus is visualised on T2 and has a low signal intensity.7 In young adults diurnal changes in T2 relaxation are present; these changes disappear after the age of 35 years and are thought to be a normal aspect of ageing.8 In the third decade the intranuclear cleft appears as a horizontal band of decreased signal intensity on T2 in the central part of the discs, giving it a bilocular appearance on sagittal images. It resembles a fibrous transformation of the gelatinous matrix of the nucleus pulposus. In middle-aged and elderly patients there is a gradual signal loss of the intervertebral discs on the T2 images until the disc become hypointense.9 The loss of signal is best seen on T2 and correlates to a decrease in water and proteoglycan content and increase in collagen. Though the decrease in T2 signal of the intervertebral disc is age-related it predisposes to degenerative changes in the discs such as loss in disc height, disc herniation and annular tears (Fig. 55-1). The highest T2 values are seen near the vertebral endplates and the lower T2 values are present in the intranuclear cleft and the peripheral annulus fibrosus due to its fibrous nature. In general in the normal ageing disc the height is preserved, disc margins remain regular and radial annular tears are not a usual consequence of ageing. On the basis of a series of post-contrast MRI studies of the lumbar spine, degeneration and normal ageing have been shown to be two separate processes.10 Resnick and Niwayama conclude there are two different processes of degeneration: a first type, which can be considered normal ageing, involves the annulus fibrosus and adjacent ring apophysis (spondylosis deformans) (Fig. 55-2); the second type, called intervertebral osteochondrosis, affects the nucleus pulposus and the vertebral endplates, corresponding to the pathological ageing process.11 Anterior and lateral marginal osteophytes are considered as normal ageing while endplate changes and reactive bone marrow are seen as pathological changes. Large amounts of gas in the central disc space seen on X-ray or CT studies are indicative for pathological intervertebral osteochondrosis while small amounts of gas near the apophyseal enthesis should be considered as spondylosis deformans (Fig. 55-3). The prevalence of degenerative disc disease is linearly related to age. Intervertebral disc degeneration begins early in life.12 Many other factors (e.g. biomechanical and quality of collagen) are also implicated. Degeneration includes changes involving the endplates (sclerosis, defects, Modic changes and osteophytes) as well as disc changes (fibrosis, annular tears, desiccation, loss of height and mucinous degeneration of the annulus). The relation between low-back pain and abnormalities in the lumbar spine is controversial as abnormal findings are often seen in asymptomatic patients on plain radiographs, CT studies and MRI studies.13 Degenerative changes in the disc are already seen in one-third of healthy persons between 21 and 40 years old. The high prevalence of asymptomatic disc degeneration must be taken into account when MRI is used for assessment of spinal symptoms. Although the validity of disc height as an indication for degenerative disc changes is questionable, the loss of height of the intervertebral space is the earliest sign of disc degeneration on plain radiographs. Loss of disc height has been reported in asymptomatic subjects, indicating there is no direct relationship between clinical symptoms and imaging findings. The position of the patient (lying down or standing) should be taken into account. Other signs, including sclerosis of the vertebral endplates, osteophytes, vacuum phenomenon and calcification, are more reliable, though they indicate late degenerative changes. Signal loss on T2 is an early indicator of intervertebral disc degeneration on MRI.9 As described earlier, in normal ageing the decrease in signal intensity on T2 should be uniformly distributed over the different levels. If the signal loss is only seen in one or two levels this should be interpreted as abnormal. This finding is often referred to as ‘a black disc’, and has been applied to describe discogenic pain syndrome (Fig. 55-1). The degenerative process typically starts at the levels with the highest mechanical stress (motion/weight bearing). In the cervical spine, levels C5–C6 and C6–C7 are most commonly involved and in the lumbar spine the levels L5–S1 and L4–L5. With ageing, the intervertebral disc becomes more fibrous and less elastic. The degenerative changes are accelerated when the structural integrity of the posterior annulus fibrosus is damaged by overload. This will eventually lead to formation of fissures in the annulus fibrosus. In the international literature the term ‘annular tear’ is the most widely used and is also supported by the Combined Task Forces; however, the terminology ‘annular fissure’ is also used. One should take into account that ‘annular tear’ does not imply this is caused by trauma. Annular tears can be divided into concentric, transverse or radial tears:14 • Transverse tears or ‘rim lesions’ are horizontal ruptures of the Sharpey’s fibres near the insertion in the bony ring apophysis. The clinical significance of transverse tears remains unclear, although some authors believe they influence and accelerate degeneration and are associated with discogenic pain.14 They are believed to be post-traumatic in origin and are often associated with small osteophytes. • Radial tears are annular tears permeating from the deep central part of the disc and extend outwards toward the annulus in either the cranio-caudal or the transverse plane (Fig. 55-4). Most of these tears do not reach the pain-sensitive outer layers of the annulus. Radial annular tears are associated with disc degeneration14 and a complete radial tear is necessary for progressive deterioration of the disc.15 The clinical significance of annular tears remains unclear. Some annular tears can cause low-back pain without the presence of modification of the disc contours, also known as discogenic pain.16 On the other hand, annular tears are often found in asymptomatic patients and can be seen as a part of the ageing process.17 On MRI annular tears can be seen as an area of high signal intensity on T2 or as foci of annular enhancement on gadolinium-enhanced T118 (Fig. 55-5). On T2 the signal intensity is the same as the adjacent cerebrospinal fluid. Repetitive microtrauma may cause annular tears to enlarge and become inflamed; this can be seen as an area of increased signal intensity. This phenomenon is seen on T2 and is known as a high intensity zone (HIZ).19 The HIZ is a combination of radial and concentric annular tears which merge in the periphery of the disc. The presence of a high intensity zone is believed to be related to discogenic pain as it involves the outer, highly innervated layers of the annulus. The value of this sign is, however, limited due to a poor sensitivity and a limited positive predictive value.20 On T1 extradural inflammation is seen as a zone of intermediate signal intensity, replacing the fat between the disc and the dural sac; on post-contrast images there is intense enhancement. In the cervical spine annular tears, rim lesions and prolapsed disc material are poorly recognised on MRI, even in severely degenerative disc.21 In the thoracic spine herniated disc fragments are often associated with abnormal straight or curvilinear densities on CT, also known as the ‘nuclear trail sign’. On MRI this finding may also be associated with a comet-tail configuration in the axial plane. This sign indicates advanced disc disruption and degeneration and must be distinguished from an ageing disc that has not failed. Herniation is defined as a displacement of disc material (cartilage, nucleus, fragmented annular tissue and apophyseal bone) beyond the limits of the intervertebral disc space.3 The definition of the intervertebral disc is the three-dimensional volume defined by the adjacent vertebral endplates and the outer edges of the vertebral ring apophysis, excluding osteophytes. A break in the vertebral endplates or disruption of the annulus fibrosus is thus necessary for disc displacement to occur. Disc herniations through one or both vertebral endplates are called intervertebral herniations. These herniations are also called Schmorl’s nodes and are often surrounded by reactive bone marrow changes (Fig. 55-6). One hypothesis is that this type of herniation is caused by a weak spot in the vertebral endplate caused by regression of the nutrient vascular canals leaving a scar.22 When in young individuals a herniation of the nucleus pulposus through the ring apophysis occurs before bony fusion a small segment of the vertebral rim may become isolated.23 This is called a limbus vertebra and is most commonly found in the lumbar region and less frequently on the mid-cervical level. They are characterised by a defect in the anterior wall of the vertebra and usually at the anterior superior margin in the lumbar spine and at the anterior inferior margin at cervical level. A ‘bulging’ of the disc is defined as a circumferential or generalised disc displacement involving more than 50% of the disc circumference and is not considered as being a disc herniation (Fig. 55-7). The term ‘bulging’ is not correlated with pathology or aetiology but only refers to the morphological characteristics. A bulging can be physiologically seen on the level L5–S1 and on mid-cervical level, can reflect advanced degenerative changes, can be a pseudo-image caused by partial volume effect, can be associated with bone remodelling or can occur in ligamentous laxity.3 There are two types of disc bulging: an asymmetrical type, as frequently seen in scoliosis, or the symmetrical type, with equal displacement of the disc in all directions. Two types of disc herniations can be differentiated on the basis of the shape of the displaced disc material (Fig. 55-8). A disc herniation is called an ‘extruded disc’ when the base against the disc is smaller than the diameter of the displaced disc material, measured in the same plane (Fig. 55-9). A ‘disc protrusion’ is used when the base of the disc is broader than any other diameter of the displaced disc material (Fig. 55-10). A protruded disc can be focal if < 25% of the disc circumference is involved or broad-based when 25–50% of the disc circumference is involved. When there is no connection between the disc and the displaced disc material, this is called a sequestrated fragment or free fragment and is also described as a disc extrusion (Fig. 55-11). On imaging studies, it is often impossible to determine whether continuity exists. Therefore it is more practical to use the term ‘migration’, which signifies displacement of disc material away from the site of extrusion regardless of the continuity (Fig. 55-12). The Combined Task Forces have maintained the distinction between protrusion and extrusion, which is useful because an extrusion is seldom seen in asymptomatic patients.24 The term ‘disc extrusion’ is also more acceptable to patients than ‘disc herniation’. A ‘contained’ herniation refers to the displacement of disc material which is covered by the annulus fibrosus. If this cover is absent, the herniation is ‘uncontained’. With discography it is possible to distinguish a contained from an uncontained disc herniation and separate a leaking from a non-leaking disc, depending on the displacement of injected contrast agent. On cross-sectional imaging (CT or MRI) it is often impossible to differentiate contained from uncontained disc extrusions. Communication with clinicians requires an accurate and simple classification of the disc fragments in the vertical and horizontal direction. The Combined Task Forces have opted for a classification based on anatomic boundaries frequently used by surgeons.25 In the transverse/axial plane the following zones are used:
Degenerative Disease of The Spine
Introduction
Degenerative Disc Disease
Nomenclature and Classification
Age-related Changes in the Intervertebral Disc
Degenerative Disc Disease
Annular Tears
Disc Heriation
Degenerative Disease of The Spine
Chapter 55