Disorders of the Ankle and Foot
Lateral
Peroneal Tendons
Tenosynovitis
In normal individuals, a small amount of fluid can often be found in the tendon sheath, distal to the tip of the malleolus, and should not be mistaken for tenosynovitis.
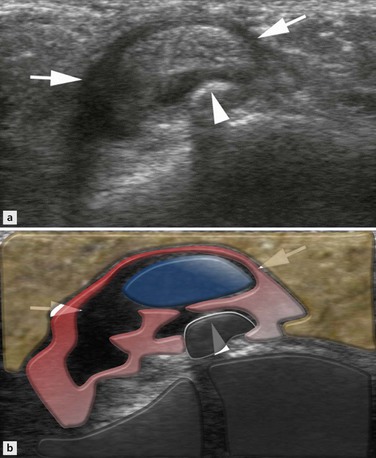
Any doubt should lead to examination of the contralateral asymptomatic side, where a similar finding can help to establish these changes as normal. In tenosynovitis the amount of fluid may vary but is generally more important and fluid surrounds the tendon transversally (‘halo sign’) (Fig. 26.1) and extends longitudinally.
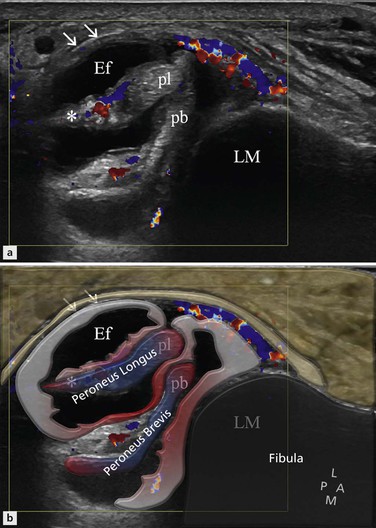
Figure 26.1 Peroneal tenosynovitis. Axial section behind the lateral malleolus. Effusion in the peroneal sheath. Thickening of the synovial wall (arrows) and mesotendon (asterisk). Hyperaemia on colour Doppler.
In patients with lateral ankle pain, colour or power Doppler examination often displays signs of hyperaemia in the synovial hypertrophic tissue, inside the tendons and/or around the tendon sheath.
Tenosynovitis may be mechanical, due to overuse or trauma, or associated with inflammatory joint diseases. Traumatic tenosynovitis is seen in patients with ankle derangement and ligament lesions, but it is important to know that effusion in the peroneal tendon sheath may just be a sign of communication to the ankle joint through an acute complete tear of the calcaneofibular ligament. Serous tensosynovitis is frequently found in patients with tendon overuse without a history of trauma, either in a sport setting or in elderly patients. Ultrasonographic signs of tendon tear should always be carefully searched for. In patients with inflammatory joint diseases, e.g. rheumatoid arthritis or gout, tenosynovitis is generally of a proliferative type with marked pannus-like synovial thickening, hyperaemia in patients with active disease, tendinopathy, irregular tendon borders, and thinning or complete tear of the tendons. Calcifications in chronic synovial sheath thickening are rare and seen as echo-rich focal areas with shadowing. They should be distinguished from a fracture of an os peroneum with retraction of the proximal tendon part behind the lateral malleolus. Tenosynovitis may also occur around an accessory peroneal bone, called the painful os peronei syndrome (Fig. 26.2).
Peroneal Tendinopathy and Tendon Tear
The configuration of the peroneus tendon varies with the severity of the lesion. With overuse, the peroneus brevis tendon can be seen as a U-shaped flattened tendon in the axial plane, with the concavity embracing the peroneus longus tendon. In more advanced stages, a partial tear of the peroneal brevis tendon appears with a longitudinal split into two tendon parts. This tendon split extends in both directions, and the peroneus longus tendon can insinuate itself between the separated parts of the peroneus brevis tendon. This appearance of three tendons within the sheath must be differentiated from the presence of an accessory tendon, the posteriorly situated peroneus quartus tendon. If there is an associated tear of the superior peroneal retinaculum, the anterior part of the peroneus brevis tendon may dislocate between the lateral malleolus and the skin. A complete axial tear of one or both peroneal tendons (Fig. 26.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree