Diffusion-weighted magnetic resonance imaging (DWI) provides image contrasts that are different from conventional magnetic resonance techniques. DWI is particularly sensitive for detecting acute ischemic stroke, but it also has many other clinical applications, including the evaluation of central nervous system (CNS) infections. This article addresses the role of DWI in the differential diagnosis of CNS infections, and discusses the most common DWI findings for each type of infection.
Infections of the central nervous system (CNS) continue to be a worldwide health problem, mainly in poor and developing countries. Because treatment options are available for most causes of CNS infection, the correct differential diagnosis must be obtained as early as possible. Clinical presentation and laboratory data are useful for differential diagnosis, but medical imaging is also important.
Magnetic resonance (MR) imaging is the method of choice for patients with CNS infections because it provides high anatomic resolution and tissue contrast, multiplanar acquisition, and high sensitivity to contrast enhancement. In addition, advanced MR imaging techniques, such as MR spectroscopy, diffusion-weighted imaging (DWI), diffusion tensor imaging (DTI), and dynamic-susceptibility contrast-enhanced perfusion MR imaging, provide metabolic and functional information about lesions, improving the diagnostic assessment. Of these advanced techniques, the DWI provides potentially unique information on brain tissue viability because its image contrast is dependent on the molecular motion of water, which may be substantially altered by infectious diseases. The aim of this review is to discuss the main clinical applications of DWI in the differential diagnosis of CNS infections, assessing the most common DWI findings in each type of infection.
Viral infection
Herpetic Encephalitis
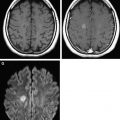
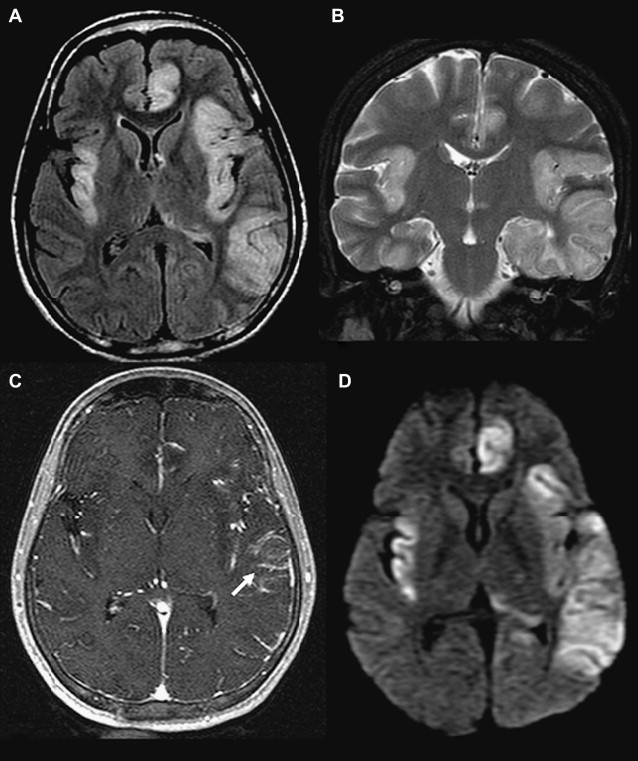
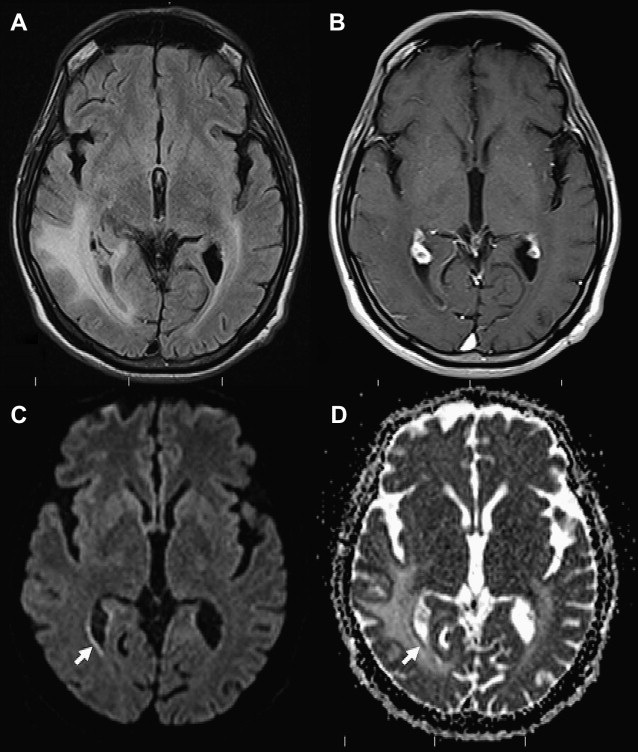
Herpes simplex virus type 1 (HSV-1) is the major causative agent of herpetic encephalitis and fatal sporadic encephalitis, with a high mortality rate. Laboratory findings are nonspecific, and isolation of HSV-1 from the cerebrospinal fluid is rare. MR imaging demonstrates early edematous changes in herpes encephalitis, with an increased signal in the temporal and inferior frontal lobes on T2-weighted imaging (T2-WI). This hyperintense signal involves both the cortex and white matter, and may be seen as early as 48 hours after the onset of symptoms. Herpes encephalitis typically shows heterogeneously restricted diffusion in the early stages of disease, when the inflammatory reaction is more severe. In some cases, DWI shows parenchymal alterations characterized by hyperintensity on DWI, even before abnormalities are noted on conventional MR imaging sequences, such as T2-weighted and fluid attenuation inversion recovery (FLAIR) images. The decrease in water diffusion is caused by cytotoxic edema, and is usually associated with irreversible neuronal damage undergoing necrosis, and poor outcome ( Fig. 1 ). DWI may also reveal large extensions and a higher number of lesions than T2-WI, and is the method of choice for monitoring treatment response. Facilitated diffusion with high apparent diffusion coefficient (ADC) values is seen later, in parallel with the development of vasogenic edema and encephalomalacia ( Fig. 2 ).
Human Immunodeficiency Virus
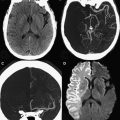
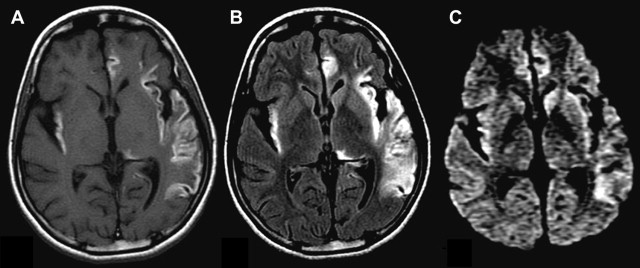
CNS involvement is an early feature of human immunodeficiency virus (HIV) infection. Although MR imaging is a sensitive technique for visualizing the effects of HIV in the brain, it cannot show early pathologic involvement. MR imaging features of brain HIV infection include bilateral symmetric increased T2-WI signal intensity in the white matter, and cerebral atrophy. At this stage, DWI may be normal or show “T2 shine-through” effects ( Fig. 3 ). HIV-positive patients in more advanced stages may develop dementia, also known as AIDS dementia complex, or HIV-associated dementia (HAD). HAD occurs in 20% to 30% of untreated adult patients. The clinical symptoms of HAD include disabling cognitive impairment accompanied by motor dysfunction, a change in behavior, or both.
Data from recent studies suggest that DTI might be sensitive for detecting early CNS involvement in HIV infection. Abnormal fractional anisotropy (FA) in the frontal white matter and internal capsules of HIV-positive patients has been demonstrated. In another study, a decrease in FA in the corpus callosum and an increase in mean diffusivity in the subcortical white matter were associated with high viral loads and low CD4 counts. However, the findings of brain areas with abnormal DWI and DTI findings, and the relationship between those variables and the clinical and laboratorial data, are discordant with other studies.
Progressive Multifocal Leukoencephalopathy
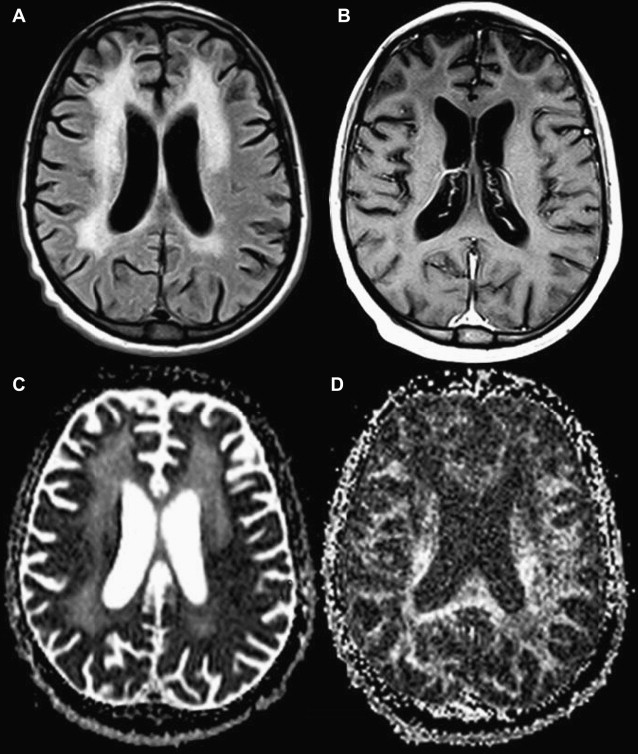
Progressive multifocal leukoencephalopathy (PML) is a serious subacute demyelinating disease of the CNS caused by JC polyoma virus infection of oligodendrocytes. JC virus infects approximately 70% of the human population and typically remains latent until reactivation by an immunodeficient state (common in AIDS patients). MR imaging findings suggestive of PML include the presence of bilateral asymmetric white matter lesions that are hyperintense on T2-WI and hypointense on T1-weighted imaging (T1-WI), and involve the subcortical “U” fibers with “scalloped” appearance, usually without mass effect. PML lesions usually have no significant mass effect and no contrast enhancement.
Recently, studies have used DWI to evaluate patients with PML, and suggested that DWI may detect areas of active disease more effectively than other sequences. Thus, DWI may be the method of choice for monitoring disease activity and eventual response to treatment. When evaluated by DWI, many PML lesions are characterized by a central core of low signal intensity surrounded by a rim of high signal intensity (area of disease activity) ( Fig. 4 ). The peripheral hyperintense rim progressively loses its signal intensity over time, while sustaining high signal intensity on conventional T2-WI. Recent studies also suggest that DWI may be useful for documenting the response of PML to highly active antiretroviral therapy. Usiskin and colleagues obtained serial ADC measurements using a b value of 3000 s/mm 2 , finding a marked reduction in lesional ADC, and a reconstitution of anisotropy in the affected areas that correlated with treatment response.
Other Infections
Herpes simplex virus type 2 is a major cause of neonatal encephalitis, and CNS is involved in approximately 30% of infected infants. Infection can result in microcephaly, seizures, microphthalmia, multicystic encephalomalacia, and death. Early findings, seen on MR imaging, include a reduction of distinction at the gray-white matter interface, and the associated edema may be difficult to distinguish from surrounding unmyelinated immature white matter, because both have an increased signal on T2-WI. Recent data proved that DWI is useful for early herpes encephalitis diagnosis. Lesions of herpes simplex encephalitis is seen on DWI as reduced (cytotoxic edema) or increased (vasogenic edema) movement of water molecules.
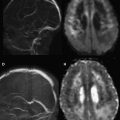
Cytomegalovirus, a virus in the herpes family, infects most infants by the end of their first year and, although rare in adults, is commonly seen in immunocompromised patients. Characteristic lesions are encephalopathy, subependymal spread, and more rarely, nodular focal lesions. Encephalopathy may occur as a rare acute form or, more frequently, a subacute/chronic form, resulting in a condition described as ventriculoencephalitis. MR imaging reveals focal encephalopathy with increased signal on T2-WI and often low signal on T1-WI, with no contrast enhancement. Subependymal spread is usually revealed only after contrast administration, and appears as a thin line of enhancement along the ventricular walls. Subependymal lesions may show reduced diffusion because of inflammation and cytotoxic edema ( Fig. 5 ).
Influenza virus is associated with various CNS lesions, many of them showing poor prognosis (acute necrotizing encephalopathy, Reye syndrome, and other types of influenza-associated encephalitis/encephalopathy). In acute influenza-associated encephalopathy/encephalitis, MR imaging shows lesions with diffuse or focal involvement of the cerebral cortex, the entire brain, or the bilateral thalamus. Recently, acute encephalopathy syndrome characterized by biphasic seizures and late reduced diffusion was reported. MR imaging shows no acute abnormality during the first 2 days after clinical onset, but reveals reduced diffusion in the frontal or frontoparietal subcortical white matter, with sparing of the peri-rolandic region, from days 3 to 9. The diffusion abnormality disappears between days 9 and 25, finally resulting in cerebral atrophy.
Subacute sclerosing panencephalitis (SSPE) is a slow progressive neurodegenerative infection by Morbillivirus genus viruses, characterized by fatal inflammation and sclerosis of the brain. Clinical manifestations, presence of elevated titers of measles antibodies in the cerebrospinal fluid (CSF) and serum, and abnormal complexes on electroencephalogram establish the diagnosis. There is little correlation between imaging findings and clinical stage. Early findings include a T2-WI signal increase in the frontal, temporal, and occipital white matter; less frequently, pial and parenchymal contrast enhancement, local mass effect, and edema are observed. Focal well-circumscribed areas of hyperintensity on T2-WI can be seen in the basal ganglia, especially the putamen. Atrophy may be the only finding in very slowly progressing cases of subacute sclerosing panencephalitis. For DWI findings, Kanemura and Aihara showed that the regional ADC of the frontal lobe decreased significantly with clinical stage progression, and increased to normal range during clinical improvement. Oguz and colleagues demonstrated increased diffusion of the periventricular white matter and centrum semiovale and reduced diffusion of the arcuate fibers. Finally, Trivedi and colleagues showed that FA values were significantly lower in the periventricular white matter in patients with SSPE and normal findings on conventional imaging, compared with the periventricular white matter of the controls in all cerebral lobes.
Bacterial infection
Cerebritis and Pyogenic Abscess
Cerebritis is the earliest manifestation of a cerebral pyogenic infection that may progress to a brain abscess. The histopathologic findings are characterized by a localized but poorly demarcated area of parenchymal softening with scattered necrosis, edema, vascular congestion, petechial hemorrhage, and perivascular inflammatory infiltrates at pathology studies. T1-WI MR imaging shows an ill-defined area of isointensity or hypointensity and subtle mass effect, with minimal or absent contrast enhancement. On FLAIR and T2-WI, the infected tissue is hyperintense. Cerebritis can appear as slightly reduced diffusion on DWI, probably related to hypercellularity, brain ischemia, or cytotoxic edema.
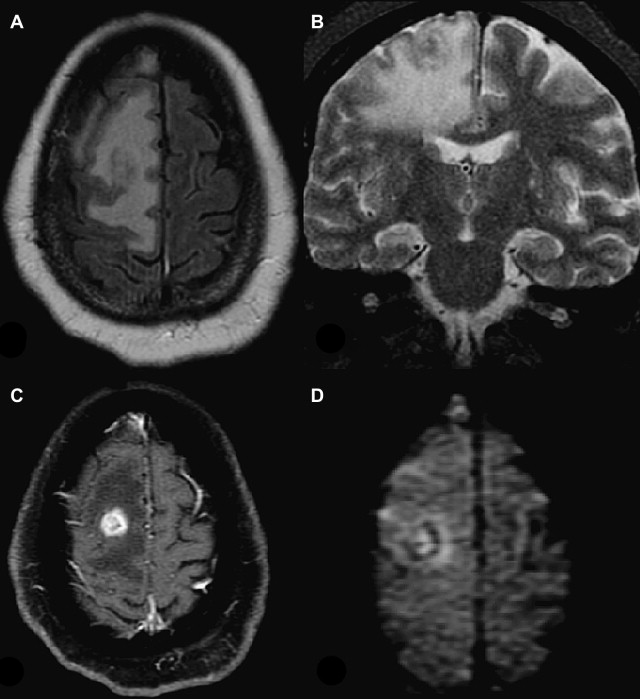
Pyogenic brain abscesses account for only 2% of intracranial mass lesions, commonly viewed as circumscribed, enlarging, focal infections. Brain abscesses may occur from hematogenic dissemination of extracranial foci, from the extension of meningeal or nasosinusal infections, or after trauma and surgical procedures. MR imaging of a typical abscess with a central liquefactive necrosis shows that the center of the cavity is slightly hyperintense to CSF, while the surrounding edematous brain is slightly hypointense to the normal brain parenchyma on T1-WI. On T2-WI the signal intensities are variable, depending on the protein composition and viscosity of the material in the central cavity. Usually an isointense-to-slightly hyperintense rim appears on T1-WI, and is hypointense on T2-WI. Ring enhancement after gadolinium administration is frequently seen, with a smooth and thin-walled ring that is often thinner along the medial margin.
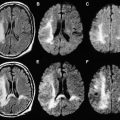
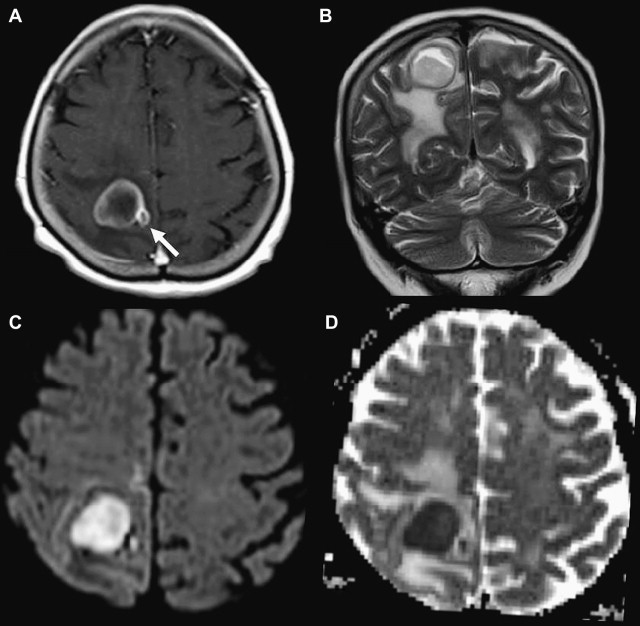
DWI usually shows reduced diffusion in the center of pyogenic brain abscesses ( Fig. 6 ). This appearance might be related to the high viscosity and cellularity of pus, which restricts water proton mobility. However, care is needed when interpreting DWI and ADC maps of pyogenic abscesses, because small lesions may have normal ADC values. In addition, in the early stages of a pyogenic abscess, during capsule formation, reduced diffusion may be restricted to the wall of the lesion, making differential diagnosis from another infectious causes of brain abscesses and necrotic tumors difficult ( Fig. 7 ). ADC values may vary with the age of an abscess and the course of therapy. Ketelslegers and colleagues reported a case of a pyogenic abscess in which the ADC values increased from 0.63 by 0.79 × 10 −3 mm 2 , to 1.10 by 1.29 × 10 −3 mm 2 over 3 weeks of treatment. Another potential factor that may influence ADC values in an abscess is host immune status. In many studies, absolute ADC values are used rather than ADC ratios. Absolute values may be more susceptible to errors in measurement.
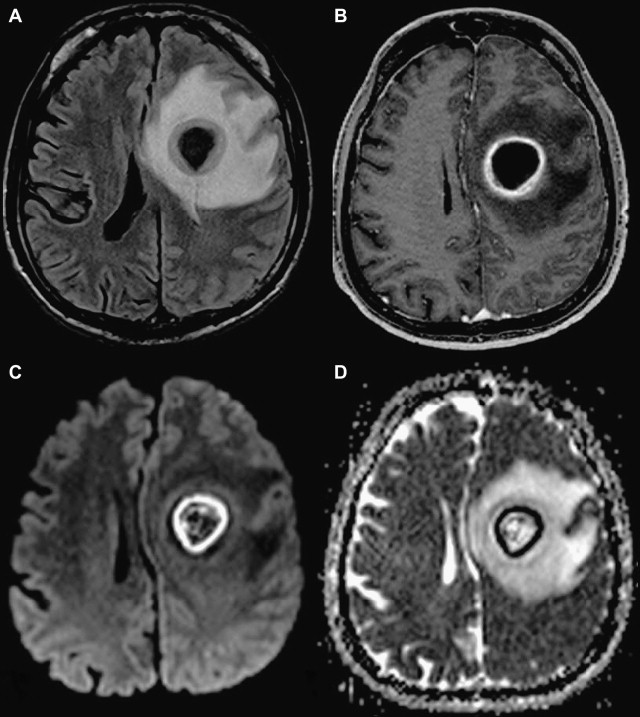
DWI is also used to distinguish brain abscesses from necrotic or cystic neoplasms. Fertikh and colleagues assessed DWI findings for a series of 53 patients with ring-enhancing masses in the brain (26 abscesses and 23 neoplasms). The mean ADC ratios were significantly higher in neoplasms than in abscesses (2.45 vs 1.12). The accuracy of ADC ratios in discriminating abscesses from neoplasms, determined by the area under the receiver operating characteristic curve, was high, 0.91 ± 0.04 (mean ± standard error of the mean). ADC ratios were significantly higher in neoplasms than in pyogenic abscesses, but no difference was seen in ADC ratios between neoplasms and nonbacterial abscesses. In addition, the efficiency of the DWI increased from 87% to 94.3% when information about the presence of a T2 hypointense rim was added. The investigators concluded that ADC measurements significantly helped in distinguishing brain abscesses from necrotic or cystic neoplasms, and that ADC measurements were more reliable in cases of bacterial abscesses than in nonbacterial cases. This finding is important because cerebral abscesses can be stereotactically aspirated, avoiding a formal craniotomy in tumor treatment ( Fig. 8 ).
Tuberculosis
Meningitis is the most common intracranial manifestation of tuberculosis (TB). It is usually more prominent in the basilar cisterns, especially around the circle of Willis. However, tuberculomas, tuberculous abscess, and cerebral ischemia and infarction are not uncommon findings. The most common imaging findings associated with CNS TB include enhancement of the basal cisterns, granulomata, calcifications, hydrocephalus, meningeal enhancement, and infarction, most often of the basal ganglia. Coexistent pulmonary TB is seen in 25% to 83% of cases of CNS TB. Tuberculous leptomeningitis from CNS TB may directly involve intracranial arteries through the inflammatory infiltrate, or indirectly through reactive endarteritis obliterans, resulting in thrombosis and infarction. Infarctions are even more common in children. The middle cerebral artery and its branches are most often affected, especially the small perforating branches supplying the basal ganglia. In these patients, DWI is essential for differentiating between direct extension of the infection to the brain parenchyma, and infarction. Reduced diffusion is usually seen in the infarction, while direct extension of the infection results in more heterogeneous signal intensity on DWI and ADC maps.
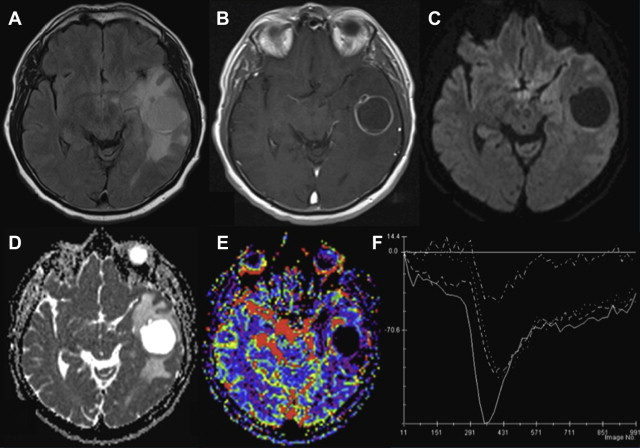
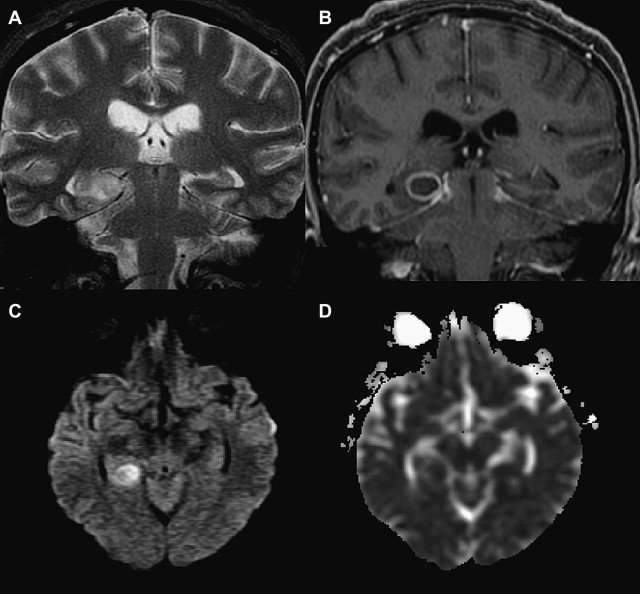
Tuberculomas are granulomas that usually develop from either hematogenous spread or extension from CSF via cortical veins or small penetrating arteries. On T2-WI, they are usually hypointense and show nodular enhancement in the early stages. During this phase, the tuberculomas may present with heterogeneous signal intensity on DWI and ADC maps, showing reduced or increased diffusion ( Figs. 9 and 10 ). As they mature, they develop a T2-WI hypointense center surrounded by an isointense capsule corresponding to solid caseation necrosis, and have ring enhancement. Tuberculous abscesses are more common in HIV-infected patients. These abscesses range from 3 to 20 cm 3 and are hypointense on T1-WI and hyperintense on T2-WI, showing well-defined rim enhancement on postcontrast images. Although tuberculous abscesses may show reduced diffusion in the walls and increased diffusion in the center of the lesion, comparative analysis of ADC values from the walls of the pyogenic, tuberculous, and fungal abscesses have shown no significant differences.
Syphilis
Neurosyphilis is a sexually transmitted disease caused by Treponema pallidum . Symptomatic cases can be divided into 4 types, based on the predominant clinical features: meningeal, vascular, general paresis, and tabes dorsalis. The most common forms of neurosyphilis are meningeal and vascular. Pathologically the meningeal form has acute inflammatory meningeal infiltrate, with neuritis and gumma formation. The vascular form is characterized by vascular endarteritis, causing irregular stenosis of medium or large vessels; and syphilitic gummas may occur in the parenchyma or may be extra-axial, and are characterized by areas of granulated tissue surrounded by mononuclear cells and epithelial fibroblasts.
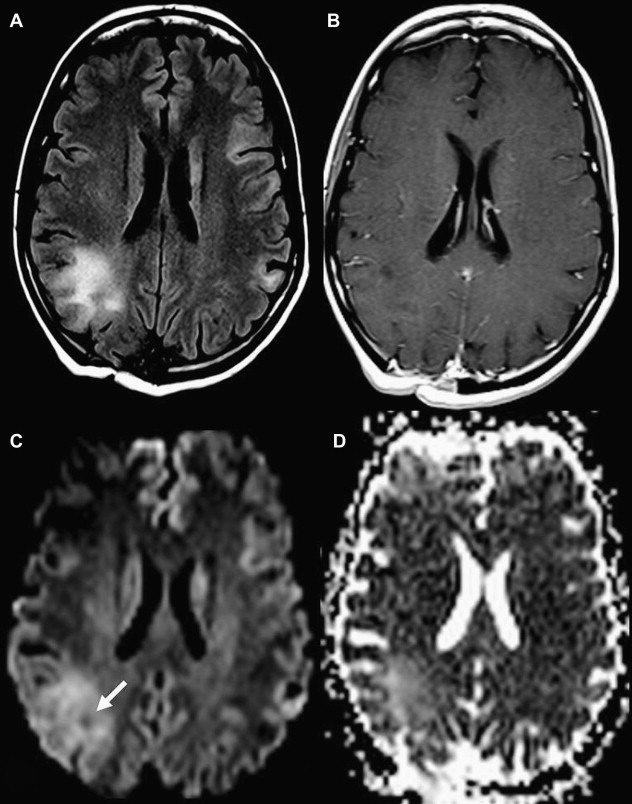
Neurosyphilis has a wide range of imaging findings, such as atrophy, white matter lesions, infarctions, gummas, meningeal enhancement, and arteritis. Evidence of infarctions of various ages may be seen, and meningovascular syphilis should always be considered when evaluating an HIV-infected patient who presents with cerebral infarction. The infarcts are typically located in the perforating artery territory of the basal ganglia and brainstem ( Fig. 11 ). DWI is important for these patients, because it shows acute infarctions as reduced diffusion. For cerebral gummas, MR imaging shows hypointense to isointense lesions on T1-WI, and hyperintense lesions associated with central nodular enhancement and surrounding edema on T2-WI. Reduced diffusion of water molecules can also be seen in these lesions. The exact mechanism for restricted diffusion in the gumma is unclear, but may be due to cytotoxic edema of inflammatory cells.
Others
Septic emboli
Cerebrovascular occlusions by septic embolism usually occur in patients with bacterial endocarditis, history of intravenous drug abuse, or cyanotic heart disease. MR imaging findings may vary from major arterial branch infarction to multiple small abscesses located at the gray-white matter junction, depending on the size of the emboli. As in other abscesses, DWI shows restricted diffusion within the lesions because of the pus content. In cases of very small lesions, reduced diffusion may not be seen.
Meningitis
Meningitis, an acute or chronic inflammatory process of the pia-arachnoid, is potentially serious in childhood because of the possibility of developing cerebral infarcts. DWI is a simple method for assessing the vascular and neurologic complications of bacterial meningitis. Infarcts, which are frequent, may be related to septic vasculitis, and the frontal lobes are most commonly involved. The size, location, and multiplicity of the infarcts correlate with outcome. Infratentorial lesions are associated with a poor outcome, whereas patients with a favorable outcome develop only a few small scattered lesions.
Empyema
Subdural and epidural empyemas account for about 30% of intracranial infections. Empyemas usually develop as a complication of sinusitis, otitis media, meningitis, trauma, or craniotomy. Both subdural and epidural empyemas appear as extracerebral collections of fluid showing intense enhancement of the surrounding membrane. On extra-axial collections, patients with subdural empyemas show a high signal on DWI, which is confirmed on ADC maps as restricted diffusion. However, epidural empyemas may also appear as areas of low signal, or a mixture of high and low signals on DWI ( Fig. 12 ). Therefore, the high signal on DWI and markedly diminished ADC distinguishes extra-axial empyemas from reactive effusions.
Pyogenic intraventricular empyema (PIE) is characterized by the presence of pus in the ventricles. Rupture of a brain abscess is the most common cause, but extension of meningitis into the ventricles and a neurosurgical procedure or device are also described. DWI is the most sensitive MR sequence for PIE diagnosis, and it is characterized by high signal intensity in the dependent portion of the ventricles and low signal intensity on ADC maps.
Bacterial infection
Cerebritis and Pyogenic Abscess
Cerebritis is the earliest manifestation of a cerebral pyogenic infection that may progress to a brain abscess. The histopathologic findings are characterized by a localized but poorly demarcated area of parenchymal softening with scattered necrosis, edema, vascular congestion, petechial hemorrhage, and perivascular inflammatory infiltrates at pathology studies. T1-WI MR imaging shows an ill-defined area of isointensity or hypointensity and subtle mass effect, with minimal or absent contrast enhancement. On FLAIR and T2-WI, the infected tissue is hyperintense. Cerebritis can appear as slightly reduced diffusion on DWI, probably related to hypercellularity, brain ischemia, or cytotoxic edema.
Pyogenic brain abscesses account for only 2% of intracranial mass lesions, commonly viewed as circumscribed, enlarging, focal infections. Brain abscesses may occur from hematogenic dissemination of extracranial foci, from the extension of meningeal or nasosinusal infections, or after trauma and surgical procedures. MR imaging of a typical abscess with a central liquefactive necrosis shows that the center of the cavity is slightly hyperintense to CSF, while the surrounding edematous brain is slightly hypointense to the normal brain parenchyma on T1-WI. On T2-WI the signal intensities are variable, depending on the protein composition and viscosity of the material in the central cavity. Usually an isointense-to-slightly hyperintense rim appears on T1-WI, and is hypointense on T2-WI. Ring enhancement after gadolinium administration is frequently seen, with a smooth and thin-walled ring that is often thinner along the medial margin.
DWI usually shows reduced diffusion in the center of pyogenic brain abscesses ( Fig. 6 ). This appearance might be related to the high viscosity and cellularity of pus, which restricts water proton mobility. However, care is needed when interpreting DWI and ADC maps of pyogenic abscesses, because small lesions may have normal ADC values. In addition, in the early stages of a pyogenic abscess, during capsule formation, reduced diffusion may be restricted to the wall of the lesion, making differential diagnosis from another infectious causes of brain abscesses and necrotic tumors difficult ( Fig. 7 ). ADC values may vary with the age of an abscess and the course of therapy. Ketelslegers and colleagues reported a case of a pyogenic abscess in which the ADC values increased from 0.63 by 0.79 × 10 −3 mm 2 , to 1.10 by 1.29 × 10 −3 mm 2 over 3 weeks of treatment. Another potential factor that may influence ADC values in an abscess is host immune status. In many studies, absolute ADC values are used rather than ADC ratios. Absolute values may be more susceptible to errors in measurement.