Clinical Presentation
The patient is a 37-year-old man who presented with low back and right leg pain. He underwent a right L5-S1 microdiscectomy. He did well for about 5 years, but then developed recurrent symptoms. He currently describes right leg pain and numbness radiating down to the foot greater than low back pain. The pain is 60% in the right leg and 40% in the low back. There is no left leg pain or acute change in bladder function. Pain score ranges from 3/10 to 8/10. Straight leg raise is positive at 60 degrees on the right and negative to 90 degrees on the left.
Imaging Presentation
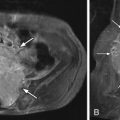
Axial T1-weighted pre-contrast and post-contrast magnetic resonance (MR) images at the L5-S1 level reveal a focal region of soft tissue along the right posterolateral aspect of the disc with peripheral enhancement. These findings are consistent with a recurrent disc herniation with surrounding granulation tissue in a patient with a previous right-sided laminectomy. The disc herniation causes posterior displacement of the traversing right S1 nerve root ( Fig. 23-1 ) .
Discussion
Surgery for lumbar disc herniation is successful in 75% to 92% of patients. This leaves 8% to 25% of patients with residual or recurrent low back pain and/or radicular pain. The success of a second operation depends on whether the initial surgical indication was correct and what the diagnosis is currently. The causes of failure include insufficient disc removal including sequestered disc, wrong site surgery, unrecognized second disc herniation, recurrent disc herniation, epidural fibrosis/scar, arachnoid adhesions, and traumatic injury to a nerve root. Recurrent herniations have been reported in 5% to 11% of patients and are therefore a major cause of surgical failure. If the residual/recurrent pain is due to a retained or recurrent disc herniation, then these patients tend to show improvement with a second operation with a percentage showing improvement similar to that after a primary surgical procedure. If, however, the surgical failure is due to scar formation, then these patients tend to show little improvement. It has been suggested that the annulotomy created during the surgical procedure weakens the disc and that it is thereafter more susceptible to recurrent disc herniations. Disc herniations are usually ipsilateral to the annulotomy; however, up to 34% of patients have contralateral disc herniations. Risk factors associated with recurrent disc herniations include young age, male gender, smoking, and traumatic events, particularly sports-related activities and lifting.
The distinction between recurrent disc herniation and scar formation has been attempted with myelography, unenhanced computerized tomography (CT), enhanced CT, CT/discography, unenhanced magnetic resonance imaging (MRI), and enhanced MRI. Benoist and colleagues demonstrated that myelography was not sensitive or specific for the differentiation of recurrent disc herniation and scar. Braun and colleagues showed that enhanced CT was more sensitive than unenhanced CT. Prior to the advent of MRI, CT was the study of choice to evaluate the postoperative spine. Studies comparing enhanced CT imaging with unenhanced MR imaging evaluating the accuracy of diagnosing recurrent disc herniation versus scar demonstrated the superiority of MR imaging. MRI had a 79% accuracy for diagnosing scar and a 97.8% accuracy for recurrent disc herniation compared with CT’s 42.2% accuracy in the diagnosis of scar and 71% accuracy for recurrent disc herniation. Furthermore, enhanced CT requires a large volume of iodinated contrast and is only able to scan one level of the spine at a time. MRI does not have these drawbacks, and therefore MRI has become the preferred method in the evaluation of recurrent disc versus scar formation. A study by Bernard demonstrated that CT/discography was more sensitive than enhanced MRI in predicting recurrent disc herniation. However, discography is an invasive procedure with significant risks to the patient, and therefore is not considered a preferred method in evaluation of recurrent disc herniation.
MRI, in patients without contraindications to MRI, has replaced other imaging modalities in the evaluation of the postoperative back. The differentiation of recurrent disc herniation and scar tissue is predicated on the fact that scar tissue enhances because it has a blood supply, a fenestrated capillary endothelium, and an extravascular space. Disc material does not have a blood supply. Instead, contrast diffuses into the cartilaginous disc fragment. Scar tissue enhances maximally soon after injection of contrast and then begins to decrease 20 minutes after injection. Disc material demonstrates mild continuous enhancement over the first 45 minutes after injection, although enhancement is always less than that of adjacent scar tissue.
Studies have also suggested the utility of unenhanced MRI in the determination of scar tissue versus recurrent disc herniation. Hueftle and colleagues reported 100% sensitivity, 71% specificity, and 89% accuracy of unenhanced MRI with 100% sensitivity, specificity, and accuracy after the administration of contrast media. Mullin and colleagues evaluated postoperative patients with noncontrast MRI and obtained the correct diagnosis in 90% of cases. In the other 10% of the cases (nine patients) contrast was administered and three diagnoses were unchanged, two diagnoses were improved, and four diagnoses were made worse. The criteria used to diagnose recurrent disc herniation were based on signal characteristics and morphology. In the abstract of a study by Hochhauser and colleagues, “the most reliable MR sign for recurrent herniated disk was the presence of a sharply marginated focal polypoid disk protrusion beyond the posterior margins of the adjacent vertebral bodies shown to best advantage on sagittal T1- and T2-weighted and axial T1-weighted spin-echo MR images. Disc herniations usually maintained isointensity with the intervertebral disc of origin, while extradural fibrosis exhibited variable signal intensity. The preoperative diagnosis of extradural fibrosis on MR was based primarily on its irregular configuration and extension.” Other morphologic features that suggest scar include the absence of mass effect upon the thecal sac, absence of continuity with the parent disc, and retraction of the thecal sac at the level of the soft tissue mass. These authors suggest that suspected recurrent disc herniation could be evaluated with noncontrast MR examination and that contrast could be “reserved for difficult or unresolved cases.”
The intervertebral disc, as well as other cartilage, has a large amount of glycosaminoglycans, which have fixed negative charges. These negative charges slow the diffusion of charged particles or ions through the cartilage. Therefore, in principle, a paramagnetic contrast agent that has a charge should diffuse less readily into and through a disc as opposed to a contrast agent without a charge. Experiments have demonstrated that ionic contrast media diffuses through an intervertebral disc less well than a nonionic contrast medium. In animal and human studies, discs enhanced twice as much using nonionic contrast media versus ionic media. Therefore, if a patient is being evaluated for recurrent disc herniation, it is more appropriate to choose an ionic contrast agent so that surrounding scar tissue is maximally enhanced and disc material is minimally enhanced.
Another method of separating recurrent disc herniation from scar tissue is through adjusting the dose of paramagnetic contrast. A concentration of 0.1 mmol/kg is typical for post-contrast imaging. Scar tissue is better enhanced at a concentration of 0.3 mmol/kg and is more clearly separated from a recurrent disc herniation than at 0.1 mmol/kg. One has to weigh the slightly added benefit of additional contrast versus cost and the potential toxic effects of higher doses of gadolinium.
Lastly, over time, a disc herniation becomes vascularized. Scar tissue, over time, decreases in its enhancement. It is possible that if a patient waits to get imaged a few months after a disc herniation that it may be impossible to see a difference between scar tissue and disc herniation.
It appears that the best way to distinguish between scar tissue and disc herniation is with MR imaging using ionic paramagnetic contrast, preferably but not necessarily at a higher concentration, and within a few days to weeks of the beginning of symptoms.
Imaging Features
Recurrent Disc Herniation
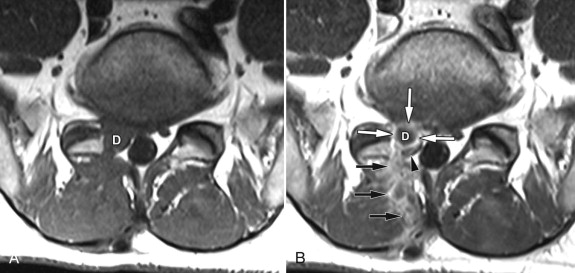
A recurrent disc herniation has many of the same imaging characteristics of a nonoperated disc herniation. With CT imaging, the recurrent disc herniation will be seen as a mass-like region of soft tissue attenuation, similar to the parent disc, usually ventral or ventral lateral in location that may be connected with the parent disc ( Fig. 23-2 ) . There may be a decrease of complete obliteration of the normal epidural fat. If contrast is given, there may be peripheral enhancement around the disc herniation because of scar tissue. On MRI, the recurrent disc herniation will be isointense to the parent disc unless the fragment is calcified, in which case it would be of low T1 signal intensity ( Fig. 23-3, A ) . The disc herniation is isointense to hyperintense on T2-weighted sequences ( Fig. 23-3, B ) . The disc material will demonstrate no to minimal enhancement if imaged within the first 20 minutes after intravenous injection. There may be peripheral enhancement around the disc and in the laminectomy defect secondary to vascularized scar tissue (see Figs. 23-1, B , and 23-3, C ).