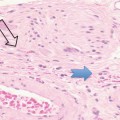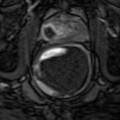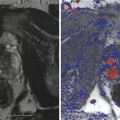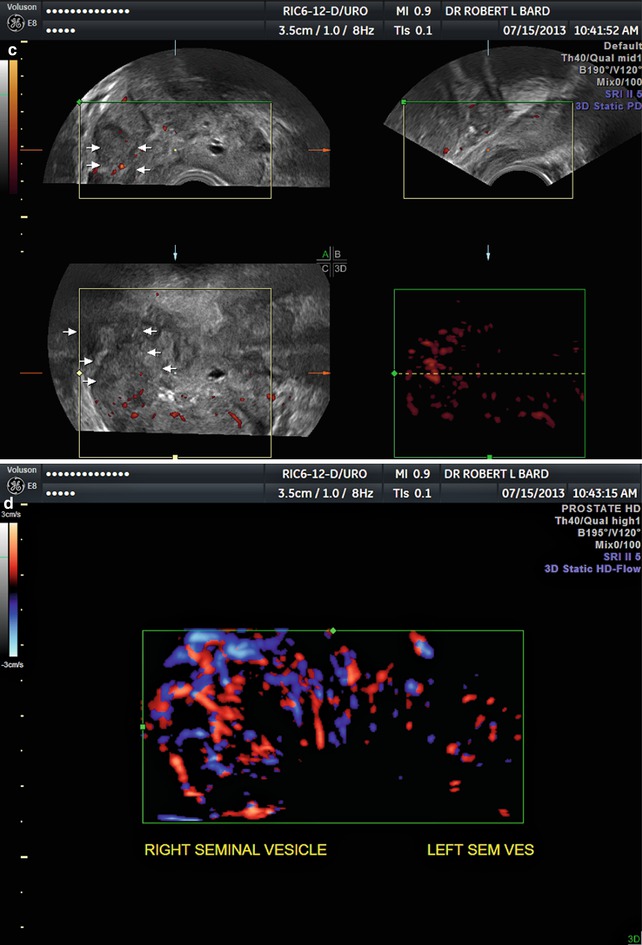
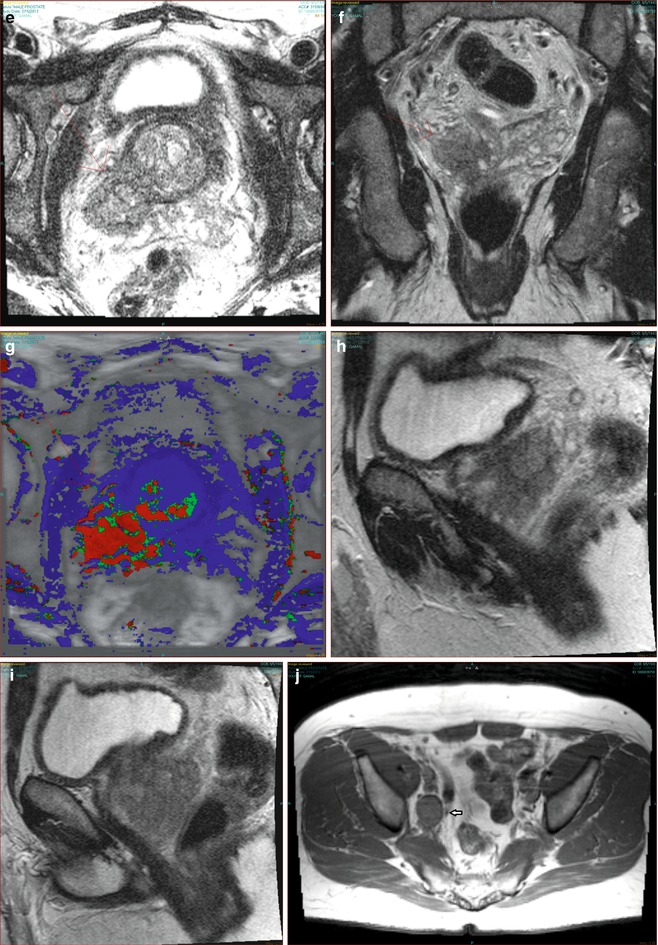
Fig. 9.1
(a) 3D patient with Gleason 7 shows dilated right seminal vesicle. (b) 3D coronal view shows direct invasion. (c) 3D coronal view shows lateral indirect invasion. (d) 3D Doppler confirms vascular invasion. (e) MRI shows indirect invasion. (f) Coronal MRI shows direct invasion. (g) DCE-MRI confirms invasion. (h) Sagittal MRI confirms direct invasion. (i) Sagittal MRI confirms indirect invasion. (j) T1 MRI shows right obturator lymph node. (k) T2 MRI shows right obturator lymph node. (l) Diffusion MRI shows right obturator lymph node
DWI is extensively covered in many chapters of prostate imaging as highly effective in both anatomic verification and grading of prostate tumors; however, DWI does not appear to accurately differentiate malignant tissue from benign prostatic hyperplasia (BPH) as this condition may also cause areas of restricted diffusion in the central parts of the prostate gland (Lenz et al. 2011).
9.4 WbDWI Imaging Metastases from Cancer
Metastatic disease spreads to the liver, lung, and bone hematogenously. Lymphadenopathy may be due to local invasion or by lymphatic drainage. Generally metastatic nodal disease from prostate cancer is small and usually not imaged by wbMRI. Metastatic involvement of local disease to the seminal vesicles, bladder, bowel, and pelvic side wall musculature is currently under study with this modality.
9.4.1 Liver Metastases
The tumor having the greatest metastatic potential is malignant melanoma. Indeed, clinicians would see a patient with an eye patch and enlarged liver and conclude that uveal melanoma was the etiology.
The literature on PET/CT imaging of hepatic metastases of uveal melanoma surprisingly shows poor imaging correlation, that is, metastatic disease may be easily undetected by this highly malignant disorder. A multitumor multicenter study including 11 patients with malignant melanoma studied by PET/CT and wbDWI showed a 100 % correlation by wbDWI at b = 1,000 with the 18 FDG images (Lichy et al. 2007).
Liver tumors were also evaluated by respiratory breath-holding versus respiratory-triggered imaging in a study of 92 lesions showing the mean contrast-to-noise ratio (CNR) of metastases, hepatocellular carcinomas, and abscesses was better using the respiratory-triggered approach (Kandal et al. 2009).
9.4.2 Pulmonary Metastases
The common finding of a pulmonary solitary nodule on chest x-rays leads to CT and PET/CT studies with attendant patient stress, radiation exposure, and false positives and negatives. Nodules smaller than 5 mm are likely to be benign (Goodman 2005). In a study of 54 biopsy-proven solitary nodules greater than 5 mm, malignant nodules showed a mean DWI score of 4.03 while benign nodules approached a score of 2.50 with an accuracy of 79.6 %. While useful for evaluation of large nodules, small nodules remain a diagnostic problem (Satoh et al. 2008).
9.5 Imaging Bone Metastases
Metastases prefer to site in areas of red bone marrow usually found in the axial skeleton (Scher 2003). Conventional bone scintigraphy has been used since 1970 and still is used to detect the osteoblasis in the bone matrix commonly associated with osteoblastic-forming tumors like prostate cancer. However, false-positive findings seen in degenerative disease, inflammatory disorders, and trauma degrade the sensitivity of this modality (Eustace et al. 1997). Conventional x-ray and CT show abnormal findings in the boney cortex rather than bone marrow invasion and represent late-stage disease.
MRI has been used for two decades to detect marrow disease; however, findings often lack specificity and 18F PET/CT has been improving accuracy (Bard 2009). WbDWI provides anatomic and functional imaging of solid tumors that experience restricted diffusion possibly due to high cellular density and/or breakdown of the Na+/K+ (sodium/potassium) pump occurring from apoptosis.
WbDWI was evaluated against the current gold standard of 18F PET CT in a study of Gleason score 8 tumors. The study showed the pelvis and spine were the most common sites and there were no solitary metastases outside these locations. wbMRI showed a higher specificity and 18F PET/CT showed a higher sensitivity for detection of bone metastases from prostate cancer. False-positive findings are more common with 18F PET /CT than wbDWI since it is not tumor specific, and its uptake in bone lesions reflects elevated local blood flow in association with increased osteoblastic activity (Mosavi et al. 2012).
9.5.1 Principles of Bone Marrow Imaging
Since bone metastases cause great morbidity, a noninvasive modality is preferred. WbDWI is showing greater acceptance since it is highly sensitive to cellular density changes in the marrow space. Yellow bone marrow is low in cell density due to fatty tissue predominance, and red bone marrow has higher cell density and water content providing a higher b value in wbDWI; therefore patients with higher marrow fat content (elderly, postmenopausal women, and patients with drug-induced osteoporosis) are better candidates for DWI. Younger patients and patients receiving bone marrow stimulators are less well suited for evaluation (Padhani et al. 2013).
9.5.2 Imaging Bone Metastases from Prostate Carcinoma
Bone scintigraphy, widely used to confirm metastatic foci, has a sensitivity of 70 % and a specificity of 57 %. This has led to the preference for 18F-NaF PET/CT for confirmation; however, this lacks specificity due to a 100 % sensitivity (Even-Saphir et al. 2006).
wbMRI poorly depicts tumors in the skull and ribs; however, studies have shown that metastases outside the pelvis and spine are rare (Costelloe et al. 2012). A scientific panel at the 60th Journees Francaises de Radiologie (JFR2012, Paris) concluded that standard MRI of the pelvis and lumbar spine was sufficient screening to rule out metastatic disease to the axial skeleton.
9.6 Imaging Artifacts in wbMRI
3 T imaging has the intrinsic advantage of higher SNR which improves lesion detection. Artifacts such as dielectric effects and tissue absorption rates generally noted at 3 T are less common at 1.5 T. Eddy currents induced by the rapid switching of the magnetic gradient field with echo planar imaging cause residual magnetization that results in geometric distortion and image shearing (Koh and Collins 2007) which makes DW image alignment with T2WI more difficult. Greater B1 field inhomogeneity at 3 T fails to achieve uniform fat suppression across large fields of view causing chemical shift and ghosting artifacts. MR frequency offsets applied can differ between anatomic stations, and voxel shift can occur in the phase encoding direction producing structural misalignment (i.e., spinal nonalignment) between imaging stations. Further technical considerations may be found in the MRI scientific literature (Koh et al. 2012




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree