Clinical Presentation
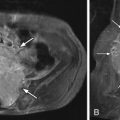
The patient is a 65-year-old male with a 2-year history of progressive right thigh pain radiating down the lateral aspect of the right leg. The pain is exacerbated by walking but also present when sitting. The patient walks with a limp. Straight leg raising sign is negative. There is a diminished right knee jerk ( Figs. 21-1 and 21-2 ) .

Imaging Presentation
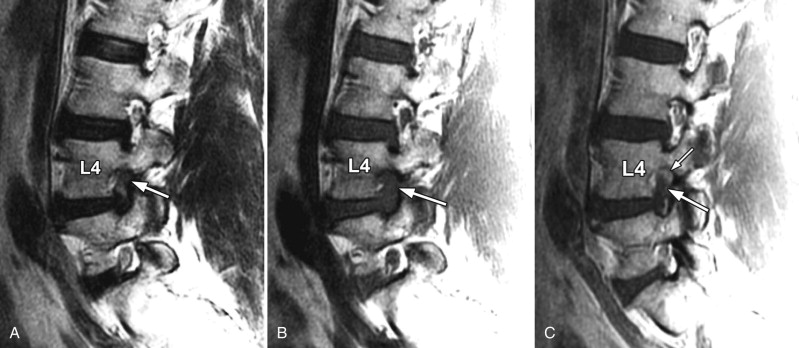
Magnetic resonance (MR) imaging of the lumbar spine reveals a large herniated disc extending into the right L4-5 neural foramen obscuring the intraforaminal fat adjacent to the right L4 nerve root. Subtle contrast enhancement is demonstrated adjacent to the nonenhancing intraforaminal disc fragment.
Discussion
Foraminal or extraforaminal disc herniations comprise approximately 10% of lumbar disc herniations. The L4 nerve root is most commonly involved. Foraminal disc herniations tend to occur in older patients, often with little evidence of disc degeneration. Posterolateral vertebral osteophytes and facet hypertrophy may contribute to the neural foraminal stenosis associated with foraminal disc herniation. The predisposing factors for lateral disc herniations are similar to other lumbar disc herniations. (Refer to discussion in Chapter 17 on lumbar disc herniation).
With foraminal or far lateral (extraforaminal) disc herniations, characteristic clinical findings are related primarily to radiculopathy in the distribution of the involved nerve root. The radicular pain with foraminal and extraforaminal disc herniations may be extremely intense, which is believed to be due to compression of the dorsal root ganglion. The pain is often located in the groin or anterior thigh, but may radiate more distally in the lower extremity. The pain may be accentuated by lateral bending. Low back pain may be present but is frequently absent or less severe than the radicular pain. The patient may experience dysesthesias or sensory loss. The knee jerk may be absent. A positive straight-leg raising sign is often present.
Imaging Features
Herniated discs that extend into the neural foramen (intervertebral foramen) usually are not detected by myelography alone, because they cause minimal or no root pouch deformity and therefore require computed tomography (CT) or MR for imaging detection ( Figs. 21-1 to 21-7 ) . Foraminal and extraforaminal (far lateral) disc herniations are not uncommonly overlooked even when CT and MR imaging studies are interpreted.





Lateral disc fragments compress the nerve roots as they course below the pedicle at a given lumbar disc level. For example, a lateral disc herniation at the L4-5 level will produce L4 radiculopathy, whereas a posterolateral disc herniation compressing the thecal sac at the same level causes L5 radiculopathy. A foraminal disc herniation may be visible on CT as an isointense or slightly hyperintense mass within the neural foramen (see Fig. 21-3 ). MR imaging has advantages over CT for detection of lateral disc herniation. The foraminal disc herniation is usually well demonstrated on axial T1-weighted images, which show excellent contrast between the disc material and the fat (see Figs. 21-1 to 21-6 ).On MR imaging, the foraminal disc herniation is usually contiguous with the parent intervertebral disc, a finding that is best demonstrated on parasagittal MR images obtained through the neural foramen (see Figs. 21-1 and 21-4 ). The parasagittal T1-weighted or T2-weighted Spin Echo (SE) MR images obtained through the foramen are also valuable for assessing the degree of nerve root compression (see Figs. 21-1 and 21-4 ). The herniated disc fragment typically does not enhance, but enhancement is nearly always demonstrated along the margin of the intraforaminal disc fragment (see Figs. 21-6 and 21-7 ).
Most foraminal and extraforaminal disc (far lateral) herniations tend to have a wide base where they extend beyond the vertebral body margin, and therefore the majority of foraminal disc herniations are disc protrusions by definition (see Figs. 21-5 and 21-6 ). However, lateral and far lateral foraminal disc extrusions also occur. Double disc fragments can also occur in the neural foramen or lateral to the neural foramen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree