Clinical Presentation
The patient is a 75-year-old female who has presented with mid and low back pain and report of numbness and tingling in both legs for the past 4 weeks. The patient was on a three-step ladder putting away some dishes when she lost her balance and fell on her back. She was initially only sore from her fall; however, her back pain did not subside over the next several days, and she began to feel numbness and tingling in both legs that did not change character with a change in position. She has been incontinent of urine twice over the last 2 weeks and feels she is unsteady on her feet.
Imaging Presentation
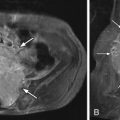
Axial and sagittal reformatted computed tomography (CT) images of the thoracic spine demonstrate a calcified mass along a left posterior paramedian midthoracic disc, which impresses the left ventrolateral aspect of the thecal sac and displaces it to the right compatible with a calcified herniated disc ( Fig. 25-1 ) .
Discussion
Thoracic disc herniations are rare when compared with lumbar and cervical herniations. Most series report an incidence of thoracic disc herniations in less than 2% of all operated discs and symptomatic disc herniations composing less than 1% of spinal disc herniations. Autopsy studies have demonstrated an incidence of thoracic disc herniations of 7% to 15%. It has been postulated that the low incidence of thoracic disc herniation is related to the limited mobility of the thoracic spine secondary to the small size of the thoracic discs, the restraint placed on the thoracic spine by the ribs, and the coronal orientation of the thoracic facet joints. Most thoracic disc herniations are reported in the lower thoracic spine, with T11-12 being the most common; 75% of all thoracic disc herniations occur below the T8 level. Most surgical series demonstrate thoracic disc herniations to be central or paramidline and less likely posterolateral or lateral. Multilevel disc herniations have been reported with an incidence of less than 5% of all patients. Most studies show an equal distribution of thoracic disc herniations between men and women. Degenerative changes are likely the most common cause of thoracic disc herniations.
The role of trauma as a cause of thoracic disc herniations has been widely debated. Most series demonstrate trauma to not be a significant etiology of thoracic disc herniations, whereas others disagree and believe that the trauma may have been minor or too far in the past for the patient to recall. One study demonstrated that men under the age of 40 had a 53% incidence of traumatic disc herniation, whereas all others had a 17% rate. This suggests that younger men are a distinct group in regard to incidence of thoracic disc herniation.
Thoracic disc herniations can be difficult to diagnosis clinically because there are a myriad of clinical presentations. Unlike cervical or lumbar disc herniations where pain may be associated with an extremity, thoracic disc herniation pain may have vague symptoms that could easily be confused with cardiac, pulmonary, gastrointestinal, or genitourinary disorders. Patients with a lateral disc herniation at the C7-T1 or T1-2 level may present with Horner’s syndrome. A disc herniation in the mid or lower thoracic spine can present as a Brown-Séquard syndrome or anterior spinal artery syndrome. A disc herniation at the thoracolumbar junction could present with a conus medullaris syndrome. Patients have incorrectly had abdominal surgery to alleviate their pain.
However, most often, the patient demonstrates typical signs and symptoms of disc herniation. If the patient has a foraminal or lateral disc herniation, he or she will have back and radicular pain. If the patient has a central disc herniation, he or she may have pyramidal tract signs. The patient may describe decreased sensation over a dermatomal level. The patient may demonstrate decreased abdominal and/or anal reflexes.
It is extremely important, in the thoracic region, to make sure the imaging level is well defined. The thoracic spine has no good landmarks, as there are in the cervical or lumbar regions, and therefore a wrong level surgery could occur. It is important to have a sagittal scout image that extends either from C2 through the thoracic spine or a scout image that includes the lumbosacral junction. Although exact counting is preferred, the key is for the surgeon or interventionalist to understand what level(s) the radiologist is describing.
Imaging Features
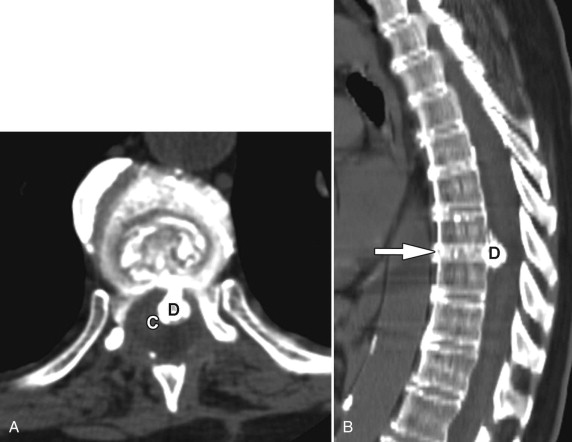
Plain film radiography cannot be used to diagnosis a thoracic disc herniation; however, radiographs can show intervertebral disc calcification, which is more common in people with thoracic disc herniations than in the normal population. On CT, the disc herniation is often contiguous with the intradiscal calcification ( Fig. 25-2 ) . Some believe that the intradiscal calcification is calcification along a radial fissure similar to radial fissures seen with lumbar discography. However, a normal thoracic radiograph does not preclude a thoracic disc herniation. Myelography without CT can demonstrate the mass effect that a disc herniation may have on a contrast-filled thecal sac resulting in central spinal stenosis or a nerve root amputation sign secondary to a foraminal soft tissue abnormality; however, the findings on myelography are not specific to disc herniations. Any extradural soft tissue mass can result in similar myelographic findings. Furthermore, myelography is more invasive than either CT or magnetic resonance imaging (MRI). A CT scan after myelography is more sensitive and specific for thoracic disc herniations ( Fig. 25-3 ) .