Presentation and Presenting Images
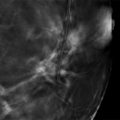
A 39-year-old female treated for left breast cancer with a lumpectomy, chemotherapy, and radiation therapy more than 10 years ago presents for screening mammography.
59.2 Key Images
59.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
59.2.2 Imaging Findings
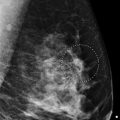
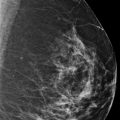
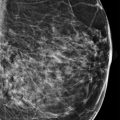
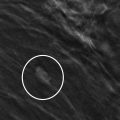
In the upper outer quadrant of the left breast, there are significant postsurgical changes that can be very distracting when reviewing a mammogram and looking for any changes ( ▶ Fig. 59.1 and ▶ Fig. 59.2). On first glance, the mammograms appear very similar to prior exams. However, the digital breast tomosynthesis (DBT) images suggest a developing asymmetry (comparisons not shown) adjacent to the postsurgical changes at the 3 o’clock location in the posterior depth ( ▶ Fig. 59.3 and ▶ Fig. 59.4).
59.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
59.4 Diagnostic Images
( ▶ Fig. 59.5, ▶ Fig. 59.6, ▶ Fig. 59.7, ▶ Fig. 59.8, ▶ Fig. 59.9, ▶ Fig. 59.10, ▶ Fig. 59.11)
59.4.1 Imaging Findings
The diagnostic imaging confirms the presence of an irregular mass with indistinct margins at the 3 o’clock location in the posterior depth ( ▶ Fig. 59.5, ▶ Fig. 59.6, and ▶ Fig. 59.7). The accompanying ultrasound examination demonstrates a 1.2 × 1.3 × 1.2 cm irregular mass with angular and indistinct margins located at 3 o’clock, 7 cm from the nipple ( ▶ Fig. 59.8 and ▶ Fig. 59.9). The mass has posterior acoustic shadowing. This mass was biopsied with ultrasound guidance, and the ribbon marker placed at the completion of the biopsy is located in the developing asymmetry, originally seen on the screening mammogram ( ▶ Fig. 59.10 and ▶ Fig. 59.11).
59.5 BI-RADS Classification and Action
Category 4C: High suspicion for malignancy
59.6 Differential Diagnosis
Recurrent invasive ductal carcinoma: The patient had cancer of the left breast many years ago, receiving a lumpectomy, radiation and chemotherapy. New masses or developing asymmetries near or at a surgical sight always raises concern for recurrent breast cancer.
Scar tissue: Post-treatment changes of the breast following surgery and radiation continue to evolve over time. A developing mass or calcifications in the treated breast need to be evaluated prior to dismissing it as post-treatment changes.
Fat necrosis: Fat necrosis can have many forms, from calcifications to spiculated masses. Similar to scars, developing changes need to evaluated prior to dismissing as part of the spectrum of fat necrosis changes.
59.7 Essential Facts
Breast-conserving therapy (BCT) is widely used for treating localized cancer. It is important to recognize the mammographic changes that occur in a conservatively treated breast.
Local recurrence after BCT is approximately 1 to 2% per year. Based on this estimate, a patient who has a mammogram 10 years after her initial cancer, has a 10 to 20% chance of recurrence at 10 years.
DBT allows the ability to scroll through image sets thus revealing findings that may have been obscured by background noise.
Lesions seen better on DBT can be more accurately assessed using the BIRADS classification.
59.8 Management and Digital Breast Tomosynthesis Principles
Any new or developing suspicious mammographic finding warrants evaluation regardless of how its appearance compares to the original cancer.
Factors that affect the detection of cancer lesions on mammography are technique sensitivity, distracting lesions, tumor growth rate, tumor growth pattern, and the background upon which the tumor is displayed.
The mammographic appearance of a recurrence does not always correlate with the appearance of the initial breast cancer.
59.9 Further Reading
[1] Andersson I, Ikeda DM, Zackrisson S, et al. Breast tomosynthesis and digital mammography: a comparison of breast cancer visibility and BIRADS classification in a population of cancers with subtle mammographic findings. Eur Radiol. 2008; 18(12): 2817‐2825 PubMed
[2] Weinstein SP, Orel SG, Pinnamaneni N, et al. Mammographic appearance of recurrent breast cancer after breast conservation therapy. Acad Radiol. 2008; 15(2): 240‐244 PubMed

Fig. 59.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree