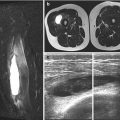
Fig. 7.1
Corner lesion (arrows in a and b) and bucket-handle lesion (arrows in c and d)
7.1.1 Rib Fractures
Rib fractures occur in older children in case of motor vehicle accidents, while in infants without metabolic bone disease, they are extremely rare, thus being highly suggestive of NAI (Fig. 7.2). Fractures of the first rib require even greater force than other rib fractures and strongly suggest abuse [11]. Barsness et al. [12] examining 62 rib fractures in children found that in the 82 % of cases, the lesions were due to abuse even reaching 95 % in children less than 3 years of age. Due to the plasticity of the young children’s skeleton, the rib cage can more easily deform rather than break. Rib fractures in infants are strongly correlated with abuse with a specific mechanism: adult hands pressing the infant chest generates squeezing force on the immature skeleton that may result in fractures of the anterior, lateral, and posterior aspects of the rib [13]. Sometimes, generally in large babies (>3,300 g) with difficult deliveries, rib fracture may be produced by a birth trauma. Posterior rib fracture is highly specific for NAI given that posteriorly the ribs are attached relatively tightly to the vertebral bodies and transverse processes. Since the forces are distributed in an area similar to the size of adult’s hands, fractures are typically seen in similar locations in multiple adjacent ribs and are often bilateral. Fracture healing occurs rapidly and may be divided into four stages: inflammation, soft callus, hard callus, and remodeling. Acute rib fractures appear as complete or incomplete linear lucent areas across the rib; however, if the fracture is incomplete or complete but nondisplaced or in an area with many overlapping structures, it may be hard to visualize, especially at the costovertebral joint. With healing, more fractures become apparent, as subperiosteal new bone and callus become evident. Thus, follow-up radiography performed 2 weeks after the injury increases the detection of rib fractures. Oblique chest radiography and bone scintigraphy are helpful to increase the detection of fractures. It has been shown that bone isotopic scan demonstrates radiographically occult rib fractures in 10 % of abused children [14]. Computed tomography (CT) performed in presence of polytrauma can easily depict rib fractures. Cardiopulmonary resuscitation may result in rib fractures more commonly in adults generally involving the anterior ribs, while posterior rib fracture does not result from such maneuvers. The rib fractures located on the middle axillary line have no distinctive characteristics from those determined by resuscitation. Spevak et al. [15] reported 0 % of rib fractures on autopsy in 91 infants who died after cardiac resuscitation, and Sewell reported no rib fracture after prolonged cardiac massage in a case of osteogenesis imperfecta type II [16]. Specificities of X-ray findings for infant abuse are listed in Table 7.1.
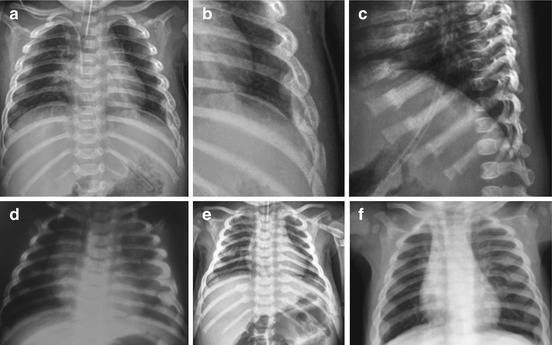
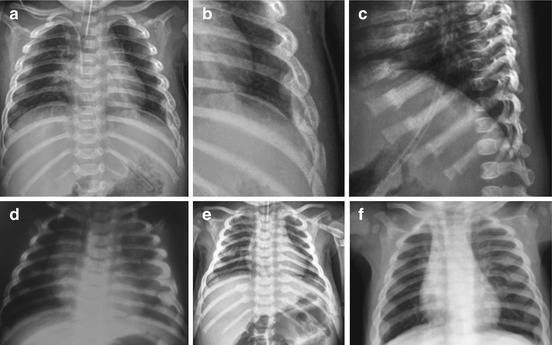
Fig. 7.2
Multiple rib fractures in different stages of evolution (a–c same patient; d–f other patients)
Table 7.1
Specificity of radiological findings in child abuse
High specificity | Moderate specificity | Common findings with low specificity |
|---|---|---|
“Classical” metaphyseal lesions | Multiple fractures, especially bilateral | Clavicular fractures |
Posterior rib fractures | Several fractures in different healing stage | Diaphyseal fractures of long bones |
Scapular fractures | Epiphyseal separations | Linear skull fractures |
Spinous process fractures | Vertebral body fractures and subluxations | Subperiosteal new bone formation |
Sternal fractures | Digital fractures | |
Complex skull fractures |
7.1.2 Other Fractures
Any type of fracture has been described in NAI. Particular attention should be given to the age and development of the child as well as to the injury and its mechanism. The given history for the injury is extremely important since it reveals the degree of force of the injury. Physeal fractures are rare under 3 years old. Type I Salter-Harris fractures in infants are not simply identified in the acute phase since the epiphysis is not ossified; thus, US can help in the correct diagnosis. Diaphyseal fractures of long bones are a common finding in children with a low specificity for abuse; this type of fractures generally occur as a result of accidental trauma in older children, while they are suspected for abuse in non-walking infants; “those who don’t cruise, don’t bruise” [17]. Multiple diaphyseal fractures in different stages of healing are shown in Fig. 7.3. Pelvic fractures in young children generally are due to motor vehicle accidents and, however, have been reported in NAI [18]. The domestic accidents as a fall from a high chair, a changing table, a sofa, a baby crib, or a bed are common and rarely lead to fractures or other serious injuries. A fall down the stairs is often used as an explanation for an inflicted injury, but epidemiologic studies of stairway falls demonstrate a limited injury pattern. In walking children, spiral fracture of the tibia called “toddler fracture” (Fig. 7.4) is common without a clear precedent trauma; it is not suspected of abuse, although it is often diagnosed already in the initial phase of healing because the child refuses to walk. Any vertebral fracture in children without a good explanation is suspected for NAI.
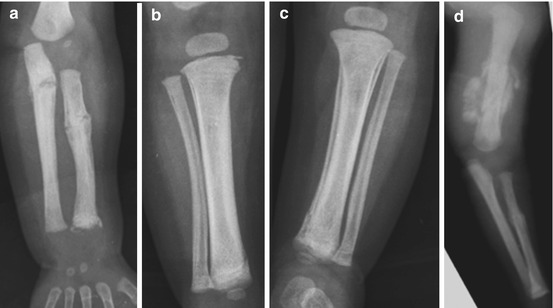

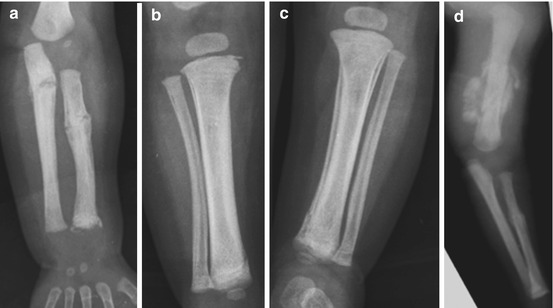
Fig. 7.3
Multiple fractures of long bones in different stages of healing (a–c on the same patient: radioulnar and tibioperoneal fractures; (d) another patient with humeral and radial fracture in different stages of healing)

Fig. 7.4
Toddler fracture: oblique metaphyseal fracture (black arrow) diagnosed during healing phase with slight periosteal reaction (white arrows). This fracture is not suspected for NAI
7.1.3 Fracture Healing in Children
Infants heal more quickly than older children and adults do. Dating the age of fractures in suspected abused children is very important, especially in the presence of more than one fracture and when the given history is suspect. The subperiosteal new bone (soft callus) is visible within 10 days after the injury. Calcified, and so visible, callus is observed in all fractures after 2–4 weeks (Fig. 7.5). Incomplete bridging of the fracture line is noted as early as 3 weeks after injury, and complete bridging with disappearance of fracture lucency is evident in almost half of the fractures at 10 weeks. Metaphyseal fractures can be dated with a good approximation: at a short distance from trauma, it is possible to detect marginal fragments of the physis and laminar gaps of the metaphyseal cortex; then, a progressive cortico-periosteal reaction occurs followed by the complete fusion of the fracture fragments to meta-diaphyseal region. Repeated and not treated subperiosteal hemorrhages determine after a few weeks the formation of thick periosteal sleeve and subsequently the cupping deformation of the metaphyses producing permanent alterations of the limbs such as bowing and dysmetria. Radiologists should be able to distinguish recent from old fractures, to determine if a fracture (excluding skull fractures) is in phase of healing as well as to recognize whether the fractures are of similar or different age in presence of multiple fractures.


Fig. 7.5
Repair process: (a) right humerus: partial detachment associated with reparative periosteal apposition. (b) After 2 weeks complete fusion of the fracture fragment (c) left humerus: corner lesion (c) and complete repair after 2 weeks (d); (e) distal tibial corner fracture; (f) large periosteal apposition after 10 days and complete healing after 38 days (g)
7.2 X-Ray of the Skeleton
X-ray of the skeleton is the first study in suspected NAI if the baby is in a stable condition. In order to make a correct diagnosis, X-rays need to be technically well done. Skeletal radiograph allows:
To detect a hidden damage to the bone
To get additional information about a clinically suspected NAI
To date the injury
To discover any disorder of the musculoskeletal system that can predispose to a fracture
The X-ray study must be carried out in a technically correct way and must be of high diagnostic quality. The right timing of the X-ray allows the early identification of a NAI and an immediate alert of the security team in order to promptly support the child. In fact, a delay in the examination might help parents to provide an alibi as declaring that the trauma occurred during hospitalization. When the child refers to the Department of Diagnostic Imaging, the radiological staff must be in contact with the staff that takes care of the child so that the X-ray is performed in the most appropriate time, and after the examination the child can go back to the clinical reference for ongoing care, thus suggesting the need of a multidisciplinary assessment. The X-ray must be made in accordance with the principles of accuracy and radiological high quality, which include highly technical factors, patient positioning, correct exposure factors for age and weight, and appropriate protections. In all radiographs, the name of the patient, a side marker studied, the date, and the time of the test must be clearly and correctly visible. The radiologist may request additional views if necessary. It is important that each anatomical area is examined with a separate exposure in order to optimize image quality. In particular, the whole skeleton (“babygram”) should not be performed on a single X-ray. Soft tissues as well as bone must be studied, since soft tissue swelling can be an indirect sign of fracture.
The radiographic views that should be performed in all cases of suspected NAI are shown in Table 7.2. X-rays are of extreme importance during the follow-up too, in order to confirm or exclude the diagnosis of NAI. The X-ray follow-up substantially increases the discovery of rib and metaphyseal fractures. In case of strong suspicion of NAI, it is necessary to perform a complete X-ray of the skeleton (except the skull) for the detection of occult fractures not seen on the first X-ray examination. In case of equivocal findings, in some areas at the first examination, it is necessary to repeat screenings of these anatomical areas to demonstrate radiographic signs suggestive of bone healing. The timing of the follow-up is crucial for dating the fractures. Radiographic examination should be repeated approximately 2 weeks after the first examination (from 11 to 14 days), even if this behavior has potential drawbacks: delay in diagnosis in some cases, inability to properly handle the child and his family as a result of delay, difficulty in deciding the place in which the child will stay in the interval between the first and the second examination, and possibility that the child will miss the X-ray follow-up. In our hospital, we use a system of flat panel detectors (“flat panel detectors,” FPD), which result in a higher image quality and in a substantial X-ray exposure reduction. In newborns, the kV range used for radiographic examination of all the skeletal segments ranges from 55 to 70. The focus-film distance is ~100 cm. Both joints should be included in the examinations of the long bones. Chest X-ray should be performed using the bone technique. The radiology report should provide a concise description of all the areas where a fracture is present or suspected. It is very important to collect precise informations about the event. The inconsistent responses should not be contradicted. The radiologist’s goal in the suspected NAI is to identify injury by imaging (in agreement with ALARA – As Low As Reasonably Achievable), to check the congruence between history and lesions diagnosed, to determine whether the etiology of the lesions is virtually non-accidental, to discover the age of injury, and, in doubt of abuse, to cooperate with physicians, coroner, magistrate, etc. [19].
Table 7.2
The skeletal survey in suspected infant abuse
Anteroposterior chest including clavicles |
Lateral chest |
Anteroposterior humeri |
Anteroposterior forearms |
Posteroanterior hands |
Anteroposterior pelvis |
Lateral lumbar spine |
Anteroposterior femora |
Anteroposterior tibiae |
Anteroposterior feet |
Anteroposterior skull |
Lateral skull |
7.2.1 Radioisotopic Bone Scanning
Scintigraphy is extremely sensitive in the identification of fractures and in some cases is able to demonstrate traumatic lesions invisible or hardly detectable at the first X-ray of the skeleton. Considered together, radiography and skeletal scintigraphy identify a greater number of traumatic injuries. CT has the same role in NAI and in accidental bone trauma. It is able to define the extent and severity of complex fractures and/or fractures unrecognized by X-ray and in particular vertebral, sternal, scapular, pelvic, and complex joint fractures. MRI has a prominent role in the evaluation of soft tissue trauma, occurring alone or in association with skeletal trauma. Recently some authors emphasized the role of whole-body MRI with STIR sequences and Fluorine-18 NaF PET imaging for the study of skeletal lesions instead of skeletal survey [20, 21].
7.2.2 Postmortem Radiography
Children who die from a sudden and unexpected or unexplained death generally undergo autopsy to determine the cause of death. X-rays is needed to complete the autopsy and in doubt of abuse should be performed in a small field of view in order to highlight rib fractures and typical metaphyseal lesions that can suggest the diagnosis of NAI. Therefore, a postmortem radiographic skeletal survey must be done in all children who die under suspicious circumstances in the hospital before transporting to the coroner’s office.
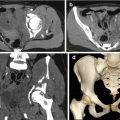
7.3 Visceral Lesions
Thoraco-abdominal visceral lesions from NAI are not common, representing 2–4 % of injuries. This type of lesions are described in all ages but are most common in children less than 3 years, with a high mortality rate (around 45–53 %) especially due to diagnostic and therapeutic delay [22]. Lesions of the hollow viscera are rarely found in accidental trauma in which single lesions of solid organs are most frequent; thus, they are highly suggestive of abuse. The injury can be caused by collision of solid organs against the spine, by compression of the hollow viscera against the column, by acceleration or deceleration of mobile structures, and rarely from blowout. Young children are more vulnerable because the ribs are more subtle, abdominal organs are more prominent, the abdominal walls are thinner, the muscles and skeletal structures are weaker compared to adult, and there is little protective fatty tissue around the pancreas, kidneys, and bowel loops. Most injuries occur in the duodenum (Fig. 7.6a, b) (with a prevalence of parietal hematoma due to the rich vascularization) and in proximal jejunum (with a prevalence of perforation due to the relatively fixed position) [23]. In stable patients, in case of suspect of visceral lesions, contrast-enhanced CT is the first investigation. It allows good evaluation of the lesion, shows the presence of free air or endo-abdominal fluid, and is the method of choice to detect lesions of the small bowel and mesentery. For an accurate diagnosis, it is important to get the correct timing of the contrast bolus. The examination should be performed without oral contrast medium, which could increase the risk of aspiration, especially if a child is sedated or immobilized. Protocols should be used with doses as low as possible (ALARA) in relation to the weight of the child, for example, not more than 80 KV in neonates and infants, directly after infusion of contrast medium. US has low sensitivity for lesions of solid organs and viscera and does not evaluate the bones and lungs; thus, it can be useful only in minor trauma and during follow-up of parenchymal lesions. In the chest pulmonary contusions, pleural effusion, cardiac laceration, esophageal rupture, aortic dissection, aortic pseudoaneurysm by direct trauma, and lethal “commotio cordis” are described [24]. In the abdomen, rarely can occur a gastric rupture with rapid onset of painful symptoms that can lead, especially if the diagnosis is delayed, to sepsis, shock, and death. Intramural hematoma in young children generally indicates abuse since it can be spontaneous only in case of purpura or coagulation disorders. It is manifested by partial or complete obstruction but often the symptoms appear late. Pancreas lesions are due to direct trauma to the upper abdomen. A complete pancreatic transection can occur (Fig. 7.6c, d) with a possible subsequent development of pseudocyst. Pancreatic lesions can evolve in early or late pancreatitis; in fact, pancreatitis in young children without a familiar history is suspected of abuse [25]. Visceral injuries are often associated to pancreatic lesions. Liver lesions are not frequent nor characteristics of NAI. The bleeding can be contained by the liver capsule or it can reach the peritoneal cavity. Most liver lesions are treated conservatively. Splenic and urinary tract lesions are not common in abuse and may be associated with other alterations. A scrotal hematoma can be caused by direct trauma or by extravasation of blood from the abdomen. There may be lesions of the penis. Vascular lesions are rare in children. Intra-abdominal vessels lesions are rare and may be associated with other lesions of the liver or the spleen.