Presentation and Presenting Images
A 70-year-old female presents for screening mammography. She has a history of left breast cancer treated 2 years ago with a lumpectomy but not radiation therapy, which she declined.
57.2 Key Images
( ▶ Fig. 57.3, ▶ Fig. 57.4, ▶ Fig. 57.5)
57.2.1 Breast Tissue Density
The breasts are almost entirely fatty.
57.2.2 Imaging Findings
There are postsurgical changes in the upper outer quadrant consistent with the patient’s prior lumpectomy for DCIS 2 years ago. The skin incision is marked with a wire marker. On the conventional craniocaudal (CC) mammogram, there is an asymmetry that is just lateral to the prior lumpectomy site ( ▶ Fig. 57.3). The corresponding tomosynthesis images demonstrate a focal asymmetry at the 2 o’clock location in the middle depth ( ▶ Fig. 57.4 and ▶ Fig. 57.5). The asymmetry was obscured by the overlapping tissue on the conventional mediolateral oblique (MLO) mammogram ( ▶ Fig. 57.2).
57.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
57.4 Diagnostic Images
( ▶ Fig. 57.6, ▶ Fig. 57.7, ▶ Fig. 57.8, ▶ Fig. 57.9, ▶ Fig. 57.10, ▶ Fig. 57.11, ▶ Fig. 57.12, ▶ Fig. 57.13, ▶ Fig. 57.14)
57.4.1 Imaging Findings
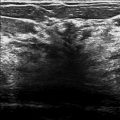
The diagnostic imaging further delineates the developing asymmetry on the both the CC and MLO spot-compression images ( ▶ Fig. 57.6, ▶ Fig. 57.9 and ▶ Fig. 57.7, ▶ Fig. 57.10) to be at the 2 o’clock location, 6 cm from the nipple. The targeted ultrasound demonstrates the 4-mm hypoechoic mass with indistinct margins at the 2 o’clock location, 6 cm from the nipple ( ▶ Fig. 57.11 and ▶ Fig. 57.12). This mass is at the medial edge of the patient’s incision scar from the prior lumpectomy. The mass was biopsied with ultrasound guidance and the ribbon clip, placed at biopsy, is found at the location of the mass seen on tomosynthesis (arrow in ▶ Fig. 57.13 and ▶ Fig. 57.14).
57.5 BI-RADS Classification and Action
Category 4B: Moderate suspicion for malignancy
57.6 Differential Diagnosis
Ductal carcinoma in situ (DCIS): DCIS is more common to present as calcifications. It can also present as a focal asymmetry, a mass, or an architectural distortion. This patient had prior DCIS treated with lumpectomy and without radiation therapy. This lesion is in the local vicinity of her prior cancer treated 2 years ago and likely represents local treatment failure.
Invasive cancer: Invasive cancers can present in the same areas as DCIS. A biopsy yielding invasive cancer would be concordant and similarly would represent local treatment failure.
Fat necrosis: Fat necrosis can resemble tumor recurrence. It can appear as a focal asymmetry, a mass, or dystrophic calcifications. When the imaging findings are not characteristic, biopsy is often necessary to differentiate fat necrosis from carcinoma.
57.7 Essential Facts
Local treatment failure is likely to occur at or near the site of the original cancer and appear within the first 5 to 7 years after treatment.
Local recurrence can be in situ or invasive cancer.
Fat necrosis can occur around a surgical site and resemble a tumor. It typically occurs approximately 2 years after treatment.
Mammographic detection of small cancers at screening allows for the decision for breast-conserving therapy.
Not all patients have the same breast-conserving therapy. It is important to know the patient’s surgical outcome (surgical margin status) and whether they had radiation, chemotherapy, or hormonal therapy. These factors can influence local recurrence.
As patients undergo breast-conserving therapy, it is important to be aware of the normal treatment changes that can occur in the breast over time, and those that are abnormal and need further evaluation.
57.8 Management and Digital Breast Tomosynthesis Principles
Initial reports suggest that the interpretation time for digital breast tomosynthesis (DBT) with FFDM is roughly double that of full-field digital mammography (FFDM) alone. This is an important consideration if an entire screening practice is converted from FFDM alone to FFDM plus DBT. Additional time will need to be allocated for interpretation.
It is uncertain if the interpretation time persists or decreases over time with experience.
Many of the initial studies in DBT were simulations with inflated numbers of cancers, thus the results may not extrapolate to the real world. This should be taken into consideration when evaluating sensitivity and specificity, which in these experimental situations may be overstated.
Prevalent detection bias occurs when a new technology or test is introduced into a population. This can lead to increased cancer detection rates and outcomes when first introduced that are not observed in subsequent years.
57.9 Further Reading
[1] Conant EF. Clinical implementation of digital breast tomosynthesis. Radiol Clin North Am. 2014; 52(3): 499‐518 PubMed
[2] Dershaw DD. Breast imaging and the conservative treatment of breast cancer. Radiol Clin North Am. 2002; 40(3): 501‐516 PubMed
[3] Helvie MA. Digital mammography imaging: breast tomosynthesis and advanced applications. Radiol Clin North Am. 2010; 48(5): 917‐929 PubMed

Fig. 57.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree