First decade, 1978–1987; 110 (12.8 %)
Second decade, 1988–1997; 376 (44.1 %)
Third decade, 1998–2007; 367 (43.1 %)
P value
Age (years)
46 ± 17
44 ± 15
45 ± 14
0.425
Male gender (%)
74
73
71
0.856
Familial IDCM (%)
12
18
15
0.197
Duration of HF (months ) [range]
2 [0–17]c
3 [0–13]e
0 [0–5]
<0.001 g
SBP (mmHg)
126 ± 14
124 ± 16e
127 ± 19
0.020
NYHA III–IV (%)
36c, d
23
25
0.029
Patients with previous episodes of HF (%)
87
79
66
<0.001
Anemiaa (%)
9
12
10
0.456
GFR ≤60 ml/min (%)
15
8
11
0.336
Sinus rhythm (%)
84
90
89
0.222
LBBB (%)
26
32
30
0.464
LVEF (%)
29 ± 9c
31 ± 11e
33 ± 11
<0.001
LVEDD-I (mm/m2)
39 ± 7c,d
37 ± 6e
34 ± 5
<0.001
LVEDV-I (ml/m2)
114 ± 60c
107 ± 41e
91 ± 34
<0.001
Restrictive filling pattern (%)
37e
17
<0.001 f
Moderate–severe MR (%)b
39
34
0.157f
Beta-blockers after first evaluation (%)
11c, d
82
86
<0.001
ACE inhibitors or ARBs after first evaluation (%)
34c, d
93
93
<0.001
Digitalis after first evaluation (%)
66c, d
79e
38
<0.001
Aldosterone antagonists after first evaluation (%)
8
5e
18
0.001
ICD implantation during follow-up (%)
1c, d
14
13
0.002
Time from diagnosis to implantation (months) [range]
268
129 [99–165]
22 [2–47]
<0.001 g
CRT implantation during follow-up (%)
0
6
6
0.301f
Time from diagnosis to implantation (months) [range]
151 [129–206]
23 [10–82]
<0.001 f, g
4.4 Diagnostic Criteria
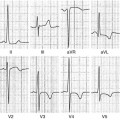
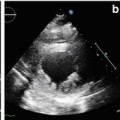
After clinical suspicion or screening, DCM is diagnosed by demonstration at imaging (typically 2D echocardiography) of LV dilatation and systolic dysfunction after excluding specific causes sufficient to determine the degree of myocardial dysfunction and dilatation, such as systemic arterial hypertension (>160/100 mmHg), coronary heart disease (stenosis >50 % of the luminal diameter in a major branch), chronic excessive alcohol consumption (>100 g/day), rapid and sustained supraventricular arrhythmias, systemic diseases, pericardial diseases, congenital heart diseases, and cor pulmonale. Clinical examination, electrocardiography (ECG) and chest X-ray radiography are not specific for DCM, whereas on echocardiography, it is possible to evaluate disease criteria.
In 1999 a collaborative European study proposed a standardization of diagnostic criteria and methods of enrollment in familial DCM. Inclusion criteria were a LV ejection fraction (EF) <45 % documented at 2D echocardiography or angiography and/or a fractional shortening <25 % at M-mode echocardiography and an LV end-diastolic diameter >117 % of the predicted value corrected for age and body surface area (BSA). Familial DCM was diagnosed in the presence of two or more affected individuals in a single family or in the presence of a first-degree relative of a DCM patient, with well-documented, unexplained SD at <35 years of age. Moreover, major and minor criteria were formulated to distinguish affected, possibly affected, and nonaffected family members (Table 4.2) [5].
Table 4.2
Major and minor criteria for diagnosing DCM
Major criteria | |
1 | LVEF 45 % (>2 SD) and/or FS <25 % (>2 SD), as ascertained by echocardiography, radionuclide scanning or angiography |
2 | LVEDD >117 % of the predicted value corrected for age and body surface area, which corresponds to 2 SD of the predicted normal limit +5 % |
Minor criteria | |
1 | Unexplained supraventricular (atrial fibrillation or sustained arrhythmias) or ventricular arrhythmias, frequent (>1,000 . 24 h−1) or repetitive (three or more beats with >120 beats/min−1) before the age of 50 |
2 | LVEDD >112 % of predicted value |
3 | Left ventricular dysfunction: LVEF <50 % or FS <28 % |
4 | Unexplained conduction disease: 2 or 3 atrioventricular conduction defects, complete LVBBB, sinus nodal dysfunction |
5 | Unexplained sudden death or stroke before 50 years of age |
6 | Segmental wall-motion abnormalities (<1 segment, or 1 if not previously present) in the absence of intraventricular conduction defect or ischemic heart disease |
4.5 Prognostic Stratification and Therapy
Prognosis of patients with DCM has significantly improved compared to the past, when ~50 % of affected patients died within 2 years of diagnosis [6]. In the last decade, in particular, an 8-year survival rate of >85 % was estimated in DCM, with an incidence of fewer than two major events per 100 patients per year, significantly higher than in the previous two decades [3] (Table 4.3). Many factors contributed to the improvement during this time. First is earlier diagnosis, especially when the disease is diagnosed while still in the asymptomatic phase [7]. In this sense, familial screening is an important instrument for the early diagnosis of DCM in asymptomatic patients and can impact long-term survival [4]. Therefore, a systematic familial screening with clinical interview, physical examination, ECG, and echocardiography should be performed on all probands (even in sporadic cases) and their first-degree relatives from puberty to 50 years of age.
Table 4.3
Occurrence of major events in the study population according to decade of enrolment in the Heart Muscle Diseases Registry of Trieste
First decade, 1978–1987; 110 patients | Second decade, 1988–1997; 376 patients | Third decade, 1998–2007; 367 patients |
|---|