Imaging Options and Protocols
Computed tomography (CT) and magnetic resonance imaging (MRI) are the primary imaging modalities for assessment of the paranasal sinuses. Both these imaging techniques are far superior to plain radiographs in the evaluation of the sinonasal cavities. Plain radiographs of the paranasal sinuses are limited in their ability to delineate the complex bony anatomy or to characterize sinonasal disease and hence are almost obsolete today. They also suffer from high false-negative results.
CT
CT scan is the primary imaging modality for evaluation of sinonasal disease. The concept of screening sinus CT (SSCT) performed in the coronal plane with single window settings, 3-mm sections, and without administration of contrast was promoted in the early 1990s when functional endoscopic sinus surgery (FESS) became popular among endoscopic surgeons. With the evolution of CT scanners to multidetector (MD) CT technology, direct coronal acquisition is no longer commonly performed. Today sinus CT is performed in the axial plane with the patient supine on the scanning table and neutral position of the gantry using 0.625-mm collimation. The volumetric dataset is then reconstructed in coronal, axial, and sagittal planes to provide up to 0.9-mm-thick images in bone (width 3500, center 500) and soft tissue (width 270, center 70) algorithms. When a contrast CT is required, 3- to 4-mm-thick slices are generated in soft tissue algorithm.
MRI
MRI of the paranasal sinuses is performed using a head and neck coil. The protocol includes nonenhanced high-resolution 3- to 4-mm T1- and T2-weighted images, diffusion-weighted imaging (DWI), and contrast-enhanced T1-weighted images with fat suppression. Axial and coronal planes are preferred, and sagittal sequences may be performed when required. Care must be taken to include the adjacent orbits and intracranial cavity along with the sinuses.
Anatomy
Nose, Nasal Cavity, and Lateral Nasal Wall
The nose implies the external nose that projects anteriorly from the face. It consists of a bony portion superiorly and a cartilaginous portion inferiorly. The anatomic subunits of the nose include the nasal root, dorsum, side walls, and nasal septum. The nasal septum is the midline partition that separates the right and left side of the nose and is made up of the septal (quadrangular) cartilage anteriorly, the perpendicular plate of the ethmoid bone posterosuperiorly, and the vomer posteroinferiorly. The external nose leads posteriorly into the nasal cavity, which in turn leads posteriorly into the nasopharynx.
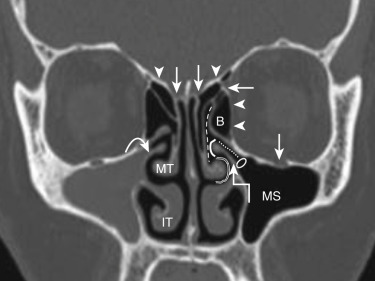
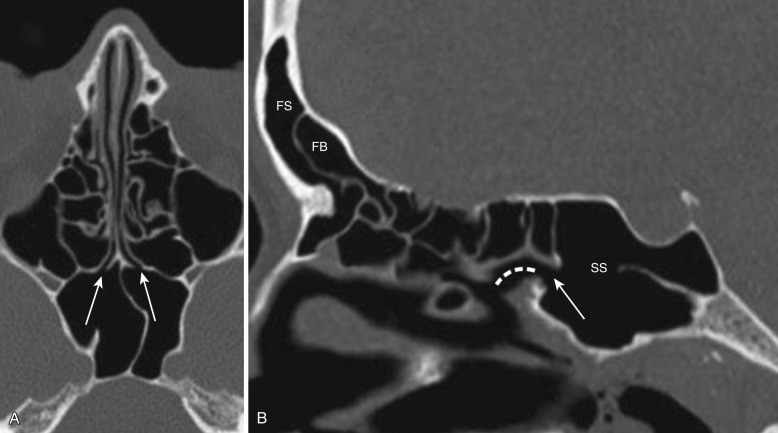
The lateral wall of the nasal cavity shows three (sometimes four) constant projections—the superior, middle, and inferior turbinates—that divide the lateral nasal wall into three meati lateral to the turbinates—the superior, middle, and inferior meati, respectively. A fourth turbinate (supreme turbinate) may be present, and the supreme meatus is the space above the superior turbinate and lateral to the supreme turbinate. The turbinates and meati are best seen on coronal CT sections ( Fig. 23-1 ). The middle turbinate and meatus form the most important anatomic area in the lateral wall of the nose. The attachments of the middle turbinate have anatomic and surgical relevance and provide fairly good stability to the turbinate. Anteriorly the turbinate runs in the sagittal plane and attaches superiorly to the cribriform plate (see Fig. 23-1 ). As it continues behind, it turns laterally into the coronal plane and attaches to the lamina papyracea to form the basal lamella that divides the ethmoid cells into the anterior and posterior ethmoid cells. The middle meatus contains the drainage pathways of the anterior ethmoid air cells, the maxillary and frontal sinuses (osteomeatal unit [OMU]). This region is most commonly involved in the pathophysiology of chronic rhinosinusitis and will be described in greater detail in the following sections.
Paranasal Sinuses
There are four paired paranasal sinuses, one on either side of the midline. They develop from ridges in the lateral nasal wall by the eighth week of embryogenesis and continue pneumatization until early adulthood. Each sinus is named after the bone in which it is located. The relevant imaging anatomy is described in the following sections.
Maxillary Sinus.
Each maxillary sinus is located within the maxillary bone and is the largest and most constant paranasal sinus. It is present at birth and shows a bimodal growth pattern between ages 1 and 3 and 7 and 18 years. The roof of the sinus is formed by the floor of the orbit and has a canal for the second branch of fifth cranial nerve (see Fig. 23-1 ). The medial wall is formed by portions of the ethmoid, palatine, and lacrimal bones. A fairly large part of the medial wall, however, does not contain any bone and is formed by connective tissue and sinus mucosa. This membranous area is called the fontanelle and can break down secondary to sinus infection, forming an accessory ostium of the sinus. The accessory ostium is nonfunctional and drains the sinus only when the main ostium is blocked. The primary maxillary sinus ostium is located on the highest part of the medial wall of the maxillary sinus (see Fig. 23-1 ). The floor of the sinus is formed by the alveolar process of the maxilla and palatine bones. The posterolateral wall separates it from the pterygomaxillary fissure medially and infratemporal fossa laterally (see Fig. 23-23A, B, and D ). The maxillary sinus drains through the primary ostium into the ethmoid infundibulum (see Fig. 23-1 ).
Ethmoid Sinus (Ethmoid Air Cells).
Each ethmoid sinus is located within the ethmoid labyrinth and has a honeycomb appearance. It is present at birth and continues to grow until about 12 years of age. The ethmoid labyrinth is situated inferolateral to the olfactory fossa, which is bounded by the horizontal and vertical lamellae of the cribriform plate. The roof of the sinus is formed by the fovea ethmoidales of the frontal bone, which joins the vertical lamella of the cribriform plate (see Fig. 23-1 ). The medial wall is formed by the lateral surface of the middle and superior turbinate, the lateral wall by the lamina papyracea (see Fig. 23-1 ), and the posterior wall by the anterior wall of the sphenoid sinus ( Fig. 23-2 ). The ethmoid sinus is divided into multiple discrete cells by bony lamellae that extend laterally to the lamina papyracea and superiorly to the fovea ethmoidales. Of these, the basal lamella divides the ethmoid air cells into anterior and posterior groups of ethmoid cells. The anterior ethmoid air cells drain into the ethmoid infundibulum, and the posterior ethmoid air cells drain into the superior meatus (see Figs. 23-1 and 23-2 ). The pneumatization of the ethmoid air cells shows the highest variation among all the sinuses. There are two primary types of ethmoid air cells: intramural and extramural. Intramural cells remain within the ethmoid bone and include the ethmoid bulla, suprabullar cell, and frontal bullar cell. The extramural cells develop external to the ethmoid labyrinth and include the agger nasi cell, frontal cell, supraorbital ethmoid cell, Haller cell, and Onodi cell. These are considered separately in the section on anatomic variants.
Frontal Sinus.
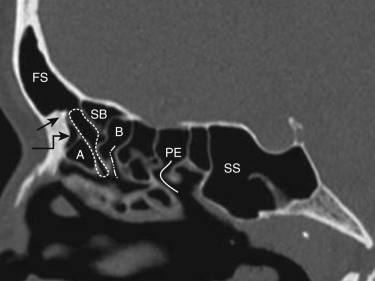
Each frontal sinus lies within the frontal bone. The frontal sinus is rudimentary at birth and begins to grow by age 6, continuing until the late teens. The frontal sinuses on two sides are separated by the interfrontal sinus septum. The anterior wall is the thick anterior table, and the posterior wall is the thinner posterior table that separates the sinus from the cranial cavity. The floor is the anterior roof of the orbit. The frontal sinus drains through the frontal sinus ostium and the frontal recess into the middle meatus (see Fig. 23-2 ).
Sphenoid Sinus.
The sphenoid sinus is located in the body of the sphenoid. It begins to grow at age 3 and is fully pneumatized by about age 18. The sphenoid sinuses on the two sides are separated by the intersphenoid septum. The roof of the sinus is formed by the sellar floor, and the lateral wall demarcates the sinus from the cranial cavity. The carotid artery is situated in the lateral wall, the optic nerve superolateral to the sinus, and the vidian nerve canal in its floor (see Fig. 23-5A ). The sphenoid sinus ostium is located medially in the anterosuperior portion of the sinus and opens into the sphenoethmoid recess ( Fig. 23-3 ).
Drainage Pathways of the Paranasal Sinuses
The paranasal sinuses are broadly divided into two major groups: the anterior sinuses and the posterior sinuses. The anterior sinuses comprise the frontal sinus, anterior ethmoid air cells, and maxillary sinus. These drain into a common area centered in the middle meatus, the osteomeatal unit (OMU). The posterior sinuses are the posterior ethmoid air cells and the sphenoid sinuses. These drain into the sphenoethmoid recess.
Osteomeatal Unit.
The OMU is the common drainage pathway of the anterior sinuses, the key area in the pathophysiology of chronic sinusitis and the center of interest since the advent of FESS. It is a narrow anatomic region bounded by the middle turbinate medially, the lamina papyracea laterally, and the basal lamella posteriorly. This region and all its components are best visualized on coronal CT sections (see Fig. 23-1 ). The OMU comprises the uncinate process, hiatus semilunaris, ethmoid infundibulum, and the ethmoid bulla (bulla ethmoidales).
The uncinate process is a key component of the osteomeatal unit and a very important surgical landmark for endoscopic sinus surgery. It is a hook-shaped bone that arises from the posteromedial wall of the nasolacrimal duct and is best seen on coronal CT sections as the superior extension of the medial wall of the maxillary sinus (see Fig. 23-1 ). The maxillary sinus ostium is located behind the uncinate process.
The hiatus semilunaris is a crescent-shaped cleft located just posterior and superior to the uncinate process and anteroinferior to the ethmoid infundibulum (see Fig. 23-1 ). It serves as the communication of the ethmoid infundibulum with the middle meatus.
The ethmoid infundibulum receives drainage from the ethmoid bulla in its anterior portion and the maxillary sinus ostium in its floor. It opens into the hiatus semilunaris and is located inferomedial to the ethmoid bulla and superolateral to the uncinate process (see Fig. 23-1 ).
The ethmoid bulla is the largest and most constant of the anterior ethmoid air cells. It receives drainage from the anterior ethmoid air cells and drains into the ethmoid infundibulum. There may be variation in the amount of pneumatization of the ethmoid bulla. If it is not pneumatized, it is termed torus ethmoidales; excessive pneumatization may form a giant bulla that may fill the entire middle meatus. The ethmoid bulla is located just posterior and superior to the hiatus semilunaris and posterior to the frontal recess. The lateral wall is formed by the lamina papyracea, the roof by the skull base, and the posterior wall by the basal lamella (see Figs. 23-1 and 23-2 ). Sometimes an air recess may form between the bulla and the basal lamella; this is called a retrobullar recess or sinus lateralis.
Frontal Recess and Frontal Sinus Drainage Pathway.
The frontal sinus drainage pathway (FSDP) comprises the frontal sinus infundibulum, frontal sinus ostium (FSO), and frontal recess (FR). Only the FR is a part of the OMU. The entire anatomy of the FSDP is best seen on coronal and sagittal images. The frontal sinus tapers down to a funnel-shaped inferior portion called the frontal sinus infundibulum. This frontal infundibulum leads to the FSO, which is the narrowest part of the FSDP and located in its most dependent portion in the floor of the sinus at the level of the nasofrontal spine (see Fig. 23-2 ). The frontal infundibulum and the FSO are best visualized on sagittal images. The portion of the FSDP below the ostium is the FR, and this drains into the middle meatus (see Fig. 23-2 ). It measures about 13 mm in anterior-to-posterior dimension and has the shape of an inverted funnel with its tip at the frontal ostium. The FR is surrounded by the ethmoid air cells—the agger nasi cell anteriorly, the ethmoid bulla posteriorly and laterally, and the most anterior and superior portion of the middle turbinate medially (see Figs. 23-1 and 23-2 ).
Sphenoethmoid Recess.
The sphenoid sinus ostium opens into the sphenoethmoid recess (SER). The SER lies just lateral to the posterosuperior nasal septum and behind the tail of the superior turbinate and is best appreciated on sagittal and axial CT images (see Fig. 23-3 ). The posterior ethmoid air cells drain into the superior meatus and from there into the SER (see Fig. 23-2 ).
Important Anatomic Variations and Their Relevance
Numerous variations in the sinonasal anatomy have been described. Many of them have important clinical and surgical relevance, and it is very important to identify them on the presurgical scans obtained in such patients. MDCT with its multiplanar reformations provides the best details of the complex bony anatomy and anatomic variants of the sinonasal cavities. It is extremely important to review the CT images in all three planes for better understanding of the anatomy and identification of these anatomic variations. If available, review of images on a workstation is extremely beneficial for reporting the scans.
Frontal Recess Cells
These cells are variations in the pneumatization of the anterior ethmoid air cells. They are broadly divided into the anterior and posterior groups of frontal recess cells. The anterior group is located anterior to the frontal recess and comprises the agger nasi cells and the frontal cells. The posterior frontal cells are located posterior to the frontal recess and include the supraorbital cells, frontal bullar cells, and suprabullar cells; they are bordered posteriorly or superiorly by the base of the skull. These cells may obstruct frontal sinus drainage at the level of the frontal recess and contribute to the development of frontal sinusitis. Also, if these cells are not addressed during endoscopic surgery on the frontal recess, they often lead to surgical failure and recurrence of the disease process. Therefore it is very important for the radiologist to identify them and comment on their presence using the standard nomenclature as described below.
Agger Nasi Cell.
The agger nasi cell (ANC) is a fairly constant anteriormost ethmoid cell seen in up to 98% patients at CT. It is located anterior to the vertical attachment of the middle turbinate and is best visualized on sagittal and coronal CT sections ( Fig. 23-4 ; also see Fig. 23-2 ). The degree of pneumatization of the ANC varies and has a bearing on the size of the frontal sinus ostium and frontal recess.
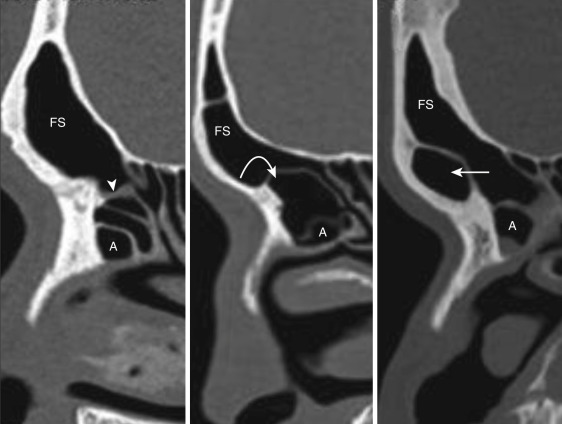
Frontal Cells (Kuhn’s Cells).
Four types of frontal cells are described. Types 1 to 3 frontal cells are commoner and located directly above the ANC. The type I cell is a single anterior ethmoid air cell seen above the ANC (see Fig. 23-2 ). Type II cells are two or more anterior ethmoid air cells above the ANC (see Fig. 23-3 ). The type III cell is a single large cell above the ANC that bulges into the frontal sinus. The type IV cell is an isolated air cell located completely within the frontal sinus, simulating a “cell within a cell” appearance; it is visualized infrequently (see Fig. 23-3 ).
Supraorbital Ethmoid Cell.
This cell represents pneumatization of the orbital plate of the frontal bone posterior to the frontal recess and the frontal sinus. It simulates the appearance of septate or hyperpneumatized frontal sinuses on coronal images, and axial images confirm their location posterior and lateral to the frontal sinus (see Fig. 23-14 ).
Frontal Bullar Cell and Suprabullar Cell.
The ethmoid bulla forms the posterior boundary of the frontal recess. The frontal bullar cell, if present, lies above the ethmoid bulla and posterior to the frontal sinus and frontal recess. It extends into the frontal sinus and is best seen on sagittal images (see Fig. 23-3B ). When the cell lies below the level of the frontal sinus ostium and does not extend into the frontal sinus, it is called a suprabullar cell (see Fig. 23-2 ).
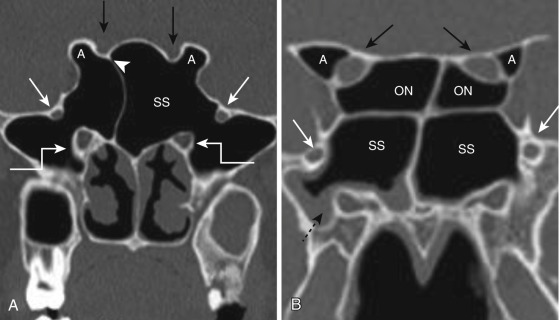
Onodi Cell (Sphenoethmoid Cell)
The Onodi cell is an anatomic variation of the most posterior ethmoid air cell when it extends into the sphenoid bone, superior or superolateral to the sphenoid sinus, pushing the sphenoid sinus inferiorly. The cell is intimately related to the optic nerve canal and can be mistaken for sphenoid sinus at endoscopy, increasing the risk of orbital complications. Hence it is of paramount importance to report their presence at CT examinations. Identification of this cell requires careful review of coronal, axial, and parasagittal CT images. Presence of a horizontal septum dividing the sphenoid sinuses into “two floors” or giving a cruciform appearance on coronal CT images suggests the presence of Onodi cells ( Fig. 23-5 ).
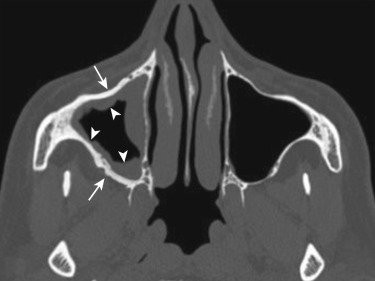
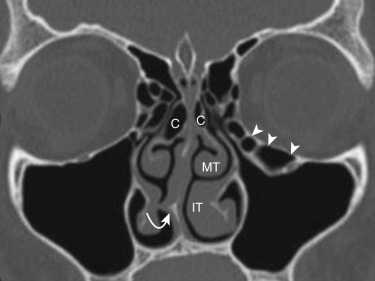
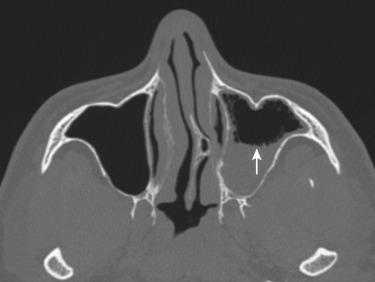
Haller Cell (Orbitomaxillary Or Infraorbital Ethmoid Cell)
This is an extramural anterior ethmoid cell that pneumatizes inferior to the orbital floor, extending from the ethmoid labyrinth below the ethmoid bulla toward the interior of the maxillary sinus ( Fig. 23-6 ). Although debate exists on whether or not their presence contributes to the occurrence of sinusitis, most agree that it is their number and size that influence the development of inflammatory sinus disease.
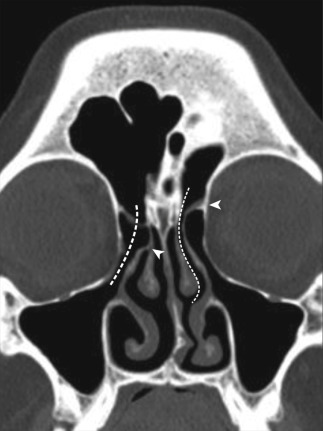
Uncinate Process Variations
Three types of uncinate processes have been described, depending on the superior attachment that impacts the drainage of the frontal sinus. Type I uncinate process is the commonest type and attaches to the lamina papyracea, separating the ethmoidal infundibulum and the frontal recess ( Fig. 23-7 ). Type II uncinate attaches to the skull base, and type III turns medially and attaches to the middle turbinate (see Fig. 23-7 ). In type II and III uncinate processes, the frontal recess opens into the ethmoid infundibulum. The uncinate process may also be medialized or lateralized. An uncinate bulla may be seen.
Nasal Septal Variations
The nasal septum may be deviated and make endoscopic access difficult. The deviation may be focal or more of a smooth curvature and is often associated with septal spurs and a concha bullosa or a lamellar concha (see Fig. 23-6 ). A nasal septal air cell may be seen in the posterosuperior portion of the nasal septum and may communicate with the sphenoid sinus.
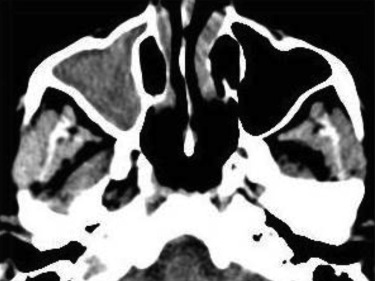
Middle Turbinate Variations
The middle turbinate may be pneumatized. When pneumatization involves the bulbous portion of the middle turbinate, it is termed concha bullosa. If only the attachment portion of the middle turbinate is pneumatized, it is termed lamellar concha (see Fig. 23-6 ). A small concha may not be clinically significant, but a larger one—commonly associated with a nasal septal deviation—may obstruct the ethmoid infundibulum and lead to sinusitis. The convexity of the middle turbinate may be directed laterally and is called paradoxical curvature of the turbinate (see Fig. 23-6 ). A small paradoxical turbinate may not be significant, but a larger one may impair drainage at the OMU.
Variations of the Ethmoid Roof
Kero’s classification describes three types of ethmoid roofs, depending on the depth of the olfactory fossa, determined by measuring the height of the lateral lamella of the cribriform plate. Type I ethmoid roof has a depth of 1 to 3 mm, type II a depth of 4 to 7 mm, and type III a depth of 8 to 16 mm (see Fig. 23-1 ). Type III is associated with more potential damage from iatrogenic injury.
Variations Related to Sphenoid Sinus
Four types of optic nerve canals (OCs) have been described, depending upon the relationship of the OC with the posterior sinuses. Type I OC is the commonest type and runs immediately adjacent to the sphenoid sinus, without indentation of the wall or contact with the posterior ethmoid air cell. Type II OC courses like the type I but indents the sphenoid sinus wall. Type III OC runs through the sphenoid sinus, with at least 50% of the nerve being surrounded by air, and type IV OC lies immediately adjacent to the sphenoid sinus and the posterior ethmoid air cells (see Fig. 23-5 ). Anterior clinoid process pneumatization is associated with type II and type III OCs and predisposes the optic nerve to injury during FESS. The carotid artery canal may form a bulge into the sphenoid sinus wall. Sometimes the sinus wall separating the optic nerve or the carotid artery from the sinus may be dehiscent, or the intersphenoid sinus septum may be attached to the sinus wall covering them, and thus arterial or nerve injury may occur when the septum is avulsed during surgery (see Fig. 23-5A ).
Other Variants
The maxillary sinus may show septations, resulting in inadequate drainage of sinus secretions. An accessory ostium may be present. The importance of this lies in the fact that an antrochoanal polyp may sometimes exit through the accessory ostium rather than the natural ostium. An aerated crista galli may communicate with the frontal recess, causing obstruction of the ostium and leading to chronic sinusitis.
Inflammatory Sinonasal Disease—Sinusitis
Sinusitis means inflammation of the sinus mucosa. Several forms are described based on the duration of symptoms. Acute sinusitis is almost always sudden in onset and may last up to 4 weeks. Subacute sinusitis is a continuation of the acute process and lasts anywhere between 4 and 12 weeks. Chronic sinusitis is defined as sinonasal inflammation that lasts for 12 weeks and beyond. The disease is termed recurrent acute sinusitis when there are more than four episodes of acute sinusitis. Acute sinusitis is most commonly an inflammatory response to an upper respiratory viral infection that causes sinonasal mucosal congestion and edema that may lead to sinus obstruction and bacterial proliferation. Chronic sinusitis develops secondary to acute disease that is refractory to treatment and is generally a sequelae to the interference of the normal mucociliary drainage of the paranasal sinuses.
Imaging is neither routinely recommended nor performed for every patient who presents with sinusitis. The American Academy of Otolaryngology, in its 2007 clinical practice guidelines, recommended against diagnostic imaging for patients with acute or subacute sinusitis unless an intraorbital or intracranial complication is suspected. Imaging is recommended in patients who fail to respond to medical treatment, present with recurrent sinusitis, or have unilateral recurrent symptoms when an alternate diagnosis of neoplasia or fungal infection is suspected.
CT is clearly superior to MRI for delineation of the bony anatomy and anatomic variants. CT shows the presence and extent of the sinonasal disease, nature of the sinonasal secretions, and presence of any intrasinus calcifications. Hence CT is the preferred technique in preoperative evaluation of the paranasal sinuses and the accepted gold standard for delineation of inflammatory sinus disease due to obstruction. Coronal CT images almost simulate the appearance of the sinonasal cavities at endoscopy and are most preferred by endoscopic surgeons. Contrast CT or MRI have a role to play when there is suspicion of an intraorbital or intracranial extension of the disease.
Imaging Findings
Acute Sinusitis.
CT and MRI may show nonspecific mucosal thickening, submucosal edema, air-fluid levels, or sinus secretions interspersed with air bubbles ( Fig. 23-8 ). Acute sinonasal secretions are of a mucoid nature (−10 to 25 HU) and are typically hypointense on T1 and hyperintense on T2 sequences. An isolated air-fluid level as the only finding in the sinus is fairly characteristic for acute sinusitis but may not be seen in all patients. Complications of acute sinusitis include orbital cellulitis, orbital abscess, empyema, meningitis, brain abscess, and superior ophthalmic vein and/or cavernous sinus thrombosis. Although they can be visualized on contrast CT, intracranial complications and assessment of the orbital apex are best done on contrast MRI studies.
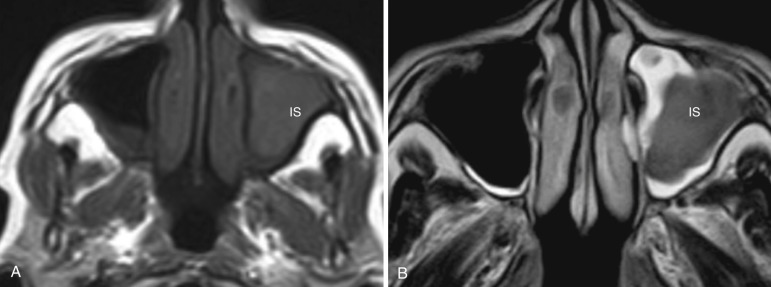
Chronic Sinusitis
Imaging features include nonspecific mucosal thickening, sinus opacification, intrasinus calcifications, and sclerosis (reactive osteitis) of the bony walls of the sinus ( Figs. 23-9 and 23-10 ). Mucosal thickening is common to both acute and chronic forms of sinusitis. Presence of a sclerotic thickened bone is a fairly characteristic feature of chronic sinusitis but may not be seen in all patients. Calcifications are generally more peripheral and scattered. Air-fluid levels may be seen. Whereas secretions in acute sinusitis are watery, chronic secretions vary in their fluid and protein content, thereby affecting their CT and MR appearances. With chronicity, secretions lose water and become more proteinaceous and hence appear denser on CT. A thin hypodense line is usually seen separating the dense sinus secretions from the bony wall and represents thickened mucosa and submucosal edema (see Fig. 23-10 ). Progressive increase in the protein content of the secretions from 5% to about 25% results in an increase in the T1-weighted signal from low to high intensity. With increase in protein content beyond 25% to about 35%, the T2 signal begins to drop ( Fig. 23-11 ). A very high protein content beyond 35% causes loss of almost all water from the secretions and results in a fall of both the T1 and T2 signal intensity, mimicking a signal void. In such cases, sinus disease may be completely missed on MRI, while CT may show the sinus filled with chronic desiccated secretions. Other features of chronic sinusitis include retention cysts, polyps, and mucoceles.