Diffusion-weighted imaging has been used extensively in clinical practice for the early diagnosis of central nervous system conditions that restrict the diffusion of water molecules because it provides information about tumor cellularity or abscesses containing viscous fluid. DTI can detect brain lesions before any conventional imaging. Even though the role of these modalities is well defined for many neurologic lesions that affect the brain, its clinical application in spinal cord diseases is increasing. This article discusses the several central nervous system conditions that may be diagnosed with diffusion imaging.
Diffusion describes the spread of particles through random motion, also called Brownian motion. Diffusion sensitization imaging was first introduced in the mid-1960s by Stejskal and Tanner and was first used in the clinical realm in the mid-1980s by Le Bihan and colleagues. In diffusion-weighted imaging (DWI), each voxel has an intensity that reflects the single best measurement of the rate of water diffusion at that location. DWI has been used extensively in clinical practice for the early diagnosis of central nervous system (CNS) conditions that restrict the diffusion of water molecules, as in areas of cytotoxic edema observed in infarction and related conditions. It also provides information about tumor cellularity or abscesses containing viscous fluid. Diffusion tensor imaging (DTI) is actually a mathematical description (ie, the tensor) and is useful when tissue has an internal structure that creates barriers to water motion. For example, the neural axons and myelin sheath allow water molecules to diffuse preferentially along their length. In some cases, DTI can detect brain lesions before any conventional imaging. Tractography gives directional information that can be exploited at a higher structural level to select and follow neural tracts through the brain. This modality is used mainly in planning surgery for tumors and to assess white matter integrity in various other pathologic conditions.
Ischemic CNS lesions
Stroke
Stroke involves a rapid onset of neurologic impairment and is the leading cause of adult morbidity and mortality in the developed world. The major cause of stroke is arterial ischemic impairment, followed by intracranial aneurysm rupture and hemorrhage. Stroke is an urgent health issue because the sooner the patients are treated the less brain damage occurs. Imaging studies play a central role in the initial evaluation of patients who have had a stroke.
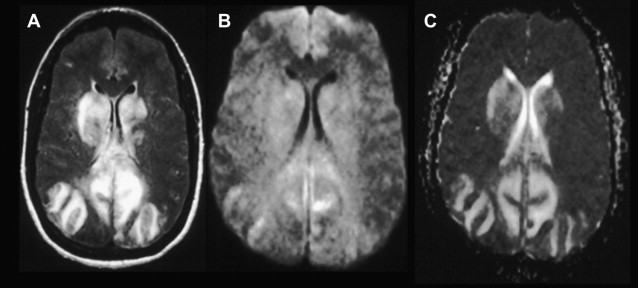
Nonenhanced computerized tomography (NECT) is an accessible and rapid technique that is usually the first to be performed in suspected cases of acute stroke. NECT detects hemorrhages and other conditions that mimic symptoms of stroke and typically reveals a cortical-subcortical hypodense area within a vascular territory. Conventional MR imaging may depict an acute and subacute infarct as a hypointense area on T1-weighted imaging (WI) and a hyperintense area on T2-WI, but it fails to differentiate between acute stroke and other lesions ( Fig. 1 ). However, DWI has the best sensitivity and specificity for the diagnosis of stroke.
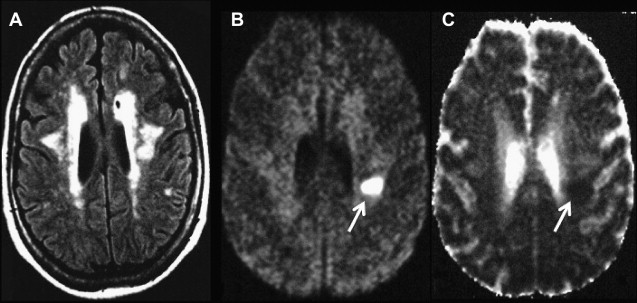
Acute stroke causes cytotoxic edema, which decreases water molecule diffusion, leading to a hyperintense area on DWI compared with normal brain tissue. To interpret the diffusion-weighted images, it is important to correlate them with apparent diffusion coefficient (ADC) maps, which should show the region as a dark area when true restriction occurs ( Fig. 2 ). Abnormalities can be seen as a reduced ADC as early as 30 minutes after the onset of ischemia, which decreases to a minimum ADC at 3 to 5 days and then increases to baseline levels by 1 to 4 weeks. This evolution is caused by vasogenic edema and further gliosis, leading to increasing extracellular water content. Some areas of moderately low ADC (<15% of normal) escape from infarction, a phenomenon known as DWI reversal.
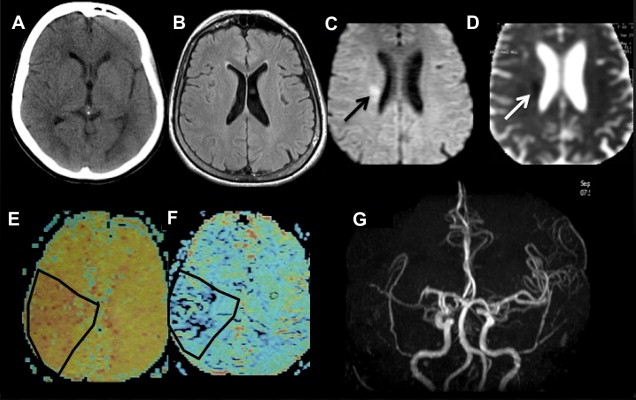
While DWI is useful to identify irreversibly infarcted tissue, perfusion-weighted MR imaging is capable of identifying areas of reversible ischemia by quantitative and qualitative evaluations of cerebral blood volume, cerebral blood flow, and mean transit time. Cerebral tissue has a vascular autoregulatory mechanism that, in the context of ischemia, causes a hypoperfused peripheral area (ie, decreased blood flow) with no DWI abnormalities, indicating that there is a potential to rescue the affected brain area. The ischemic area surrounds a central core of irreversible ischemia that has both decreased blood volume and restricted diffusion. This mismatch area is called penumbra, and when it occurs, thrombolytic therapy should be considered.
To summarize, DWI is an important tool for diagnosing and evaluating acute ischemic events. Further studies have been developed to determine the ideal selection of patients for thrombolytic treatment based on imaging data rather than on the time of stroke onset alone.
Posterior Reversible Encephalopathy Syndrome
Posterior reversible encephalopathy syndrome (PRES) is a neurotoxic state that occurs in several complex conditions (eg, chemotherapy, autoimmune disease, organ and bone marrow transplants, and preeclampsia/eclampsia). PRES has a unique pattern of brain vasogenic edema, often widespread, but predominating in parietal and occipital regions. On an ADC map, patients with PRES show areas of high signal intensity, indicating vasogenic edema. Such vasogenic edema might be expected to cause decreased signal intensity on DWI relative to the surrounding brain. In reality, however, DWI findings are most often remarkably normal despite obvious abnormalities on conventional MR imaging and ADC maps ( Fig. 3 ). These areas of edema usually reverse completely, following the prompt treatment. Focal areas of restricted diffusion are uncommon and may be associated with an adverse outcome.