The objective of this article was to emphasize the use of diffusion-weighted imaging in the diagnosis and follow-up of several major disease contexts, as established in recent literature. In some of these diseases the diffusion changes are correlated with the clinical deficit and are potentially useful for early diagnosis and longitudinal evaluation, as well as in the context of pharmacologic trials. Diffusion magnetic resonance is a major advance in the continuing evolution of MR imaging. It provides contrasts and characterization between tissues at a cellular level that may imply differences in function as well as framework and have contributed to a better understanding of the pathophysiological mechanisms of several diseases.
Magnetic resonance (MR) imaging is currently the most widely used tool for the evaluation of pathologic processes that affect the central nervous system (CNS), allowing the delineation of anatomic structures that are affected and, in many situations, an inference of the pathologic substrate. In this way, MR imaging can be used to identify inflammatory/infectious, demyelinating, neoplastic, and vascular diseases, among others. New image sequences have recently been developed; among these, there is particular interest in those based on the random motion of water molecules. These sequences allow the investigation of the hemodynamic, metabolic, functional, cellular, and cytoarchitectural status of brain tissue under different physiologic or pathologic settings, thus increasing the sensitivity and specificity of MR imaging studies. The biologic behavior of a particular disease can be measured by such methods, enabling confident diagnosis and appropriate approach, as well as the recognition of related prognostic factors. These techniques can also be used to monitor disease response to the therapeutic regimen.
The physical principles of the diffusion sequence are complex, and a detailed explanation of these principles is beyond the scope of this text. The contrast in tissues obtained from sequence diffusion-weighted imaging (DWI) is based on the stochastic displacement of water molecules, in different structures and tissues, which determines the attenuation of the MR imaging signal intensity in the presence of a strong magnetic field gradient. The degree of attenuation depends on the strength of the gradient, the length of time for which it is applied, and the magnitude of water diffusion. The free movement of water molecules can be prevented by a decrease in the volume of the extracellular medium (increased cellularity), changes in the ion transport across membranes, and a decrease in intracellular water content (increase in the nucleus-to-cytoplasm ratio); thus, any of these situations can modulate the intensity of the signal sequence.
Normal brain characteristics can be modified under pathologic conditions and influenced by various therapies. The DWI is important in the study of many different CNS disorders; the objective of this article was to emphasize the use of DWI in the diagnosis and follow-up of several major disease contexts, as established in recent literature.
Vascular diseases
Stroke
The perfect function of ion channels is directly related to the free movement of water molecules through the cell membrane, which requires a constant input of energy. Thus, neuronal and glial metabolism requires an adequate supply of oxygen, glucose, and other nutrients, which, in turn, depends on an efficient circulatory system.
Ischemic or hemorrhagic stroke may ultimately cause irreversible injuries. However, an early diagnosis of the ischemic vascular event may allow appropriate therapy and prevent, or at least attenuate, a negative outcome. It is also critical to estimate the irreversibly involved area (ischemic core) and the potentially reversible area (penumbra), because there is a direct correlation between the proportional size of the core and the risk of hemorrhagic complication after thrombolytic therapy. These size estimates can be achieved by measuring the mismatch between the area of restricted diffusion and the area of perfusion deficit estimated in perfusion studies by MR imaging. Moreover, the scaling of the penumbra affects the likelihood of favorable clinical outcomes after fibrinolytic treatment with partial or complete recovery of the impaired neurologic function.
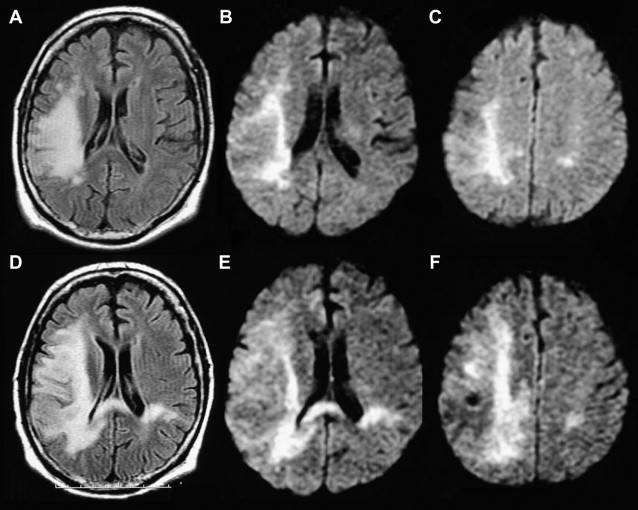
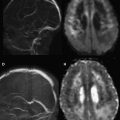
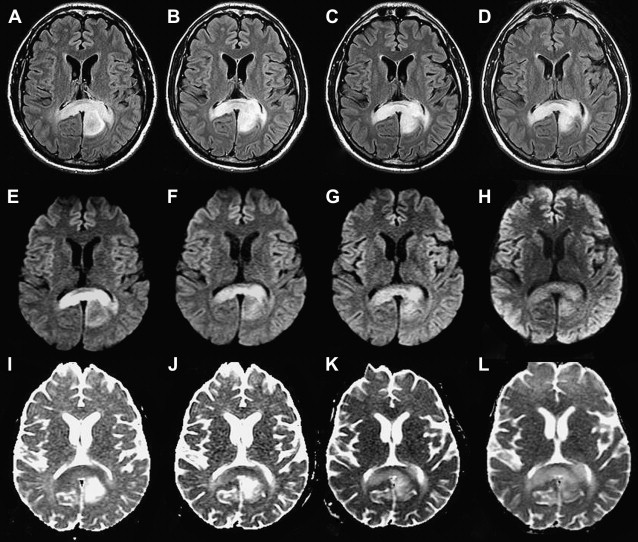
The ischemic core has experienced extreme energy deprivation and a consequent loss of cellular metabolism resulting from the dysfunction of the ATP-dependent Na + and K + pump. This leads to an intracellular influx of water and Na + , which restricts the movement of water molecules and consequently creates a focal hyperintense signal on DWI sequence, which can be confirmed by the apparent diffusion coefficient (ADC) map. This region was once considered unrecoverable, although the hyperintense signal observed in the DWI sequence is a marker of a recent ischemic event (acute/subacute), ie, documented soon after the occurrence of cytotoxic edema. These signals are usually obtained before conventional MR sequence modification. The restriction decays gradually because of cell death and the subsequent increase in the free movement of water molecules in the affected area ( Fig. 1 ). However, recent studies have suggested that damage to the area of restricted diffusion may be reversible in some situations. The main argument is that the restriction of diffusion in animals extends beyond the area of ATP-dependent pump impairment, which also correlates with the reduction of pH associated with anaerobic neuronal and glial metabolism. The diffusion tensor images (DTI) allow the visualization of areas suggestive of Wallerian degeneration in compromised brain regions, and is thus a promising technique for early estimates of reversibility.
Hypoxic-Ischemic Encephalopathy
Through some related mechanisms, global cerebral anoxia can also be diagnosed early on, and its extension can be established with great sensitivity through the DWI sequence. This provides a basis for early prognosis as well as the clinical management of the patient. Certain brain regions appear to be preferentially affected by anoxia, most likely owing to a mechanism of selective vulnerability rather than a segmental perfusion defect. The selective vulnerability of gray matter to anoxia can be attributed to its reduced blood flow, local basal metabolic rate, and the presence of receptors for excitatory amino acids. Ischemia causes an excessive release of glutamate that, after binding to the N-methyl- d -aspartate (NMDA) receptors, promotes the influx of calcium into the cell, initiating several cytotoxic processes such as the production of free radicals. This damages the cell membrane, allowing water to enter the cell and ultimately causing cytotoxic edema. The changes observed in the DWI sequence correlate with sites that are prone to cytotoxic edema, which are generally rich in glutamate receptors. In a less severe event, the neurons survive the initial insult but eventually suffer apoptotic cell death.
The MR imaging abnormalities found upon anoxia are variable and depend on several factors, including brain maturity, the severity and duration of the insult and the period of examination. Severe insults in term newborns cause selective injury to the lateral regions of the thalamus, the posterior region of the putamens, the perirolandic region, and corticospinal tract. These changes are observed as areas of hyperintensity on DWI sequence within the first 24 hours after the injury, during which the conventional sequences remain normal. However, during this period, the DWI usually underestimates the extent of anoxic injury, probably because of the apoptosis and delayed neuronal death that occurs later. Abnormalities on DWI peak at 3 to 5 days and “pseudonormalize” toward the end of the first week, reflecting the progressive increase in vasogenic edema and loss of cell membrane integrity. This apparent resolution of the DWI signal does not imply any real improvement, making evaluation with conventional MR images important during this period. Still, any negative DWIs performed within the first 24 hours after injury should be repeated at 2 to 4 days, when the restriction reaches its peak, for optimal interpretation. In term newborns, moderate anoxia causes injury in areas bordering the arterial irrigation and sites of minor perfusion, especially in the parasagittal regions. Again, DWI is the first sequence able to demonstrate the parenchymal abnormalities that appear within the first 24 hours, such as altered areas of hyperintensity in the cortex and subcortical regions of the affected site. However, we suggest that assessment with DWI should always be made in conjunction with conventional sequences and ADC values because restricted areas on the DWI may be masked because of the intrinsic high signal on T2 in the brain parenchyma observed in this age group. Areas of recent hemorrhage can also hamper the interpretation.
In preterm neonates, serious insult causes damage in areas similar to those detected in term neonates, ie, the thalamus, hippocampus, and cerebellum; less severe injuries are observed in the putamens and perirolandic region. Similarly, the DWI is altered early, typically with areas of hyperintensity, even though the conventional sequences still appear normal. The restriction zones reach a signal peak within 3 to 5 days, followed by pseudonormalization. The most common mild/moderate injuries in preterm neonates are periventricular leukomalacia and germinal matrix hemorrhage. Fu and colleagues have reported early findings of symmetric signal alteration of the periventricular white matter, similar to the findings observed in conventional sequences in the advanced stages of periventricular leukomalacia.
In older children and in adults, anoxia primarily affects the gray matter, mainly in the basal ganglia, thalamus, cortex, cerebellum, and hippocampus. Similarly, changes on DWI sequence occur early; hyperintensity can be observed before lesions appear on T1 and T2.
ADC maps and quantitative ADC of the whole brain parenchyma assist the assessment of brain damage and recovery potential in coma after cardiorespiratory arrest (CRA). A severe reduction in ADC in the first few days after global anoxia is highly indicative for permanent injury. The ideal period for the assessment is between 49 and 108 hours after CRA. A drop in the ADC over large regions of the parietal, temporal, and occipital lobes in the acute phase is associated with irreversible damage and the worst prognosis, regardless of electrophysiological test results. Lesions restricted to the thalamus and selective cortical regions suggest mild hypoxia, with potential neurologic recovery. Moreover, the ADC map can help to evaluate the benefit of various therapies; higher ADC values are observed in patients undergoing hypothermia.
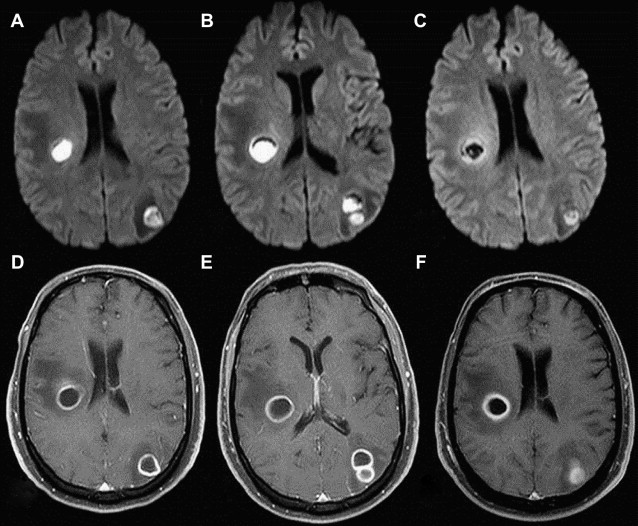
An intriguing entity known as postanoxic leukoencephalopathy occurs in 2% to 3% of patients after a diffuse cerebral hypoxic-ischemic event. It is characterized by a period of clinical stability or even improvement (lucid interval), followed by an acute neurologic decline, usually 2 to 3 weeks after the insult, involving delirium, personality changes, motor disturbances and, rarely, seizures. Typically, DWI sequence fails to reveal abnormalities at the time of the insult, but instead shows diffuse and confluent areas of restricted diffusion in the cerebral white matter at the end of the lucid interval, followed by a decrease in ADC values and signal change in T2 ( Fig. 2 ). Good clinical outcomes, as usual, are accompanied by the reduction of signal changes observed on DWI sequence and a progressive increase in ADC values. Presumably, postanoxic leukoencephalopathy may be caused by oligodendrocyte apoptosis (induced by previous anoxia) followed by diffuse demyelination.
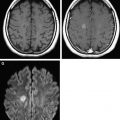
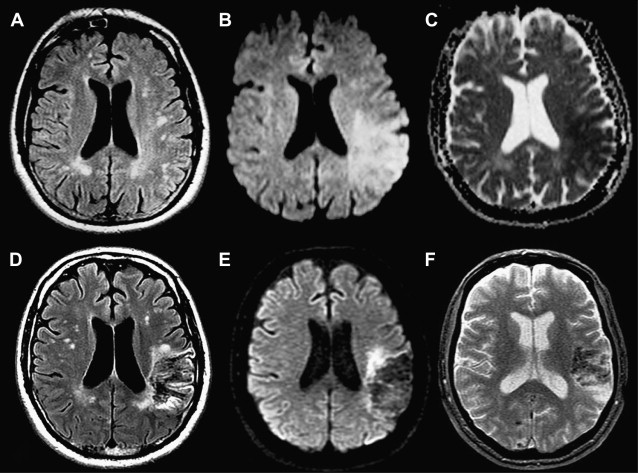
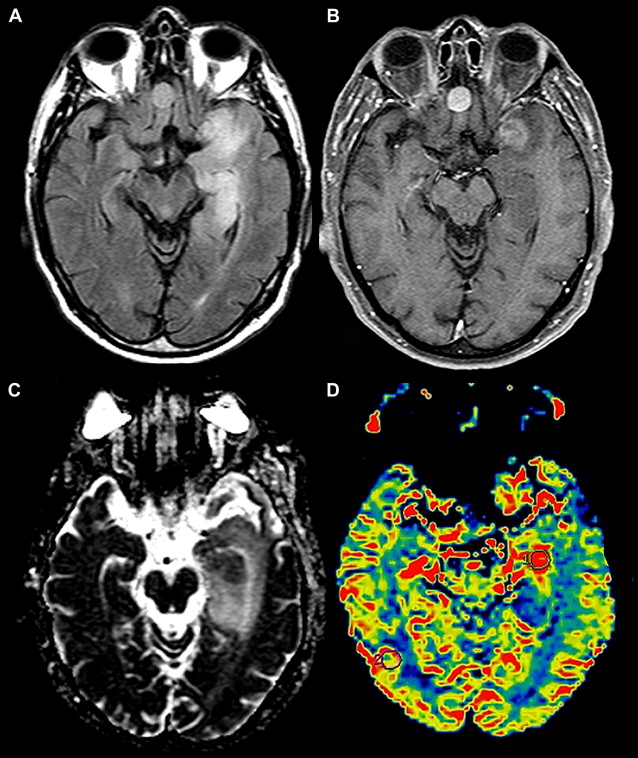
Posterior reversible encephalopathy syndrome (PRES) may be triggered by acute decompensation of blood pressure levels (eclampsia), immunosuppressive drugs (cyclosporine, tacrolimus), renal failure, systemic lupus erythematosus, and thrombocytopenia, among others. PRES is clinically characterized by altered consciousness, variable visual impairment, seizures, and headache. Its pathogenesis is not fully understood, but is known to be related to lower sympathetic tone of the brain vasculature in posterior regions (parieto-occipital) and endothelial microinjury, allowing macromolecule leakage during hyperperfusion that results in cortical and subcortical edema. This leads to an increase in interstitial pressure and a discrete compressive effect on the CNS, including small arteries. Reflexive vascular spasm is associated with this hemodynamic status. Rarely, vasospasm related to subarachnoid hemorrhage can also occur. The DWI sequence is especially relevant here, since this etiology can lead to reduced blood supply, resulting in tissue ischemia and subsequent cytotoxic edema. Thus, the presence of confirmed abnormalities on DWI sequence and ADC map indicate poor prognosis, ie, clinical and radiological irreversibility, whereas an abnormality on fluid-attenuated inversion recovery (FLAIR) with normal DWI defines a favorable clinical outcome ( Fig. 3 ). The reduction in fractional anisotropy (FA) might be caused by vasogenic edema, and should be used to indicate a favorable prognosis and reversibility.
Neoplasms
Glioma
Neoplasms of the CNS are a major cause of morbidity worldwide despite advances in surgical techniques and adjuvant treatment. The choice of therapeutic approach (and therefore its effectiveness) is directly related to the degree of tumoral differentiation, which cannot be established precisely by conventional imaging methods, especially in tumors that do not display classic signs of anaplasia, such as gadolinium enhancement or macroscopic necrosis.
The diffusion-weighted sequence can be used to estimate the degree of tumoral differentiation. High-grade tumors generally have a high nucleus/cytoplasm ratio, resulting in a reduction of the free movement of water molecules. Moreover, the size of the tumor, presence of residual tumor tissue after treatment, and even changes induced by treatment (eg, actinic ischemic sequelae) can be identified by DWI. Tracing the movement of water molecules through FA can be used to delineate the brain tracts, allowing a relatively accurate estimation of regional tumoral involvement/extension. This is possible because the high-grade tumors have expansive potential, which groups tracts of normal-appearing peritumoral white matter and simultaneously infiltrates this site, resulting in the interposition of tumor and necrotic cell/tumor cysts between these fibers, resulting in reduction of FA.
Tumors also release chemical mediators (eg, tumor necrosis factor) that increase regional vascular permeability, establishing the peritumoral edema. This edema further reduces anisotropy values and is easily identifiable in the reconstruction color maps as a reduction in the intensity of the colors of the affected fibers. Unlike high-grade tumors, low-grade neoplasms have a compressive effect only on the adjacent brain parenchyma and the corresponding fibers and tracts, but are not associated with the infiltration and peritumoral edema that increase regional anisotropy. This differential profile, in combination with apparent diffusion coefficients and conventional imaging with intravenous contrast, can contribute to a presumptive analysis of tumor grade.
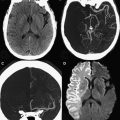
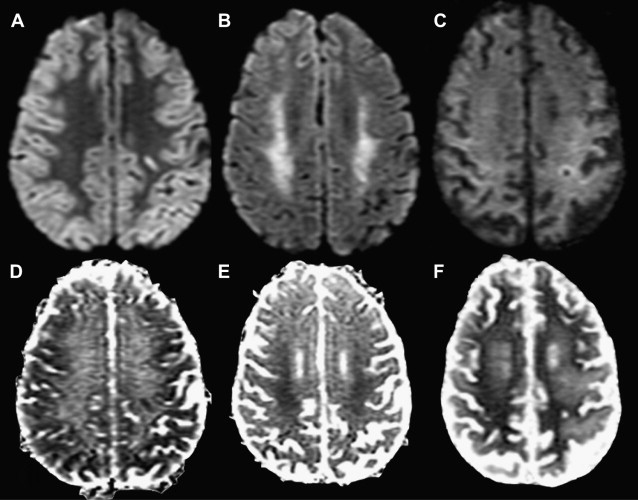
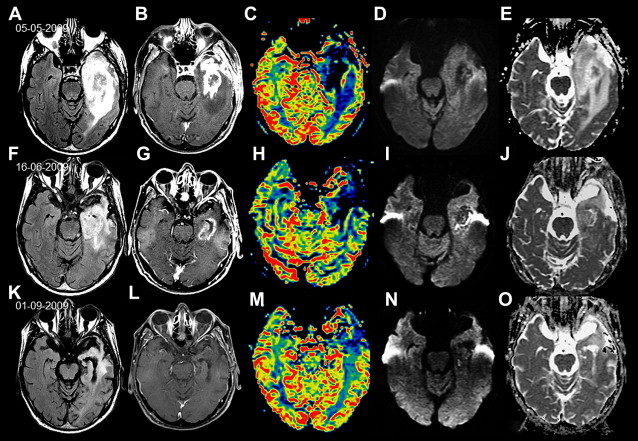
The utility of the ADC is not limited to diagnosis or to post-therapeutic monitoring. A recent study reported that neoplasms with low ADCs responded better to pretreatment than did lesions with high ADCs (related to tumoral necrosis). Experimental studies evaluating early treatment response used chemotherapy subdoses, noting changes in the ADC and even slight decreases in the viable tumor cell populations, which may be a biomarker of early response. Therefore, an early increase in ADC after or during chemotherapy or radiotherapy indicates a positive therapeutic response ( Fig. 4 ).
Tumor cells respond to invasive treatment by undergoing apoptosis, which releases intracellular water into the local environment. Cysts arising from tissue necrosis, especially in high-grade tumors, lead to significant heterogeneity in the neoplasm, and an extremely dynamic profile over the long periods of therapy. The calibration of the ADC by the ROI standard summarizes the mean and median of these values throughout the tumor but does not distinguish between areas of heterogeneity or characterize the tumor response at a particular location, which can yield an erroneous estimate of the therapeutic response. An alternative strategy is to evaluate the tumor voxel by voxel, a concept described as a functional diffusion map (fDM). These 3-dimensional maps allow superimposition of the ADC maps taken before treatment with those obtained during or after treatment, allowing a very precise delineation of the evolutionary changes in the tumor and thus its susceptibility to treatment. It is also possible to overlay these images with volumetric images taken with postparamagnetic contrast, increasing the sensitivity and specificity of the method.
The relative stability of ADC values in gliomas treated with corticotherapy after surgery belies changes in enhancement parameters (break of the blood-brain barrier), edema, permeability, and blood volume. This emphasizes the importance of monitoring tumors with diffusion-weighted images, which can differentiate between tumor progression and pseudoprogression. The presence of viable tumor cells leads to reduction of ADC values, unlike the vasogenic edema present in pseudoprogression ( Figs. 5 and 6 ). False-positive results can occur when tumor development is assessed by diffusion alone, for example, when there is significant leukocyte infiltration that increases regional cellularity and consequently reduces the ADC.
Lymphoma
Primary lymphoma of the central nervous system (PCNSL) represents 1% of all lymphomas, about 5% of non-Hodgkin lymphomas and 2% to 3% of CNS tumors. The most common histologic type of PCNSL is diffuse large B-cell lymphoma. The incidence of PCNSL differs between immunocompetent and immunocompromised individuals, as do the MR imaging characteristics of the disease. In immunocompetent patients, PCNSL is composed primarily of solid lesions, generally with homogeneous enhancement, and often without areas of necrosis. This presentation is unusual in immunocompromised patients, where the disease tends to affect the basal ganglia and the periventricular region and may contain foci of central necrosis or, less commonly, calcification and hemorrhage. The high cellularity of the PCNSL in both solid areas of viable tumor cells and necrotic foci (large populations of nonviable lymphocytes) restricts the free movement of water molecules in both segments, features that are important in differentiating the disease from an infection and in therapeutic follow-up ( Fig. 7 ). During treatment, the reduction of ADC values may indicate a good response, whereas the maintenance or elevation of this index suggests treatment failure or cancer progression.
Some recent studies have provided prospective quantitative assessments that promise to provide better detail of the microstructural disorganization of white matter involved in the neoplastic process (or its treatment) relative to its FA.
Infections of the Central Nervous System
Infections of the CNS are potentially fatal, occur in all age groups, and have varied clinical presentation and varied imaging characteristics and different etiologic agents. These diseases pose a diagnostic challenge for clinicians and neuroradiologists. MR imaging is a very sensitive tool for detecting early changes in this context.
The DWI has added specificity in some major classes of neural infections. Several studies have proven the effectiveness of this technique in differentiating between cerebral abscess and necrotic or cystic tumors. As a complement to the diagnosis, the assessment of therapeutic response, whether conservative or surgical, can be adequately estimated through follow-up with DWIs and ADC values. Here, we discuss the use of DWI and ADC in the diagnosis and follow-up of pyogenic, granulomatous, viral, and prion infections.
Pyogenic infections
The abscess is the most common focal CNS infection. It is often observed on hematogenous spread from distant foci, on direct inoculation (via trauma or surgery), on spread from an extracranial site, or as a complication of meningitis. The main signs and symptoms of the abscess result from expansive effects owing to the growth of the lesion: headache, altered mental state, focal deficits, seizures, nausea, and vomiting. Only 40% to 50% of patients are febrile in the early stages of neural infection. Abscess formation follows a predictable path that can be divided into 4 sequential stages: early cerebritis (1 to 3 days), late cerebritis (4 to 9 days), early capsule (10 to 14 days), and late capsule (beyond the 14th day).
In conventional MR imaging, the abscess appears as a lesion with ring enhancement and a thin and regular capsule. The capsule may present hypersignal on T1 and a hyposignal on T2, whereas the lesional content displays a hyposignal on T1 and a hypersignal on T2 because of perilesional vasogenic edema. Moreover, the presence of brain lesions with these characteristics does not ensure a diagnosis of the abscess; these must always be differentiated from primary or metastatic necrotic neoplasms and other infectious lesions. The first description of DWI used in this context was published by Ebisu and colleagues in 1996. These investigators observed high signal intensity within the abscess using this MR imaging sequence, associated with low ADC values, suggesting a real restriction of the free movement of water molecules, unlike what is observed in neoplastic lesions. The hypersignal intensity probably results from the physical and biochemical properties of the abscessed cavity. The presence of pus or mucus containing inflammatory cells, necrotic tissue, bacteria, and proteinaceous fluid gives the content high viscosity, with markedly restricted diffusibility. The signal abnormalities observed on DWI sequence are attributed to this set of conditions.
The treatment of pyogenic abscess varies and generally depends on the evolution of the lesion. Stereotactic aspiration followed by antibiotic therapy has been the method of choice for single or multiple abscesses, although aspiration may be declined in favor of broad-spectrum intravenous antibiotics in some situations (eg, lesions smaller than 2.5 cm). A second surgical drainage is recommended if the abscess increases in size after 2 weeks of treatment, or fails to respond within 3 to 4 weeks. The need for reoperation is relatively common, occurring in approximately 62% of cases.
All of the previously mentioned measures require reliable parameters for monitoring, so imaging methods that are able to confirm the stage of the abscess and reliably monitor its progress during and after the initiation of therapy are necessary. The literature has described MR spectroscopy as a potential tool for this purpose : the disappearance of pyogenic abscess peak markers (cytosolic amino acids, acetate, alanine, succinate) and presence of a single lactate peak imply successful treatment and a positive outcome. Still, the diffusion sequence seems even more promising in this context. Cartes-Zumelzu and colleagues have demonstrated the value of DWI in monitoring the therapeutic course applied to the abscess. These investigators reported a good correlation between the persistence or reappearance of a hyperintense signal on DWI and low ADC values after treatment (either surgical or clinical only) with pus reaccumulation within the lesion ( Fig. 8 ). Conventional MR sequences, when used in isolation, are not sufficient to predict the evolution of the lesion. The visual inspection of T1-weighted sequences after contrast may show a reduction in the size of the abscess, but this finding does not necessarily allow the inference of an appropriate response. Although the use of DWI to follow-up on abscess treatment is promising, some questions about its sensitivity and specificity for this purpose remain and further studies are required.
However, the interpretation of all these image signals must be made with caution, because the hyperintense signal on DWI of lesions with capsular enhancement is not pathognomonic for abscess. There are reports of metastatic adenocarcinoma or squamous cell carcinoma, and even radionecrotic lesions that present identically in the MR imaging.
Other applications of DWI in the context of neural infection include cerebritis, ventriculitis, and the empyemas. Cerebritis is the earliest manifestation of a cerebral infection, occurring about 2 to 3 days after pathogen inoculation, and may progress to abscess formation. An ill-defined area of coagulative necrosis is generated in response to the infectious agent, exhibiting extravasation of polymorphonuclear cells in the necrotic center and adjacent parenchymal edema with perivascular exudate. There are few studies demonstrating imaging of cerebritis, because most patients with cerebritis do not receive medical care during this stage. The several studies that do exist report low signal on T1 and a poorly delineated hyperintense signal on T2; perilesional vasogenic edema can be observed in the absence of evident parenchymal enhancement. However, the restriction of diffusion is also described in this phase, most likely a result of ischemia, hypercellularity, or cytotoxic edema, as there is still no purulent fluid. The diffusion resembles bacterial or fungal cerebritis. We were not able to find any report of the monitoring of cerebritis treatment using this MR method.
Pyogenic ventriculitis is an uncommon complication of intracranial infections in adults, but it is often found in pediatric patients with meningitis. Ventriculitis may be the source of persistent infection and treatment failure in the management of meningitis, usually caused by gram-negative bacteria. The imaging finding most characteristic of ventriculitis is the presence of irregular intraventricular debris. This can be identified in computed tomography (CT) and conventional MR sequences, but is more conspicuous in diffusion-weighted sequences. The high signal in this sequence is related to real restriction, as evidenced by low ADC values, unless only a small amount of diluted pus is present in the cerebrospinal fluid (CSF) (this is insufficient to reduce the ADC).
Hong and colleagues examined the importance of the ADC measured in the lower portions of the ventricles (CSF-dependent) in the evolution of ventriculitis in 12 patients and its correlation with CSF analysis. These investigators concluded that there is an inverse relationship between ADC values and pleocytosis or spinal fluid protein concentration; when the ADC values increased within the ventricle, both protein levels and pleocytosis decreased. These findings show that ADC values may be used in follow-up of these patients.
The epidural and subdural empyemas may be clinically differentiated based on the more insidious signs of focal expansive lesion and the absence of systemic manifestations in patients with epidural empyema. In contrast, subdural empyema is an acute condition that rapidly progresses to toxemia and neurologic abnormalities requiring immediate surgery. These infections are correlated with the presence of sinusitis and mastoiditis. Empyemas are best seen with a FLAIR sequence, but the purulent nature of the injury, as well as the presence of abscesses, is clearly confirmed in the diffusion-weighted sequence.
Granulomatous infections
The fungal cerebral abscesses are well-known entities in immunosuppressed individuals. Although the central restriction on DWI is present in nearly all pyogenic abscesses, these nonpyogenic infectious lesions have less specific characteristics. A homogeneous central restriction pattern identical to that seen in bacterial abscess can also be found in the fungal abscesses, reflecting the proteinaceous fluid and hypercellularity, as well as hematic content, that are common in infections caused by aspergillus. Therefore, this possibility should be considered and antifungal drugs should be included in the therapeutic regimen for such lesions, especially in immunocompromised individuals, when biopsy is impossible or results have not yet been received. Heterogeneous restriction patterns have also been described for fungal abscess, with restriction predominantly occurring on the walls and solid peripheral projections in these collections. It is assumed that these different patterns are generated by the complete or partial filling of the cavity by inflammatory cells and hyphae in the late capsular stage, giving the appearance of homogeneous or heterogeneous restriction, respectively. Importantly, Luthra and colleagues found lower ADC values in the restriction sites of the fungal abscess than in pyogenic lesions.
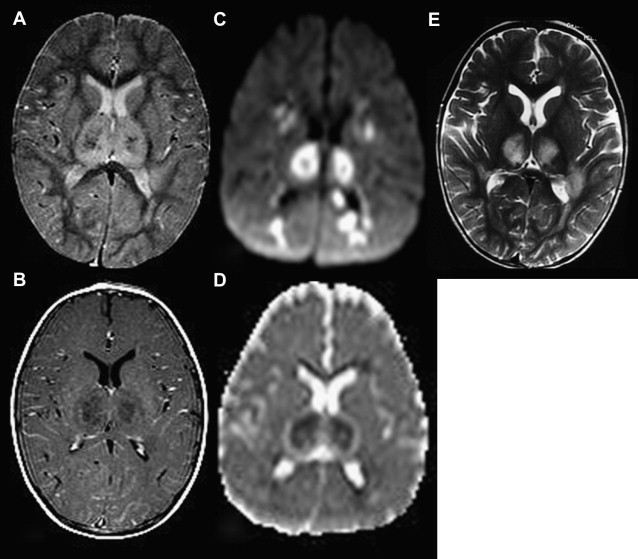
CNS infection is one of the more serious forms of Mycobacterium tuberculosis and is characterized by high morbidity and mortality. The AIDS pandemic has resulted in a significant increase of neural tuberculosis around the world. Tuberculous meningitis is characterized by the triad of cisternal meningeal enhancement, hydrocephalus, and deep infarcts, secondary to vasculitis of the medial lenticulostriate-striatal arteries and thalamic-perforating arteries (“medial TB zone”). Infarcts can be detected early by the DWI sequence as areas of high signal and low ADC values. In another form of CNS tuberculosis, the tuberculomas present a varied MR imaging signal according to their evolutionary characteristics and the presence of solid or liquid caseous necrosis. DWIs show restriction in tuberculomas with liquefied necrosis and no restriction in those with solid necrosis. Restriction of the diffusion in the presence of a low signal on T2 can contribute to the differentiation between lymphoma and tuberculoma in the context of brain focal lesions in patients with AIDS. The tuberculous abscess is a rare condition caused by M tuberculosis , constituting 4% to 7% of the total number of cases of neural tuberculosis in developing countries. The use of DWI in the diagnosis of such abscesses, as well as in pyogenic abscesses, reveals restriction with low ADC values, probably because of the presence of intact inflammatory cells in the pus. The evaluation of this sequence alone makes it difficult to differentiate between pyogenic and tuberculous etiologies.
Neurocysticercosis is the most important parasitic disease that affects the CNS and is a public health problem in developing countries. The cysts have a signal intensity similar to or slightly higher than CSF in all sequences, including DWI. The calculated ADC is high, with published values ranging from 1.55 to 2.25 × 10 −3 with slight variations according to the evolutionary stage of the parasite. These data make it possible to safely differentiate between neurocysticercosis and abscesses, whether pyogenic or tuberculous. Eccentric hyperintense signal in the DWI sequence at the location of the scolex in other sequences was described in at least 1 lesion of 7 cases with scolex studied by Raffin and colleagues. The ADC map showed a signal similar to that of CSF, and ADC measurement was not possible because of the small size of the nodule.
Viral encephalitis
The prototypical case of viral encephalitis is caused by herpes simplex. The herpes simplex virus type 1 (HSV-1) is the principal cause of fatal sporadic encephalitis, mainly producing focal encephalitis. The mortality rate reaches 70% in patients who received no treatment or incomplete treatment. The main features of this disease are signs and symptoms of focal encephalopathy, including headache, fever, neck stiffness, changes in personality and mental status, convulsions, and an acute decrease in consciousness associated with focal neurologic signs such as weakness, sensibility disorders, aphasia, defects in visual fields, and cranial nerve palsies. A polymerase chain reaction (PCR)-based technique is the method of choice for diagnosis, with sensitivity and specificity similar to those found for brain biopsies.
MR imaging, especially with diffusion-weighted sequence, is quite sensitive for the early diagnosis of herpes encephalitis, and can be used within the first 72 hours when PCR assays can yield false-negative results. The lesions are consistent with edema and inflammation, with low signal on T1-weighted and hypersignal on T2-weighted sequences. Lesions typically involve the medial aspect of the temporal lobes and inferior frontal lobes, asymmetrically, sparing the lentiform and extending to the insula within the first 48 hours. The lesions are usually not enhanced or exhibit a minimum enhancement after gadolinium administration, and may have a hemorrhagic component. Hemorrhagic lesions can easily be detected using T1 sequences or T2 gradient-echo. The DWI sequence is more sensitive than T2 or FLAIR for the early detection of necrotizing encephalitis. At this stage, 2 different patterns in the spread can occur. In the first, the spread of water is reduced as a result of cytotoxic edema, seen as hyperintense signal on DWI and hypointensity on the ADC map, usually reflecting irreversible neuronal damage and bad prognosis. The acute phase involves areas of congestion, perivascular infiltrate, and pathologic thrombi. These changes may lead to cytotoxic edema, primarily in gray matter neurons. Therefore, the change in DWI is the most precocious cell abnormality and can confirm the acute clinical symptoms of those patients. In some patients, this sequence is the only one that is altered. The second pattern of spread may indicate a subacute phase of the disease and involves an increase in water molecule diffusion owing to vasogenic edema, with reduced congestion and perivascular infiltrate seen as areas of hypersignal in DWI and the ADC map. This stage is also accompanied by the formation of vasogenic or interstitial fluid collections, with lesions evident on T2 sequences. The evolution of the spectrum of pathologic findings from cytotoxic edema to cell lysis and necrosis causes a change in the free movement of water, similar to the pseudonormalization found in stroke. Prakash and colleagues highlighted the superiority of the T2 sequence over DWI in 2 patients with encephalitis who received MR imaging between 3 and 7 weeks after the onset of symptoms. Sener reported 2 patients with simultaneous patterns of cytotoxic and vasogenic edema and suggested that the cytotoxic edema indicated fulminant necrosis and poor prognosis. However, an understanding of all the mechanisms involved in the different stages of development of herpes simplex encephalitis still requires more detailed studies with larger and more representative samples. It is possible that very early diagnosis and the institution of appropriate therapy enable effective treatment, preventing irreversible damage or even allowing the reversal of some changes. Differentiation from neoplastic processes can be achieved based on differences in the ADC values, which are lower in herpes lesions than in normal parenchyma (from 0.48 × 10 −3 to 0.66 × 10 −3 ).
Herpes simplex type 2 (HSV-2) causes genital herpes and can infect the mouth and face via sexual transmission. In the CNS, HSV-2 may be transmitted from mother to child during passage through the birth canal and causes neonatal encephalitis. Outside of the neonatal period, the virus causes HSV-1-like frontotemporal encephalitis in immunocompetent patients. The imaging findings are also similar to those in HSV-1, with areas of water molecule restriction. In immunocompromised patients, the lesions are present in a more diffuse and multifocal way, with strong signals in T2 and DWI, and are difficult to differentiate from other forms of encephalitis.
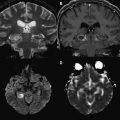
Human herpesvirus 6 (HHV-6) has 2 variants: HHV-6A and HHV-6B. Subtype B causes roseola in children, infecting virtually all children younger than 3 years. Subtype A is acquired later and displays specific neurotropic properties. HHV-6A is associated with febrile seizures, subacute and fulminant encephalitis, meningitis, meningoencephalitis, myelitis, and chronic fatigue syndrome. The cerebral infection may also selectively involve the temporal lobe, similar to limbic encephalitis, with inflammation of the uncus, amygdale, and the hippocampus body, typically sparing the parahippocampal gyrus. With the advent of DWI, characteristic findings such as irregular restriction (patchy) of diffusion may be evident before any change is visible in conventional sequences. The lesions appear hyperintense on DWI and with low ADC values in the early stages. However, follow-up in patients with unfavorable outcomes revealed an increase of ADC values, representing the T2 shine-through effect owing to the development of vasogenic edema and encephalomalacia. Another entity related to HHV-6, probably of a postinfectious nature, is acute necrotizing encephalopathy. This typically presents with changes affecting the thalami, basal ganglia, cerebellar hemispheres, and brainstem. The ADC map reveals specific findings of high central signal, indicating necrosis and hemorrhage, low central peripheral signal, related to cytotoxic edema, and high signal in the adjacent tissue, suggesting perifocal vasogenic edema. This is described as a tricolor pattern ( Fig. 9 ).
Although infection by herpes simplex is the major form of viral encephalitis, other nonherpetic infections should be considered in the diagnosis of acute viral encephalitis. In immunocompromised patients, the spectrum of possibilities is even greater. Recently, the use of techniques such as DWI has provided additional information for differential diagnosis; however, the definitive diagnosis depends on the detection of viral DNA or specific serologic markers in the CSF. Among the nonherpetic viral infections, an important group of diseases are related to arbovirus, including Japanese encephalitis, West Nile encephalitis, St Louis and Murray Valley encephalitis, and dengue virus encephalitis. However, the imaging findings in these disorders are nonspecific and overlapping, which hinders the diagnosis based on an isolated evaluation of the MR imaging. Changes in imaging tests show preferences for the thalami, basal ganglia, mesial temporal lobe structures, cortex, brainstem, substantia nigra, cerebellum, and, in some cases, the cervical cord. As with other types of viral encephalitis, the DWI is useful for the detection of lesions at early stages during which conventional MR imaging appears virtually normal.
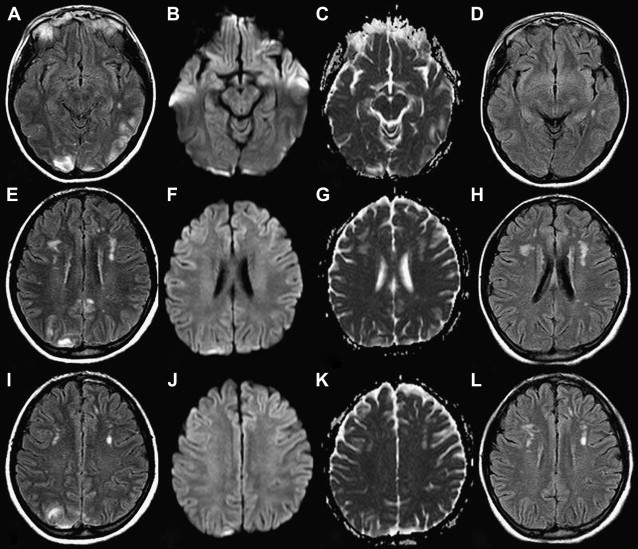
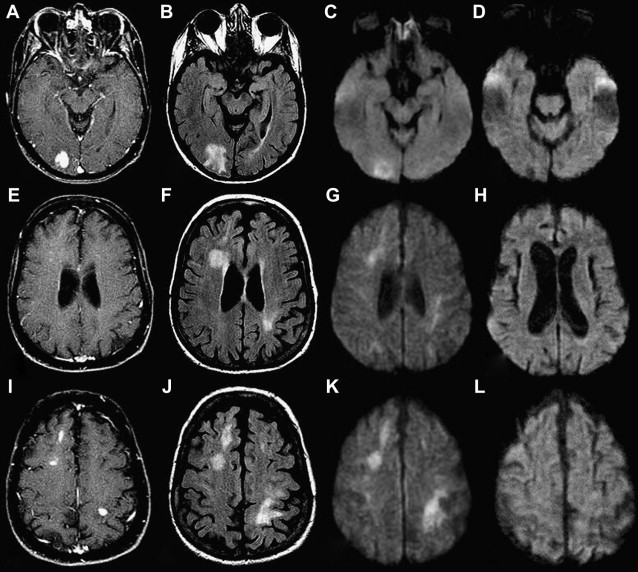
The JC virus, which has become more prevalent in recent decades with the emergence of the AIDS epidemic, causes a subacute opportunistic infection of the CNS called progressive multifocal leukoencephalopathy (PML). The virus infects the oligodendrocyte and promotes myelin breakdown with the consequent formation of infectious lesions with demyelinated substrate. The lesions are usually multifocal and can occur anywhere, most often in the parieto-occipital region. The thalami are usually affected, as are the cerebellum and the brainstem. On T2 sequences, the lesions are patchy, scalloped, and feature a high signal intensity in the white matter and extending along the white fibers that tend to cross through the splenium of the corpus callosum. PML also features the involvement of subcortical regions, minimum expansive effect and, rarely, thin peripheral enhancement. The evaluation of these lesions by diffusion-weighted sequence has proved to be a useful method of evaluating and monitoring the disease, as well as establishing differential diagnosis. The patterns of lesions in the diffusion-weighted sequence depend on the stage of the lesion. Acute lesions or the margins of large lesions (leading edges) show reduced ADC values and hypersignal on DWI. Advanced lesions and the central regions of large lesions have a high ADC and consequently low signal on DWI ( Fig. 10 ). Histopathological examination shows that the extended extracellular space is enlarged, with sparse oligodendrocytes and macrophages in the central region (where the ADC is high) and myelin loss and enrichment in the number of macrophages and oligodendrocytes with intranuclear inclusions in the periphery of the lesion. Usiskin and colleagues have demonstrated the effectiveness of the diffusion-weighted sequence by following a patient treated with HAART (highly active antiretroviral therapy regimen). After 6 months of treatment with good clinical evolution, the DWI showed less hypointensity of the central signal, with a significant decrease in ADC values and an absence of the peripheral hyperintensity signal observed in the first examination, notably with the use of a b-value of 3000.