Introduction
The most common indications for an ultrasonographic examination of the lateral aspect of the ankle are suspicion of peroneal tendon pathology or lesions of the lateral ligament complex. Patients with ligament injuries are generally examined in a chronic phase to detect late complications of ligament tears or undiagnosed associated lesions. Ultrasonography, allowing a dynamic assessment of the structures, is the best imaging modality for examination of the tendons and ligaments, but may also detect lesions of the bones (fractures) or retinacula (tendon instability). An important drawback is the inability to display osteochondral lesions of the ankle joint and tears of the interosseous ligaments (talocalcaneal).
Peroneal Tendons
Peroneal tendon pathology is frequent, especially tenosynovitis, but more significant changes like tendinopathy, tendon tears or tendon instability also occur. Of the two peroneal tendons, the peroneus brevis tendon is the most prone to injury as it is closely related to the lateral malleolus. Inflammation may also occur at the insertion of the peroneus brevis tendon at the base of the fifth metatarsal bone (enthesopathy).
Tenosynovitis
Inflammation of the peroneal tendon sheath (tenosynovitis) leads to effusion and hypoechoic synovial thickening with or without Doppler around both tendons.
| In normal individuals, a small amount of fluid can often be found in the tendon sheath, distal to the tip of the malleolus, and should not be mistaken for tenosynovitis. |
Sonopalpation is, as always, very important to establish a correlation between ultrasound findings and focal pain.

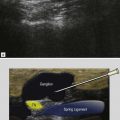
Tenosynovitis may be mechanical, due to overuse or trauma, or associated with inflammatory joint diseases. Traumatic tenosynovitis is seen in patients with ankle derangement and ligament lesions, but it is important to know that effusion in the peroneal tendon sheath may just be a sign of communication to the ankle joint through an acute complete tear of the calcaneofibular ligament. Serous tensosynovitis is frequently found in patients with tendon overuse without a history of trauma, either in a sport setting or in elderly patients. Ultrasonographic signs of tendon tear should always be carefully searched for. In patients with inflammatory joint diseases, e.g. rheumatoid arthritis or gout, tenosynovitis is generally of a proliferative type with marked pannus-like synovial thickening, hyperaemia in patients with active disease, tendinopathy, irregular tendon borders, and thinning or complete tear of the tendons. Calcifications in chronic synovial sheath thickening are rare and seen as echo-rich focal areas with shadowing. They should be distinguished from a fracture of an os peroneum with retraction of the proximal tendon part behind the lateral malleolus. Tenosynovitis may also occur around an accessory peroneal bone, called the painful os peronei syndrome ( Fig. 26.2 ).

Peroneal Tendinopathy and Tendon Tear
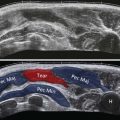
Overuse and chronic tendon instability can lead to tendinopathy with hypoechoic tendon thickening or tendon tear. Peroneal tendon tears are also seen in acute ankle sprains, or in patients with inflammatory joint diseases.
Injuries are not always symptomatic, especially in the older population and are most frequently seen in the retromalleolar part of the peroneus brevis tendon because of its position against the bone.