Clinical Presentation
The patient is a 43-year-old female who presented with complaint of 8 days of right-sided upper back pain that radiates down the right arm. The patient gives a history of a left-sided disc herniation at C5-6. The right arm pain is characterized as an electric shock sensation down the medial portion of the right arm with subjective weakness. The pain is 6/10 in intensity and is exacerbated by activities such as carrying her purse or manipulating a steering wheel while driving. Over-the-counter pain medications can reduce her pain to 5/10. The patient does not recollect any history of trauma or inciting event. Upon physical examination, the patient has full strength in the deltoids, biceps, triceps, wrist extensors, wrist flexors, finger flexors, and intrinsic hand muscles bilaterally. She reports decreased sensation to pin prick in the right upper extremity in both the ulnar and median nerve distributions.
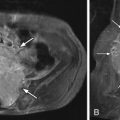
Imaging Presentation
Sagittal and axial T2-weighted magnetic resonance (MR) images were obtained and show a moderate-sized region of soft tissue signal intensity along the right posterolateral disc margin consistent with a disc herniation that compresses the right ventral aspect of the thecal sac with mild central spinal canal narrowing and severe narrowing of the right C6-7 neural foramen ( Fig. 24-1 ) .

Discussion
Cervical radicular pain caused by cervical disc herniation or spondylosis is a common cause of neck and/or arm pain. Cervical radiculopathy can also occur from many other processes including vertebral fracture, spondylolisthesis, trauma, neoplasm, infection, and metabolic conditions. A 15-year study by Radhakrishnan and colleagues of patients with cervical radicular pain concluded that the mean age at diagnosis was approximately 48 years of age. The annual age-adjusted rates per 100,000 were 83.2 for the total, 107.3 for males, and 63.5 for females. The male to female ratio was 1.7. A history of trauma immediately preceding the onset of radicular pain was seen in 14.8% of patients. The duration of symptoms before diagnosis had a mean of 40.6 days. The onset of symptoms was acute in 50%, subacute in 24%, and insidious in 26%. Neck and arm symptoms occurred in nearly all patients (97.5%). Subjective weakness was present in only 15% of patients. Symptoms were unilateral in 98% of the patients. Pain with neck movement occurred in 90% of patients. The most common etiologies of the radicular pain found at surgery were spondylosis, disc herniation, or a combination in 68.4% and a disc protrusion in 21.9%. The age- and gender-specific annual incidence rates of cervical disc herniation causing radicular pain was greatest in the 50 to 54-year-old age group and rapidly declined after 60 years of age. A similar large review of patients with cervical radicular pain by Henderson and colleagues demonstrated arm pain in 99.4%, sensory deficits in 85.2%, neck pain in 79.7%, reflex deficits in 71.2%, motor deficits in 68%, scapular pain in 52.5%, anterior chest pain in 17.8%, headaches in 9.7%, anterior chest and arm pain in 5.9%, and left-sided chest and arm pain in 1.3%.
It is important to distinguish a common misuse of the terms radiculopathy and radicular pain , which are often incorrectly interchanged. “Radiculopathy is the objective loss of sensory and/or motor function as a result of conduction block or loss of axons in a spinal nerve or its roots. There are typically symptoms of numbness and weakness in the distribution of the affected nerve. Radicular pain is caused by ectopic impulse generation. Radiculopathy relates to objective neurologic signs caused by a conduction block or loss of axons. The two conditions may coexist and may be caused by the same lesion.”
The most common cause of cervical nerve root compression is narrowing of the neural foramen secondary to spondylosis, typically from uncovertebral joint spurring, osteophytes, and/or degenerative spurring of the superior facet articulation from the more caudad vertebral body. Cervical disc herniations are the second most common cause of nerve root compression in the cervical spine. The most common level of nerve root compression by any etiology is C6-7 (~50% to 70%) followed by, C5-6 (~20%), C7-T1 (~10%), and C4-5 (~5%). The most common levels of cervical disc herniation are C6-7 followed by C5-6. Disc herniations are rare at or above C3-4.
Post-traumatic cervical disc herniations are rare. The vast majority of cervical disc herniations occur along with the degenerative disc cascade. Prior to the age of 20, few morphologic changes occur in the cervical disc. Around 30 years of age, there is a progressive decrease in disc hydration. The cervical disc becomes more compressible and less elastic. The disc loses height and begins to bulge into the spinal canal. The adjacent vertebral bodies settle closer to each other, which begins a process of osteophyte formation around the disc margin as well as the uncovertebral joints and facet joints, which can narrow the neural foramen and cause radiculopathy and radicular pain. The anatomy of the cervical disc is such that the anterior cervical annulus is very dense, but the posterior annulus has few fibers to contain the nucleus pulposus. There is also no substantive annulus over the lateral uncovertebral regions. This renders the patient with cervical discogenic degeneration susceptible to disc herniations posteriorly and laterally.
Pain is the most common finding in patients with an acute cervical radiculopathy. The pain diminishes as the condition becomes more chronic. The pain may be sharp, achy, or burning. Its location depends on which nerve root(s) are affected and can involve the neck, arm, or chest. The classic radiculopathy manifests as radiating pain in a myotomal distribution. Radicular pain is often worsened with coughing, sneezing, Valsalva maneuvers, and certain movements of the neck. Patients with high cervical disc protrusion may have nonfocal symptoms such as headache, dizziness, and tinnitus. Patients with C2-3 disc protrusions characteristically have suboccipital pain.
The Spurling test can be used to aid in the diagnosis of cervical radicular pain. The test is positive if there is reproduction of the patient’s typical pain with the Spurling maneuver (extension of the neck, rotation of the head to the side of the pain, and applying downward pressure on the head). The Spurling test has been found to be specific, but not sensitive, for cervical radiculopathy.
Selective nerve root blocks (SNRBs) can be performed both for diagnosis and therapeutic treatment. Diagnostically, SNRBs are performed if there is a question of which cervical level(s) is/are causing symptoms when imaging demonstrates more than one level of abnormality. A single-level fluoroscopically guided transforaminal SNRB with 0.3 mL of local anesthetic can help in this determination. The amount of injectate is low enough so as not to spread to adjacent levels and potentially give a false-positive result. If the test is positive, the patient should experience complete pain relief in the myotomal distribution of the injected nerve root for up to 1 hour. It is important to realize that an SNRB does not discern the cause of the radicular pain, only the level. The nerve root pain can be caused by a disc herniation, osteophyte, uncovertebral spur, or facet joint compression. Also, an SNRB blocks a portion of the facet joint, and therefore, the cause of a patient’s pain may in fact be facet-related as opposed to a compressive etiology at the neural foramen. We have found, in our institution, that inflammation of the cervical facet joint (facet synovitis) is a common cause of noncompressive radicular pain.
Imaging Features
Plain radiographic oblique views can give some information as to narrowing of particular foramen, but do not assist in the diagnosis of disc herniations. They are performed because they are inexpensive and render information about sagittal balance, instability, fractures, and congenital abnormalities. Neural compression by disc herniation or osteophyte can be indirectly diagnosed with myelography ( Fig. 24-2 ) ; however, there are many occasions when it is difficult to distinguish between an osteophyte alone compressing the thecal sac or a combination osteophyte/disc complex. The most common cause of an extradural defect on the thecal sac is a disc herniation, osteophyte, or a combination of the two.