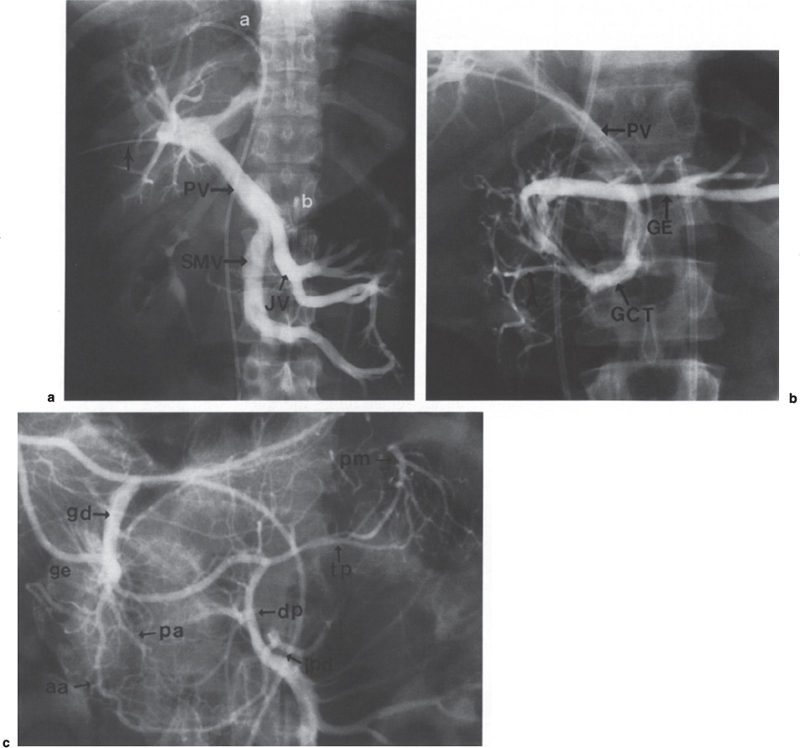
Portal Vein Sampling Islet cell tumors usually occur in the pancreas and duodenum and rarely in other sites. Most occur in adults, although they have been reported in children. Islet cell tumors may be nonfunctioning clinically or functioning with various clinical manifestations, depending on the types of hormones produced. Because of the lack of symptoms related to hormones, the nonfunctioning islet tumors, when found, are usually large. In contrast, the functioning islet tumors tend to be small, and even an occult tumor can produce symptoms. Preoperative localization studies have been used to help intraoperative localization of islet cell tumors.1–5 Several imaging techniques have been used for the localization of the islet cell tumors. These include ultrasound, computed tomography (CT), magnetic resonance (MR) imaging, somatostatin scintigraphy, endoscopic ultrasound, and intraoperative ultrasound.6–16 Although intraoperative ultrasound has been reported to be useful in localizing islet cell adenomas, most surgeons rely on a meticulous surgical exploration and palpation of the pancreas. Despite technical advances in these imaging techniques, small islet cell adenomas may remain occult. Angiography remains a useful method in localizing islet cell adenomas, with an overall success rate of 60% for insulinomas.17–19 Angiography has been much less sensitive in localizing gastrinomas because they tend to be avascular and small. Some islet cell tumors may not be even palpable at surgery because of the small size and texture that simulates the normal pancreatic tissue. Therefore, surgeons have been influenced to perform extensive dissection and distal pancreatectomy.20–21 In such circumstances, occult tumors in the head of the pancreas can be missed, and subsequent repeat exploration results in increased morbidity and mortality.19 The reported complications of surgery for insulinomas have included pancreatic fistulas, pancreatitis, sepsis, bleeding, and pneumonia. The reported mortality rate is 1.6% after primary operations, increasing to 5.7% following reoperations. Localization of such occult islet cell tumors can be achieved by measuring hormone levels in the pancreatic venous effluent using transhepatic portal vein catheterization and sampling. This transhepatic portal venous sampling (THVS), first described by Ingemansson et al in 1975,22 has proven to be a useful diagnostic procedure for localizing occult islet cell adenomas as well as the multiple sources of excessive hormone production from microadenomatosis, islet cell hyperplasia, nesiodioblastosis, and hepatic metastases.1,3,4,6,19,23–30 This chapter reviews the role of THVS and the vascular anatomy and describes the new techniques of angiographic localization that combine intraarterial stimulation and hepatic vein sampling with hormone assay. Depending on the types of hormones produced, functioning islet cell tumors can be classified as insulinoma, gastrinoma, vasoactive intestinal polypeptide tumor (VIPoma) glucagonoma, somatostatinoma, and pancreatic polypeptideoma (Table 45–1). Insulinomas are the most common functioning islet cell tumors, accounting for 50 to 60% of all pancreatic endocrine tumors.25 They occur in all age groups; about 75% are solitary and benign; about 10% are malignant. About 15% represent multifocal pancreatic disease, such as adenomatosis, nesidioblastosis, and islet cell hyperplasia. The diagnosis of insulinomas is made by a 72-hour fast with simultaneous measurement of blood glucose and insulin levels. Serum levels of C-peptide and antiinsulin antibodies are measured to exclude factitious hypoglycemia. Islet Cell Tumor Hormone Symptoms Insulinoma Insulin Fasting hypoglycemia Gastrinoma Gastrin Zollinger-Ellison syndrome VIPoma VIP WDHA syndrome Glucagonoma Glucagon Glucagonoma syndrome Somatostatinoma* Somatostatin Diabetes, diarrhea, steatorrhea Pancreatic polypeptideoma Pancreatic polypeptide Clinically silent VIP, vasoactive intestinal polypeptide; WDHA, watery diarrhea, hypokalemia, achlorhydria. *Glucagonoma syndrome, diabetes, diarrhea, dermatitis, deep venous thrombosis. The Zollinger-Ellison syndrome (ZES) occurs in sporadic form or in association with multiple endocrine neoplasia type 1 (MEN-1) syndrome. Sporadic gastrinomas may occur in the pancreas or extrapancreatically in the duodenum, hepatoduodenal ligament, and peripancreatic tissue or lymph node. The diagnostic features include peptic ulcer disease, gastric acid hypersecretion, and elevated serum gastrin. A review of 25 patients with ZES diagnosed at the University of Michigan Medical Center showed that 76% of the cases were sporadic (89% with malignant disease) and 24% were associated with MEN-1 (66% with malignant disease).31 Tumors were found in the duodenum-in 48% and in the pancreas in 20%, and in 32% of cases, tumors were found in the peripancreatic and paraduodenal lymph nodes and liver, without known primaries. Understanding the vascular anatomy and its variations is important in the performance of angiography and venous sampling for localization of islet cell tumors. The branches of the celiac, splenic, hepatic, gastroduodenal, and superior mesenteric arteries supply the pancreas. The dorsal pancreatic (DP) artery may originate from the celiac, hepatic, splenic or superior mesenteric artery, supplying the entire pancreas. The branches of the DP are the transverse pancreatic artery (communicating with the pancreatica magna and caudal pancreatic arteries) and uncinate and anastomosing branches (anastomosing with pancreatic arcade arteries of the gastroduodenal and superior mesenteric arteries). The pancreatica magna artery (arising from the proximal splenic artery) and the caudal pancreatic artery (arising from the distal splenic artery) supply the body and tail portions of the pancreas. The pancreatic arcade arteries of the gastroduodenal artery anastomose with the inferior pancreaticoduodenal artery of the superior mesenteric artery, supplying the head and uncinate process of the pancreas. If the celiac or superior mesenteric artery is stenotic or occluded, collateral circulation develops through the pancreatic arteries. The arterial supply to the extrahepatic bile duct and hepatoduodenal ligament comes from the branches of the gastroduodenal, hepatic, or superior mesenteric artery. The portal vein returns blood from the pancreas, spleen, and gastrointestinal tract. It is formed behind the pancreas by the union of the splenic and superior mesenteric veins and courses toward the porta hepatis, posterior and to the right of the hepatic artery. Its tributaries are the coronary, posterior arcade, peribiliary, cystic, and right gastric veins. The splenic vein returns the blood from the spleen, stomach, colon, and the tail and body of the pancreas. Its tributaries are the gastric, pancreatic, transverse, and inferior mesenteric veins. The superior mesenteric vein returns the blood from the head of the pancreas, duodenum, small bowel, and colon. Its tributaries are the gastrocolic, right colic, middle colic, jejunal, and ileal veins. The tributaries of the gastrocolic trunk are the anterior superior pancreaticoduodenal, anterior inferior pancreaticoduodenal, right gastroepiploic, and colic veins (Fig. 45–1). The transfemoral arterial approach is used to examine the pancreas and liver, to obtain arterial blood samples during portal venous sampling, and to inject secretin or calcium into the pancreatic arteries. The transfemoral venous approach is used to catheterize the hepatic vein for hepatic vein sampling using a 5F Cobra catheter. The procedure can be performed as an outpatient procedure. The patient can be sent home with an adult after 4 hours of observation. The preangiographic preparation of the patient is the same as that for the standard arterial catheterization: limiting oral intake to clear liquids 8 hours before the procedure, checking serum creatinine, and evaluating coagulation parameters. Before the angiographic examination, the procedure should be explained in detail to the patient, including the potential diagnostic benefits, any alternate diagnostic or therapeutic procedures, and potential complications. A sedative (midazolam) and an analgesic (fentanyl) commonly are given immediately before and during the examination. The patient should be monitored continuously for respiratory and cardiac function with pulse oximetry, electrocardiography (EGG), and blood pressure measurement. After preparation of the groin using Betadine, the puncture site is anesthetized with 2% lidocaine. After a small skin nick using a no. 11 scalpel blade, the artery is punctured using a 19- or 21-gauge single-wall puncture needle. When the 21-gauge needle is used, an 0.018-inch guidewire is introduced, and the needle is withdrawn. Then a 4F coaxial dilator is used to advance a standard 0.035-inch guidewire into the aorta. A 4F-or 5F curved tip catheter, such as a Cobra catheter or a Shepherd’s hook catheter, is used for catheterization of the celiac and superior mesenteric arteries and their branches. A Cobra catheter or a reversed-hook catheter with two sideholes placed at it tip is placed in the right hepatic vein for hepatic venous sampling. FIGURE 45–1. Veins and arteries of the head of pancreas, (a) A transhepatic venogram. a, catheter in hepatic vein; b, catheter in celiac axis; PV, portal vein; SMV, superior mesenteric vein; JV, proximal jejunal veins join the superior mesenteric vein at its confluence with the portal vein. The arrow points at transhepatic catheter. (b) Venogram of the gastrocolic trunk. PV, portal vein; GCT, gastrocolic trunk; A, anterior superior pancreaticoduodenal vein; GE, gastroepiploic vein. (c) Selective injection into the gastroduodenal artery. gd, gastroduodenal artery; aa, anterior superior pancreaticoduodenal artery; pa, posterior superior pancreaticoduodenal artery; ipd, inferior pancreaticoduodenal artery; ge, gastroepiploic artery dp, dorsal pancreatic artery; tp, transverse pancreatic artery; pm, pancreatica magna artery. Angiographic imaging techniques in general use are intraarterial digital subtraction angiography (IA-DSA) and conventional cut-film angiography. The technique of the IA-DSA is the same as that for conventional cut-film angiography, and it has several advantages over the conventional technique, including high contrast resolution, lower contrast doses, and shorter procedure time. Cut-film magnification angiography has value with sub-selective injection of contrast medium into the pancreas for the diagnosis of small islet adenomas. The angiographic examination of islet cell adenomas should begin with celiac and superior mesenteric angiography using 30 to 50 mL of contrast medium with filming up to 24 seconds to see the portal venous system. These provide a road map for subsequent superselective catheterization of the pancreatic arteries (splenic, gastroduodenal, and dorsal pancreatic arteries). A tumor blush and hepatic metastases may be seen on the celiac or superior mesenteric arteriogram. Catheterization Technique Transhepatic venous sampling usually is performed immediately after arterial catheterization. During the procedure, Versed and fentanyl are administered as needed. For patients with hyperinsulinism, intravenous glucose infusion (10% dextrose in water, 60 to 90 mL per hour) is started to maintain blood sugar within normal limits and thus prevents hypoglycemic attack during the examination

 Pancreatic Endocrine Tumors
Pancreatic Endocrine Tumors
 Vascular Anatomy
Vascular Anatomy
 Pancreatic Angiography
Pancreatic Angiography
 Transhepatic Venous Sampling
Transhepatic Venous Sampling
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree