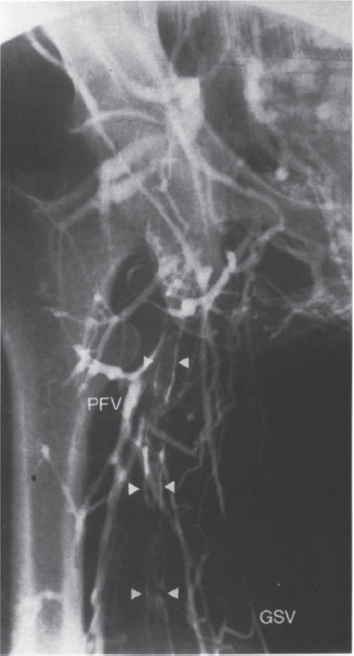
Descending Venography Chronic venous insufficiency is a major cause of morbidity. Patients with this condition too often receive inadequate clinical and diagnostic evaluations and inappropriate therapy. The noninvasive evaluation of the patient with lower-extremity venous insufficiency using color-flow Doppler has been described previously. Other noninvasive techniques include impedance plethysmography, phleborrheography, evaluation by directional Doppler ultrasound, and radionuclide techniques.1 Ascending lower-extremity venography, long considered the “gold standard” for evaluating the patient with venous insufficiency, is used to determine whether acute deep venous thrombosis (DVT) is present (Fig. 42–1) in the clinical setting of chronic venous insufficiency. This study also assists in preoperative planning by “mapping out” the location of varicosities and incompetent communicating veins between the deep and superficial venous systems; however, ascending lower-extremity venography has limitations, including the following: (1) an inability to assess function of venous valves; (2) inadequate filling of lower-extremity veins (both superficial and deep) because of altered hemodynamics; (3) a failure, in general, to image the patient in a more physiologic position (i.e., imaging the patient during contrast injections in the supine or semi-upright position instead of the standing position); (4) possible contrast allergy or contrast-induced nephrotoxicity; and (5) possible contrast-induced chemical phlebitis. Recent advances in surgical techniques used to treat patients with venous insufficiency have prompted a renewed interest in venography. This chapter discusses the anatomy and the hemodynamic evaluation of the patient with lower-extremity venous insufficiency discussed. Included in this chapter is a summary of the technique of descending pelvic and lower-extremity venography. Correlation with noninvasive imaging studies is emphasized. Clinical conditions associated with lower-extremity venous insufficiency include the following: (1) prior deep venous thrombosis, (2) pregnancy, and (3) trauma. Frequently, the patient presents clinically with a sensation of “increased fullness” in the buttocks and extremities, sometimes accompanied by chronic pain. Lower-extremity swelling and prominent varicose veins are found on physical examination. In advanced disease, skin discoloration and ulcers may occur. If contrast studies document valvular incompetence, and if competence of pelvic or thigh vein valves could be restored surgically, the lower-extremity varicosities would theoretically “deflate” without the need for extensive sclerotherapy or venous “stripping” procedures. Because lower-extremity venous insufficiency is common, the goal of the radiologist is to evaluate the patient for a possible surgical correction. Venous Anatomy of the Lower Extremities Prior to a discussion of the technique of descending pelvic venography, a review of lower-extremity venous anatomy is indicated to correlate the radiographic findings identified on ascending lower-extremity and descending pelvis/extremity venography. FIGURE 42–1. Anteroposterior spot film obtained during ascending lower-extremity venography in a man with right lower-extremity swelling. Extensive deep venous thrombosis is identified. Contrast outlines extensive thrombus (arrowheads) in the superficial femoral vein. The greater saphenous vein (GSV) and profunda femoral vein (PFV) tributaries act as collaterals. The common femoral and iliac veins are also occluded in this man with acute DVT. Doppler ultrasound should be used to screen for DVT. If this study is equivocal, then contrast venography should be performed. Derangements of valvular function may explain, in part, the clinical picture seen in patients who have suffered episodes of DVT; however, some of the abnormalities seen in patients with lower-extremity venous stasis changes may result not from previous thrombophlebitis, but rather from the absence of valves. In 1948 the relationship of valvular function to the presence of vein pathology (i.e., varicosities) was set forth by Bauer.2 According to Bauer, DVT was not a causative factor: Absence of valves between the heart and the long saphenous vein predisposes to the development of superficial varicosities, while deficiency or absence of valves in the external iliac and common femoral veins may result in excessive strain on the remaining deep valves. Incompetency or varicosity may develop in the deep venous system of such subjects and may account for the occurrence of deep venous insufficiency in patients giving no history of thrombophlebitis. Thus, valvular dysfunction was recognized as a cause of venous insufficiency. Lower-extremity Venous Valve The inferior vena cava (IVC) lacks valves; however, Friedrich3 (1882), McMurrich4 (1906), and Di Dio5 (1949) reported the occurrence of valves in the common iliac vein. The external iliac, common femoral, long (i.e., greater) saphenous, superficial femoral, profunda femoral, and popliteal veins all contain valves. The distribution of valves in the femoral, external iliac, and common iliac veins was summarized by Basmajian in 1952.6 In this anatomic study, 76 cadaver-paired limbs were dissected. In two of the cadavers, the iliac veins were destroyed, leaving only the femoral veins suitable for study. All cadavers were men with ages ranging from 31 to 94 years. No valves were found in the IVC. The common iliac veins demonstrated valves in 1 to 7%. The external iliac veins above the level of the inguinal ligament demonstrated valves in 24%. Below the inguinal ligament, the common femoral vein was shown to have valves in 67%, and the superficial femoral vein (below the mouth of the profunda femoral vein) demonstrated valves in 90%. The latter location was the most constant site noted for a valve in the femoral vein and occurred in 68 of 76 femoral veins (89.5%), usually bilaterally. The number of valves in the femoral veins between the mouth of the profunda tributary and the hiatus in the adductor magnus was variable. Five veins (6.6%) had five valves, nine veins (11.9%) had four valves, 24 veins (31.7%) had three valves, 23 veins (30.4%) had two valves, 13 veins (17.2%) had one valve, and two veins (2.6%) had no valves. No definite pattern of bilateral symmetry in valve position or number was seen.6 In a similar study by Powell and Linn7 in 1951, 27 cadaveric subjects dissected at postmortem examination ranged in age from stillborn fetuses to adults aged 84 years. Valves were present in the external iliac vein in 33% of limbs, the common femoral vein in 72%, the superficial femoral vein in 100%, and the upper third of the popliteal vein in 96%. One valve was found in each of the external iliac veins, except for two limbs in which this vessel contained two valves. A single valve was found in the common femoral vein. The superficial femoral vein contained between one and four valves (one in 10%, two in 33%, three or more in 57%). Just above the level of the knee joint, the popliteal vein contained a single valve at its upper end. No difference was seen in the number of valves present in the two sexes and no difference in the number of valves with age. In the upright position, the estimated volume of blood in the venous system of one lower-extremity is about 330 mL.8 Low-pressure gradients characterize flow within the venous system, especially in the supine position. The small positive pressure gradient of a recumbent patient between the venules in the periphery and the right atrium is only a fraction of the hydrostatic pressure difference present in the lower-extremity of an upright patient.9 During exercise, muscular contraction of the calf forcibly compresses the veins within this compartment of the leg. The valves of the venous system force blood to flow in a proximal direction. Venous pressures of up to 100 mm Hg are created by this mechanism.10 This repetitive “pumping action” aids in venous return and also reduces the pressure within the deep veins so that flow occurs from the superficial to the deep system.11 The deep paired veins of the lower-limbs are embedded in thick calf muscles and surrounded by the strong crural fascia.9 During walking, the pumping action of the so-called venous heart decreases the venous system pressure to approximately 30 to 40% of the normal 100 to 120 mm Hg upright venous pressure. The pressure level depends, to a great extent, on the competency of the venous valves in the deep, superficial, and communicating veins.12 The postthrombotic state is a sequela of DVT. The following, in order of frequency, are clinically observed in the patient with the postthrombotic syndrome (PTS): edema, pain, pigmentation changes, varicose veins, stasis dermatitis, stasis cellulitis, and chronic ulceration.12 The patient with PTS has the same standing venous pressure as the patient with a normal extremity or the patient with simple varicose veins. In PTS, however, the pressure remains unchanged during walking. Thus, persistent ambulatory venous hypertension (AVH) is found in the PTS patient and, to a lesser degree, in the patient with simple varicose veins. The sequelae of DVT are believed to arise because of the constant AVH secondary to recanalization and resultant valvular incompetence in the deep, communicating, and superficial veins of the lower-extremity, not because of deep venous system occlusion, as is so commonly believed.12

 Etiology of Venous Insufficiency
Etiology of Venous Insufficiency
 Normal Anatomy
Normal Anatomy
 Lower-extremity Venous Pressures and Physiology: Normal and Pathologic
Lower-extremity Venous Pressures and Physiology: Normal and Pathologic
 Postthrombotic Venous Disease
Postthrombotic Venous Disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree