2 Disorders of the Airways Increase in transradiancy of a lung field. One of several causes may be involved: Primary congenital pulmonary artery hypoplasia CT. Hypertransradiant hemithorax with hypoperfusion Depend on the cause Depend on the cause. Asymptomatic incidental finding in MacLeod/Swyer–James syndrome and in pulmonary artery hypoplasia Depend on the cause and/or underlying disorder. Depend on the cause and/or underlying disorder. Determine the cause and specifically exclude a tumor.
Hypertransradiant Hemithorax
Definition
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
 MacLeod/Swyer-James syndrome, i.e., hypoplasia of pulmonary parenchyma including the territory of the pulmonary artery secondary to viral infection in the first 8 years of life prior to complete maturation of the lung
MacLeod/Swyer-James syndrome, i.e., hypoplasia of pulmonary parenchyma including the territory of the pulmonary artery secondary to viral infection in the first 8 years of life prior to complete maturation of the lung  Perfusion defect from reflex vasoconstriction where a central bronchial obstruction (central bronchial carcinoma, bronchial adenoma, or endobronchial foreign body) creates a ventilation defect.
Perfusion defect from reflex vasoconstriction where a central bronchial obstruction (central bronchial carcinoma, bronchial adenoma, or endobronchial foreign body) creates a ventilation defect.
Imaging Signs
 Modality of choice
Modality of choice
 Radiographic findings
Radiographic findings
 Signs of hyperinflation in the presence of a central bronchial obstruction.
Signs of hyperinflation in the presence of a central bronchial obstruction.
 CT findings
CT findings
 Pulmonary artery hypoplasia: Hypoplastic pulmonary arterial system with otherwise normal parenchymal texture
Pulmonary artery hypoplasia: Hypoplastic pulmonary arterial system with otherwise normal parenchymal texture  MacLeod/Swyer–James syndrome: Mixed picture with hyperinflated and normally inflated areas, bronchiectatic tissue remodeling with thickened bronchi in collapsed, scarred lung segments
MacLeod/Swyer–James syndrome: Mixed picture with hyperinflated and normally inflated areas, bronchiectatic tissue remodeling with thickened bronchi in collapsed, scarred lung segments  Central bronchial carcinoma with bronchial and/or pulmonary artery obstruction
Central bronchial carcinoma with bronchial and/or pulmonary artery obstruction  Endobronchial obstruction due to tumor or foreign body.
Endobronchial obstruction due to tumor or foreign body.
 Pathognomonic findings
Pathognomonic findings
Clinical Aspects
 Typical presentation
Typical presentation
 Symptomatic in tumor cases.
Symptomatic in tumor cases.
 Therapeutic options
Therapeutic options
 Course and prognosis
Course and prognosis
 What does the clinician want to know?
What does the clinician want to know?
Differential Diagnosis
MacLeod/Swyer–James syndrome | – CT shows a mixed picture with hyperinflated and normally inflated areas – Bronchiectatic tissue remodeling with thickened bronchi in collapsed, scarred lung segments |
Pulmonary artery hypoplasia | – More common on the left than right; hypoplastic pulmonary artery system – Hemithorax smaller on the affected side – No air trapping |
Central bronchial carcinoma | – Tumor ventilation defect with perfusion defect from reflex vasoconstriction – Paradoxical hilus sign |
Endobronchial tumor (bronchial adenoma) | – Tumor ventilation defect with perfusion defect from reflex vasoconstriction – Hyperinflation with valve mechanism; CT shows endobronchial mass blocking the lumen |
Foreign body aspiration | – Ventilation defect from foreign-body aspiration with perfusion defect from reflex vasoconstriction – Hyperinflation with valve mechanism – Air trapping – History; CT shows endobronchial foreign body |
Tips and Pitfalls
Can be confused with off-center grid, post-mastectomy, and unilateral atrophy of the pectoralis muscles.
Selected References
Lucaya J et al. Spectrum of manifestations of Swyer-James-MacLeods syndrome. J Comput Assist Tomogr 1998; 22: 592–597
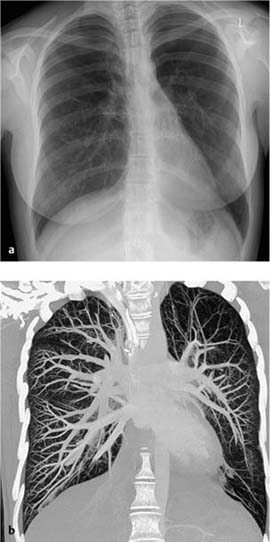
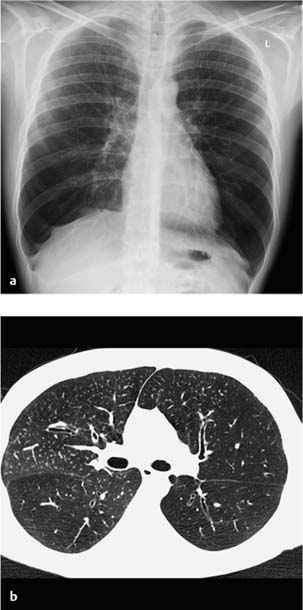
Fig. 2.1 Hypertrans-radiant hemithorax (MacLeod/Swyer–James syndrome) in an 18-year-old woman. The plain chest radiograph (a) shows increased transradiancy of the left lung with significantly diminished vascularity. The coronal slices (b – d) clearly demonstrate diminished vascularity (b, MIP), shrinkage (c), and bilateral bronchi-ectasis (d).
Bronchiectasis
Definition
Irreversible dilation of a bronchus or bronchi, especially large and small subsegmental bronchi  Reid classification differentiates cylindrical, varicose, and cystic dilation.
Reid classification differentiates cylindrical, varicose, and cystic dilation.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Congenital (Kartagener syndrome, mucociliary dysfunction, cystic fibrosis, etc.)  Infectious (allergic bronchopulmonary aspergillosis, measles, whooping cough, tuberculosis, etc.)
Infectious (allergic bronchopulmonary aspergillosis, measles, whooping cough, tuberculosis, etc.)  Bronchial obstruction or compression (tumor, foreign body, etc.)
Bronchial obstruction or compression (tumor, foreign body, etc.)  Pulmonary fibrosis (traction bronchiectasis) and/or thickening and inflammation of the bronchial wall
Pulmonary fibrosis (traction bronchiectasis) and/or thickening and inflammation of the bronchial wall  Destruction of the bronchial wall
Destruction of the bronchial wall  Peribronchial fibrosis.
Peribronchial fibrosis.
Imaging Signs
 Modality of choice
Modality of choice
CT.
 Radiographic findings
Radiographic findings
Nonspecific findings  Pronounced striped pattern
Pronounced striped pattern  Parallel stripes (“railroad track” sign)
Parallel stripes (“railroad track” sign)  Ring shadows.
Ring shadows.
 CT findings
CT findings
“Signet ring” sign (bronchial diameter exceeds the diameter of the accompanying artery)  Bronchi fail to taper peripherally
Bronchi fail to taper peripherally  Bronchi can be differentiated up to a subpleural depth of 1 cm
Bronchi can be differentiated up to a subpleural depth of 1 cm  Changes in bronchial contour (cylindrical bronchi appear as tracklike parallel lines, varicose bronchi as intermittent widening of the bronchial lumina or “strings of pearls,” and cystic bronchi as bunched “clusters of grapes,” because of shrinkage
Changes in bronchial contour (cylindrical bronchi appear as tracklike parallel lines, varicose bronchi as intermittent widening of the bronchial lumina or “strings of pearls,” and cystic bronchi as bunched “clusters of grapes,” because of shrinkage  Nonspecific findings include bronchial thickening, fluid or mucus-filled bronchi, loss of volume, air trapping, and nodular bronchial dilation (“tree-in-bud” sign).
Nonspecific findings include bronchial thickening, fluid or mucus-filled bronchi, loss of volume, air trapping, and nodular bronchial dilation (“tree-in-bud” sign).
 Pathognomonic findings
Pathognomonic findings
Predilection for the posterobasal segments of the lung  “Signet ring” sign and “railroad track” sign (see above)
“Signet ring” sign and “railroad track” sign (see above)  Ring shadow.
Ring shadow.
Clinical Aspects
 Typical presentation
Typical presentation
Recurrent bronchopneumonia  Voluminous expectorations
Voluminous expectorations  Hemoptysis
Hemoptysis  Dyspnea.
Dyspnea.
 Therapeutic options
Therapeutic options
Surgery (segmental resection or lobectomy)  Pulmonary toilet
Pulmonary toilet  Bronchospasmolytic
Bronchospasmolytic  Specific antibiotic therapy
Specific antibiotic therapy  Active immunization against influenza and pneumococcus.
Active immunization against influenza and pneumococcus.
 Course and prognosis
Course and prognosis
Severity correlates with the diameter of the abnormal bronchi (cylindrical bronchiectasis has the best prognosis, cystic bronchiectasis the worst).
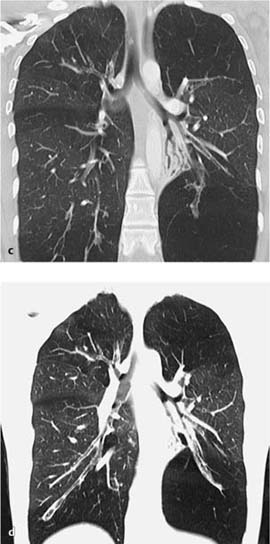
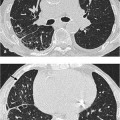
Fig. 2.2 Bronchiectasis in an 18-year-old man with immunodeficiency.
a The plain chest radiograph shows thickening of the bronchovascular bundles in the right paracardiac and left retrocardiac areas. Isolated, sharply demarcated, fine nodular densities are visible in the right lower lung field.
b On CT these changes primarily correlate with tubular bronchiectasis, occasionally concentrated, and with significant thickening of the bronchial wall and focal mucus retention.
 What does the clinician want to know?
What does the clinician want to know?
Diagnosis of bronchiectasis  Is resection of localized bronchiectatic areas indicated?
Is resection of localized bronchiectatic areas indicated?  Comorbidities detected (scarring, emphysema, abscess, empyema, broncholiths, pyemia).
Comorbidities detected (scarring, emphysema, abscess, empyema, broncholiths, pyemia).
Differential Diagnosis
Chronic bronchitis | – Involves the entire bronchial tree |
Bronchial asthma | – No productive cough |
Bullous emphysema | – No bronchial enlargement – No “signet ring” sign |
Scarring and traction | – Not a primary respiratory disease |
bronchiectasis | – Fibrotic changes in the structure of the lung |
Tips and Pitfalls
Motion artefacts on the CT due to breathing can be misinterpreted as a “railroad track” sign  Reactive bronchial dilation (“reversible bronchiectasis”) occurs in the presence of atelectasis.
Reactive bronchial dilation (“reversible bronchiectasis”) occurs in the presence of atelectasis.
Selected References
Cartier Y et al. Bronchiectasis: Accuracy of high resolution CT in the differentiation of specific diseases. AJR Am J Roentgenol 1999; 173: 47–52
King P, Song X, Rockwood K. Bronchiectasis. Intern Med J 2006; 36: 729–737
Bronchiolitis
Definition
 Epidemiology
Epidemiology
Inflammation of the peripheral respiratory bronchioles (diameter < 2 mm).
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Acutely infectious (viruses, Mycoplasma, chlamydia, aspergillosis)  Chronic inflammatory (asthma, chronic bronchitis)
Chronic inflammatory (asthma, chronic bronchitis)  Panbronchiolitis
Panbronchiolitis  Respiratory bronchiolitis (nicotine).
Respiratory bronchiolitis (nicotine).
Imaging Signs
 Modality of choice
Modality of choice
CT.
 Radiographic findings
Radiographic findings
Usually normal  Reticulonodular shadowing
Reticulonodular shadowing  Pneumonic infiltrate may be present
Pneumonic infiltrate may be present  Dystelectasis.
Dystelectasis.
 CT findings
CT findings
Centrilobular and peribronchovascular nodules  “Tree-in-bud” sign (usually peripheral)
“Tree-in-bud” sign (usually peripheral)  Ground-glass opacities
Ground-glass opacities  Bronchial wall thickening
Bronchial wall thickening  Air trapping.
Air trapping.
 Pathognomonic findings
Pathognomonic findings
None  Findings such as a mosaic pattern, “tree-in-bud” sign, or centrilobular nodules are nonspecific.
Findings such as a mosaic pattern, “tree-in-bud” sign, or centrilobular nodules are nonspecific.
Clinical Aspects
 Typical presentation
Typical presentation
Dyspnea  Nonproductive cough (productive cough occurs in diffuse panbronchiolitis)
Nonproductive cough (productive cough occurs in diffuse panbronchiolitis)  Fever.
Fever.
 Therapeutic options
Therapeutic options
Elimination of the noxious agent  Steroids (inhalational or systemic)
Steroids (inhalational or systemic)  Bronchoalveolar lavage.
Bronchoalveolar lavage.
 Course and prognosis
Course and prognosis
Prognosis is good in infections  Course is more rapid in patients with bone marrow or stem cell transplantation
Course is more rapid in patients with bone marrow or stem cell transplantation  In severe cases respiratory insufficiency andpulmonary fibrosis may develop
In severe cases respiratory insufficiency andpulmonary fibrosis may develop  Prognosis is poor in diffuse panbronchiolitis.
Prognosis is poor in diffuse panbronchiolitis.
Differential Diagnosis
Extrinsic allergic alveolitis or bronchiolitis | – No thickening of the bronchial wall – Rarely nicotine use |
Air trapping | – Extrinsic allergic alveolitis (acute stage), no bronchial wall thickening, no nicotine use – Bronchial obstruction due to foreign body or mucusretention |
Bronchiolitis obliterans with organizing pneumonia | – Nodular, usually bilateral, nonsegmental densities with air bronchogram and pleural contact |
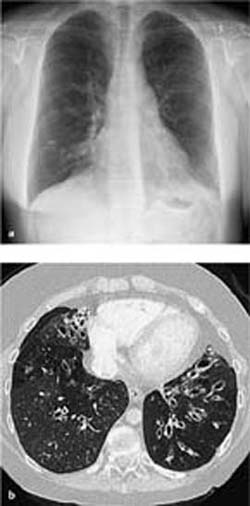
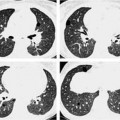
Fig. 2.3 Bronchiolitis in a 62-year-old man.
a The plain chest radiograph shows increased finely nodular shadowing, especially in the left upper field and slightly more prominent bronchial walls.
b Findings on CT are localized to the peribronchovascular region. Note the significant focal wall thickening in the small bronchi (arrowhead).
Tips and Pitfalls
False-negative diagnosis due to overlooking discrete changes.
Selected References
Hartmann TE et al. CT of bronchial and bronchiolar diseases. Radiographics 1994; 14: 991–1003
Howling SJ et al. Follicular bronchiolitis: thin-section CT and histologic findings. Radiology 1999; 212: 637–642
Müller NL, Miller RR. Diseases of the bronchioles: CT and histopathologic findings. Radiology 1995; 196: 3–12
Bronchiolitis Obliterans
Definition
 Epidemiology
Epidemiology
Depends on the etiology. Every second lung transplant recipient develops a bronchiolitis obliterans syndrome within 5 years of transplantation.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Rarely idiopathic, usually secondary to infection (mycoplasmal, viral, in children especially respiratory syncytial virus), secondary to inhalation of noxious agents, as a hypersensitivity reaction (collagen diseases), secondary to transplantation (lung, heart, bone marrow), in the setting of chronic obstructive pulmonary disease  Inflammation of the respiratory bronchioles
Inflammation of the respiratory bronchioles  Proliferation of submucosal and peribronchial tissue leading to concentric constriction of the respiratory bronchioles.
Proliferation of submucosal and peribronchial tissue leading to concentric constriction of the respiratory bronchioles.
Imaging Signs
 Modality of choice
Modality of choice
CT on inspiration and expiration (to detect air trapping).
 Radiographic findings
Radiographic findings
Signs of pulmonary hyperinflation of variable severity with diminished vascularity.
 CT findings
CT findings
Increased transparency of the pulmonary parenchyma with narrowed vessels and signs of air trapping  On expiration the density of the affected areas fails to increase
On expiration the density of the affected areas fails to increase  Affected areas show increased transparency as on inspiration
Affected areas show increased transparency as on inspiration  Mosaic perfusion
Mosaic perfusion  Peribronchiolar fibrosis (rare)
Peribronchiolar fibrosis (rare)  In postinfectious bronchiolitis there is bronchial wall thickening and bronchiectasis
In postinfectious bronchiolitis there is bronchial wall thickening and bronchiectasis  “Tree-in-bud” sign is rare.
“Tree-in-bud” sign is rare.
 Pathognomonic findings
Pathognomonic findings
Increased transparency of the pulmonary parenchyma with narrowed vessels  Severe air trapping
Severe air trapping  Mosaic perfusion.
Mosaic perfusion.
Clinical Aspects
 Typical presentation
Typical presentation
Cough  Dyspnea
Dyspnea  Fever, resembles chronic obstructive pulmonary disease but with subacute course
Fever, resembles chronic obstructive pulmonary disease but with subacute course  Primarily restrictive ventilation defect due to early complete occlusion.
Primarily restrictive ventilation defect due to early complete occlusion.
 Therapeutic options
Therapeutic options
Steroids  Immunosuppression after lung transplant.
Immunosuppression after lung transplant.
 Course and prognosis
Course and prognosis
Prognosis is good with steroid therapy.
 What does the clinician want to know?
What does the clinician want to know?
Confirmation of tentative diagnosis in at-risk patients (post bone marrow, peripheral blood stem cell, or lung transplantation).
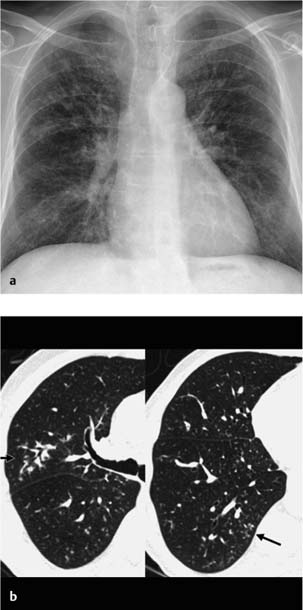
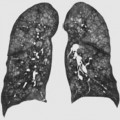
Fig. 2.4 Bronchiolitis obliterans in a 24-year-old man (graft-versus-host disease following bone marrow transplantation).
a The plain chest radiograph shows significant hyperinflation of both lungs (left more than right) with slightly more prominent bronchial walls in the perihilar region.
b CT confirms the findings and shows diminished vascularity, especially on the left side and in the right lower lobe. There was no increase in density on expiration, which is consistent with air trapping.
Differential Diagnosis
Mosaic pattern | – Constrictive bronchiolitis in graft-versus-host disease – Extrinsic allergic alveolitis (acute stage): no bronchial wall thickening, not associated with smoking – Pulmonary arterial hypertension and/or pulmonary embolism: mosaic pattern without air trapping, reduced caliber of vessels in the areas of increased transparency – Nodular ground-glass infiltrates in inflammatory lung disease |
Air trapping | – Constrictive bronchiolitis in graft-versus-host disease – Extrinsic allergic alveolitis (acute stage) – Bronchial obstruction due to foreign body, mucus plug, or tumor |
Panlobular emphysema | – Destruction of lung parenchyma – Predominantly in the basal lung segments – No mosaic perfusion |
Bronchiolitis obliterans with organizing pneumonia | – Nodular, usually bilateral, nonsegmental densities with air bronchogram and pleural contact |
Tips and Pitfalls
Generalized air trapping can escape detection, as can air trapping in an uncooperative patient (recognizable by the absence of impression of the membranous part of the trachea).
Selected References
Bankier AA et al. Bronchiolitis obliterans syndrome in heart-lung transplant recipients: diagnosis with expiratory CT. Radiology 2001; 218: 533–539
Choi YW et al. Bronchiolitis obliterans syndrome in lung transplant recipients: correlation of CT findings with bronchiolitis obliterans syndrome stage. J Thorac Imaging 2003; 18: 72–79
Hansell DM et al. Obliterative bronchiolitis: individual CT signs of small airway disease and functional correlation. Radiology 1997; 203: 721–726
Chronic Bronchitis (Chronic Obstructive Pulmonary Disease)
Definition
Pulmonary disorder characterized by increased resistance to airflow  FEV1/FVC <70%.
FEV1/FVC <70%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree