Introduction
The white matter of the central nervous system (CNS) is made up of myelinated neuronal axons. Myelin is a dielectric material composed in large part of lipids; it allows for rapid propagation of nerve impulses and is critical for normal development and functioning of the nervous system. Myelination begins early in the second trimester of fetal development and is largely complete by the end of the second year of postnatal life, although some myelination continues into adolescence. Destruction of myelin, or demyelination, is the pathologic hallmark of several neurologic diseases.
The prototypical demyelinating disease is multiple sclerosis, one of the most common causes of neurologic disability in young adults. Advances in imaging, particularly magnetic resonance imaging (MRI), have allowed radiologists to play an increasing role in both the initial diagnosis and treatment monitoring of patients with this disease. Other demyelinating diseases, including acute disseminated encephalomyelitis and progressive multifocal leukoencephalopathy, are seen in association with infections and immunologic phenomena. MRI plays an important role in diagnosing these diseases and distinguishing them from other conditions.
The disease entities in this chapter are broadly grouped by etiology. In addition to the demyelinating diseases mentioned above, this chapter also covers several other white matter diseases, or leukoencephalopathies. These diverse pathologic processes have different causes but share in common their propensity to cause white matter abnormalities often visible on diagnostic imaging studies. A basic understanding of their imaging characteristics, when combined with a thorough clinical workup, will facilitate accurate diagnosis and appropriate management.
Prior to any discussion of imaging of white matter diseases, an important caveat must be given: not all computed tomography (CT) hypodensities and T2/FLAIR (fluid-attenuated inversion recovery) hyperintense foci in the white matter indicate demyelinating disease. White matter signal changes on MRI are very common in the elderly and increase in prevalence with age. These so-called unspecific bright objects (UBOs) are not without clinical relevance in elderly patients; they have been associated with an increased risk of cognitive decline, dementia, and stroke. Other causes of T2-hyperintense white matter lesions include migraines and sequelae of cerebrovascular disease.
Multiple Sclerosis
Multiple sclerosis (MS) is the most common demyelinating disease of the CNS. MS usually presents between the ages of 20 and 50 and is three times more common in women than in men. The hallmark of the disease is multiplicity in time and space. In most cases, patients present with a subacute clinically isolated syndrome; common presentations include optic neuritis, motor and sensory deficits, transverse myelitis, and brainstem syndromes. The McDonald criteria, revised in 2010, allow for diagnosis of MS based on various clinical and paraclinical assessments, including MRI. Several MS subtypes (clinical phenotypes) have been defined on the basis of their clinical course; these definitions were most recently revised in 2013 and play an important role in disease prognostication and design of clinical trials.
The pathophysiology of MS is complex and not fully understood but is likely autoimmune in nature. The main pathologic characteristic of the disease is the demyelinated plaque, a lesion induced by a variety of immune mechanisms. Plaques are responsible for the characteristic hyperintense white matter abnormalities visible on conventional fluid-sensitive MR sequences. In addition, more advanced MR techniques have permitted detection of other abnormalities in the so-called normal-appearing white matter (NAWM) and gray matter that also occur in MS.
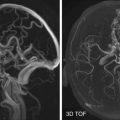
MRI is the imaging method of choice in the diagnosis and monitoring of MS, owing to its high sensitivity and specificity as well as its ability to detect or exclude possible alternative conditions. CT is limited in use where MRI is available. The MRI criteria integrated into the McDonald criteria have demonstrated a high specificity for subsequent development of MS in patients who present with a clinically isolated syndrome suggestive of MS. In such patients the MRI protocol should always include T2-weighted and FLAIR sequences, preferably with three-dimensional (3D)-Fourier transform (volumetric) to minimize partial volume averaging in the commonly small lesions.
MS lesions are seen in characteristic locations: where the white matter contacts the cerebrospinal fluid (CSF). Periventricular, optic nerve, spinal cord, and superficial brainstem lesions are typical, including the cerebellar peduncles, near the trigeminal root entry zone, the tectum, and fourth ventricular floor. Corpus callosum lesions are also characteristic and are much more common in MS than in other white matter diseases.
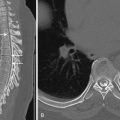
MS lesions have a characteristic size and shape. On T2-weighted and FLAIR images, demyelinating plaques in the brain appear as high-intensity lesions that are often 10 to 15 mm in size and ovoid, although this shape disappears in more advanced cases when lesions become confluent ( Fig. 19-1 ). Periventricular lesions tend to be oriented with their major axis perpendicular to the ependymal surface, referred to as Dawson’s fingers ( Fig. 19-2 ). Periventricular and juxtacortical lesions are better delineated on FLAIR images.


T1-weighted images are generally less sensitive for detection of plaques, but a subset of T2-hyperintense lesions appear dark on T1 images. These “black holes” have signal characteristics ranging from mildly to severely hypointense; the degree of hypointensity correlates with the degree of pathologic severity. When persistent, these lesions are associated with demyelination and axonal loss and have been used in clinical trials as markers of accumulated disease burden. Degree of T1-hypointensity is also influenced by scanning technique ( Fig. 19-3 ).

In addition, lesion enhancement is considered an excellent surrogate for disease activity after a study revealed contrast enhancement was associated with active inflammation in 40 of 40 pathologically proven cases. Triple-dose (0.3 mmol/kg) delayed imaging (20-40 minutes) has shown an increase of more than two times the enhancing lesion detection rate ( Fig. 19-4 ) but is not standard, given concerns about nephrogenic systemic fibrosis.

Enhancement of lesions may be homogeneous or ringlike. A differential feature from ring lesions of many other etiologies is the margin of enhancement coinciding with the margin of FLAIR signal rather than extending significantly beyond the enhancing border ( Fig. 19-5 ).

Most lesions are up to 1.5 cm in diameter, but in rare cases larger ring-enhancing lesions may be seen with obvious mass effect (tumefactive demyelination) ( Fig. 19-6 ). A characteristic feature is an open-ring appearance thought to represent a front of demyelination. In tumefactive cases, perfusion imaging can be of value because ring-enhancing malignant neoplasms typically display elevation of relative cerebral blood volume (rCBV) and rCBV ratio, whereas demyelination does not ( Fig. 19-7 ).


The “life cycle” of an MS lesion typically includes a short enhancing phase, the majority enhancing for no more than 8 weeks. Oftentimes the enhancement of each lesion appears independent of the others ( Fig. 19-8 ).

With the development of immunomodulatory treatment, MRI is periodically used (e.g., annually) even in clinically stable patients to monitor therapeutic efficacy. Contrast enhancement or interim development of new nonenhancing FLAIR lesions are considered by many to indicate failure to arrest disease.
Although MS is the epitome of white matter disease, more recently developed sequences (including volumetric T1, FLAIR, and double-inversion recovery) have revealed significant gray matter involvement.
In addition to the characteristic relapsing-remitting clinical pattern, MS can also be a progressive diffuse degenerative disease. This is manifest as cerebral atrophy and abnormalities in NAWM. Magnetization transfer contrast and diffusion tensor imaging (DTI) have shown measurable differences in the white matter of MS vs. healthy controls that were imperceptible to visual inspection. Functional (f)MRI has also been used to study connectivity abnormalities associated with cognitive dysfunction.
Viral and Postviral Demyelinating Syndromes
Acute Disseminated Encephalomyelitis
Acute disseminated encephalomyelitis (ADEM) is a demyelinating disease of the CNS that commonly follows a febrile illness such as an upper respiratory infection. Numerous infectious agents—predominantly viruses but also several bacterial species—have been reported in association with ADEM. Less commonly the disease may occur following a vaccination. Children with ADEM commonly present with nonspecific symptoms such as fever, headache, and lethargy; adults are more likely to have motor and sensory deficits, as might be seen with an acute episode of MS.
Though they can present in similar fashion, distinction between ADEM and MS is critical because of different prognostic and therapeutic implications for the patient. ADEM is more common in children and, unlike MS, is typically monophasic rather than relapsing. There are also underlying pathologic differences: though the lesions of both MS and ADEM are due to immune-mediated inflammation and demyelination, in ADEM the demyelination remains restricted to the perivascular area, unlike the confluent demyelination observed in MS.
MRI is generally considered the most valuable diagnostic tool in the workup of suspected ADEM. T2-weighted and FLAIR images demonstrate multiple asymmetric hyperintense white matter lesions, particularly in the subcortical regions ( Fig. 19-9 ). Periventricular and corpus callosum lesions are less common than in MS. Enhancement of lesions on postcontrast images is variable; larger lesions may show peripheral or focal irregular central enhancement. Spinal cord lesions can also be seen but are uncommon.

Given the overlap in MRI appearance between the two conditions, it is not always possible to distinguish ADEM from MS on a single MRI examination. For this reason, follow-up scans with an interval of at least 6 months are very helpful; lesions that resolve after corticosteroid therapy or remain unchanged suggest ADEM, but new lesions raise concern for MS.
Progressive Multifocal Leukoencephalopathy
Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease that results from an opportunistic infection of oligodendrocytes by a type of human polyomavirus called the JC virus. The disease occurs in the setting of immunosuppression; although first described in patients with Hodgkin’s disease and chronic lymphocytic leukemia, it has been most frequently associated with human immunodeficiency virus (HIV) infection. PML can also be seen in the context of biologic and immunomodulating therapies, such as natalizumab for MS. Patients usually present with insidious onset of neurologic deficits that may affect motor function, speech, vision, personality, and cognition.
MRI findings in PML include multiple hyperintense foci in the subcortical white matter on T2-weighted and FLAIR images. These lesions are frequently bilateral and characteristically involve the subcortical U fibers ( Fig. 19-10 ). The parietal, occipital, and frontal lobes are commonly affected; other common sites include the posterior fossa and the deep gray matter nuclei.

Other MRI features of PML allow distinction from other neurologic complications of the immunosuppressed state, including cerebral abscess, toxoplasmosis, and primary CNS lymphoma. PML lesions do not demonstrate mass effect or associated edema, differentiating them from these other conditions. Additionally, contrast enhancement is usually absent in PML lesions, unlike the ringlike enhancement commonly seen in cerebral abscesses or toxoplasmosis.
Special note should be made of an entity known as immune reconstitution inflammatory syndrome (IRIS or PML-IRIS), commonly observed in HIV-positive patients with PML undergoing combination antiretroviral therapy. This condition is due to a reconstituted immunity, allowing infiltration of lymphocytes into PML lesions, with corresponding CNS inflammation. In cases of PML-IRIS, PML lesions may demonstrate mass effect and gadolinium (Gd) enhancement ( Fig. 19-11 ).

HIV Leukoencephalitis
CNS manifestations of HIV infection include those related to primary HIV infection, those related to opportunistic infections, and those that result from neoplastic or vascular complications. We will focus here on the effects of primary HIV infection.
Neuroimaging findings in HIV patients may be completely normal. In patients with findings of HIV encephalitis, early MRI findings include symmetric multifocal T2-hyperintense lesions in the periventricular white matter and centrum semiovale, which generally spare the subcortical U fibers. Chronic HIV infection results in progression of these changes, with the initially patchy T2-hyperintense lesions becoming more confluent and extensive, sometimes extending to involve the basal ganglia, cortex, cerebellum, brainstem, and spine. The white matter lesions are typically slightly hypointense on T1 images and usually do not enhance. Another prominent feature of chronic HIV infection is progressive cerebral atrophy ( Fig. 19-12 ).

Toxic and Traumatic Leukoencephalopathies
Pathologic alteration of the cerebral white matter can be caused by exposure to a variety of agents, such as cranial irradiation, chemotherapeutic agents (including antineoplastic and immunosuppressive drugs), drugs of abuse, environmental toxins, and physical trauma. Clinical findings are highly variable; however, patients often present with neurobehavioral deficits ranging from inattention, forgetfulness, and personality changes to severe neurologic dysfunction, which can be easily confused with other white matter diseases.
Radiation-Induced Demyelination
Radiation injury to the brain is commonly seen as a complication of therapeutic radiation therapy for intracranial disease (most commonly primary and metastatic brain tumors, but also arteriovenous malformations) and head and neck neoplasms. It takes two forms: focal injury/radiation necrosis and diffuse white matter injury, also known as diffuse radiation-induced leukoencephalopathy.
Radiation Necrosis
Radiation necrosis (RN) is severe local tissue reaction to high-dose focal radiation therapy and is usually seen at the site of maximum radiation dose—in and around the tumor bed. The reported incidence is 3% to 24%, which increases steeply if doses exceed 65 Gy. RN is most commonly seen 3 to 12 months following radiotherapy, with 70% of cases occurring during first 2 years, but can rarely develop even decades later.
CT findings are nonspecific: RN typically appears as a focal hypodensity with mass effect and variable contrast enhancement. MRI is more sensitive and specific than CT in evaluating RN, demonstrating T2-weighted and FLAIR hyperintensity with or without irregular contrast enhancement. Differentiation between recurrent neoplasm and RN is a frequent diagnostic dilemma because they share imaging characteristics, including origin at or close to the original tumor site, contrast enhancement, interval growth, and surrounding mass effect. Certain diagnostic clues that favor RN have been described, such as a “soap bubble” or “Swiss cheese–like” pattern of enhancement and periventricular location of the lesion. Conversely, corpus callosum involvement, in conjunction with multiple enhancing lesions with or without extension across the midline and subependymal spread, suggests tumor progression.
In many cases, however, the distinction can still not be made with conventional imaging, owing to the coexistence of tumor and RN. In such cases, advanced imaging techniques like MR perfusion imaging (rCBV, vascular transfer constant [K trans ]), MR spectroscopy (choline [Cho], creatine [Cr], and N -acetylaspartate [NAA]), and positron emission tomography (PET) may be helpful ( Fig. 19-13 ). Restricted diffusion, elevated rCBV and K trans values, high Cho/Cr and Cho/NAA ratios, and high PET uptake are more frequently seen in recurrent tumor than in radiation necrosis.