Chapter Outline
Standard Position 1: Biceps Tendon
Standard Position 2: Rotator Interval
Standard Position 3: Subscapularis Tendon
Standard Position 4: Supraspinatus Tendon
Standard Position 5: Infraspinatus and Teres Minor Tendon
Standard Position 6: Supraspinatus Muscle and Acromioclavicular Joint
DYNAMIC ASSESSMENT OF BURSAL IMPINGEMENT
Overview
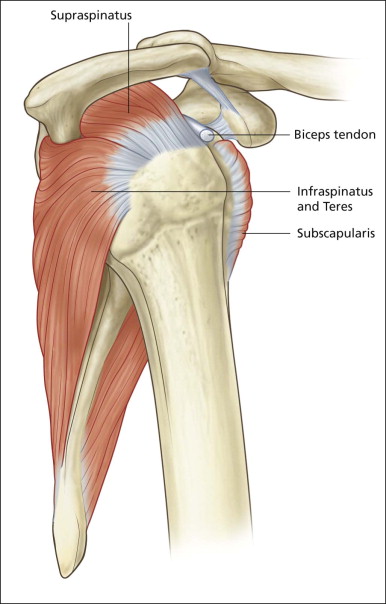
The important bony landmarks in the evaluation of the supraspinatus tendon are the humeral head, the coracoid, the clavicle and acromium, joined at the acromioclavicular joint. The glenohumeral joint is an inherently unstable joint and depends on the surrounding soft tissues for stabilization. Soft tissue stabilizers are divided into intrinsic and extrinsic. The most important extrinsic soft tissues are the supraspinatus tendon superiorly, infraspinatus posteriorly and subscapularis anteriorly ( Fig. 1.1 ). The important intrinsic soft tissue stabilizers are the glenohumeral joint and capsule.
The supraspinatus and infraspinatus are difficult to separate close to their insertions and share what is almost a conjoined tendon. Some of the fibres crisscross each other, making the two tendons difficult to separate. Anteriorly the subscapularis tendon is separated from the supraspinatus tendon by a gap, the rotator interval, which allows passage of the long head of biceps out of the joint and into its groove in the upper arm. The long head of biceps originates from the superior glenoid margin. The coracohumeral ligament helps keep the long head of biceps in position within the upper groove, by forming a sling mechanism in conjunction with the superior glenohumeral ligament. These ligaments pass from the coracoid and glenoid respectively, and insert into the humeral head on either side of the biceps tendon, securing it in place. Another important ligament, the coracoacromial ligament (CAL). Links the coracoid to the acromium and forms the coracoacromial arch along with the bony acromium.
Shoulder pain is a common complaint in the general population and impingement is a common underlying cause. Impingement is a clinical diagnosis, whereby pain occurs during arm abduction, as the supraspinatus tendon and subacromial subdeltoid bursa are compressed between the humeral head and the coracoacromial arch. This clinical scenario is also called painful arc syndrome, as pain is maximal in an arc of abduction between 30° and 60°. Interestingly, patients frequently complain of pain on the lateral deltoid rather than in the region of the acromion.
A complete ultrasound examination involves evaluating the four major tendons of the rotator cuff (biceps, subscapularis, supraspinatus and infraspinatus), the subacromial subdeltoid bursa and the acromioclavicular joint.
Patient Position
The easiest position in which to examine the shoulder is with the patient seated. A stool with either no back or a low back and arms is ideal. This will allow for full access and permit the shoulder to be moved into a range of positions. It is a matter of personal preference whether the examiner carries out the examination standing or sitting, behind or in front of the patient. There are minor advantages and disadvantages to each of these, but none is particularly important and the choice is a matter of personal preference. Some variations in position are required for patients in wheelchairs and for patients who must remain recumbent whether because of illness, surgery or fear of fainting. Many wheelchairs allow the sidearm to be removed, facilitating arm movement. If the patient is also able to sit a little forward in the chair then generally all of the important positions can be achieved without too much difficulty.
It is important to take a history directly from the patient before the examination begins as this can often provide useful diagnostic information. The examination itself begins with a brief inspection of the shoulder, useful to detect muscle wasting. As with most ultrasound examinations the probe should be held lightly with sufficient, but not excessive, contact with the skin. Holding the probe between the thumb and adjacent fingers while resting the little finger on the patient’s skin is an ideal way of obtaining excellent contact with minimal pressure.
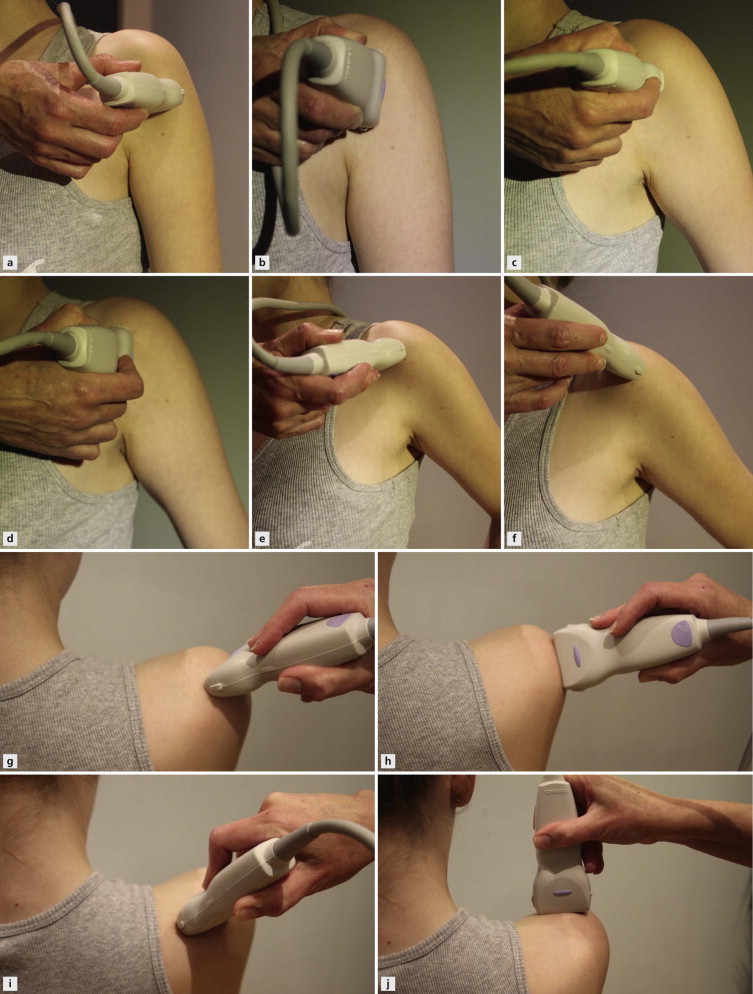
The cuff is examined from biceps anteriorly to teres minor posteriorly and from the acromioclavicular joint superiorly to deltoid insertion inferiorly. The examination is concentrated on the four major tendons, but it is important to have a routine to ensure that none of the other important structures is overlooked. My preference is to begin with the biceps tendon and rotator interval anteriorly, then move sequentially through subscapularis, supraspinatus and infraspinatus and teres in that order ( Fig. 1.2 ). The examination concludes with an assessment of the posterior glenohumeral joint, infraglenoid notch, supraspinatus muscle and the acromioclavicular joint, before sweeping down to the deltoid insertion.
The cuff tendons, particularly supraspinatus, should be examined both statically and dynamically. The static examination is divided into six standard positions with specific imaging goals in each position. The dynamic examination has many components, but primarily seeks to evaluate the behaviour of the subacromial subdeltoid bursa as it abuts the coracoacromial arch on arm abduction.
Standard Position 1: Biceps Tendon
Imaging Goals
- 1.
Confirm that biceps tendon lies within groove.
- 2.
Identify abnormal fluid in the sheath and bursa.
- 3.
Identify normal internal tendon structure.
Technique
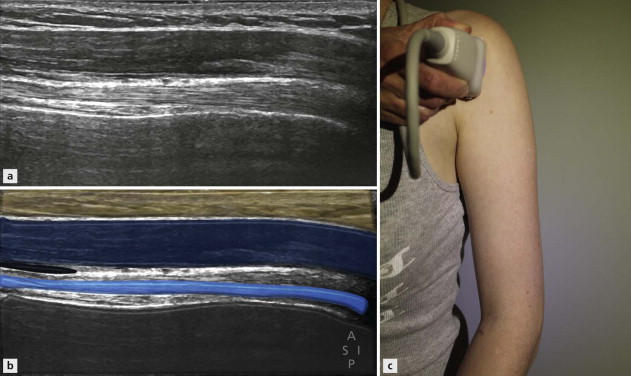
The patient sits and places their hand on their knee palm upwards. This induces a little external rotation sufficient to bring the bicipital groove to an anterior position ( Fig. 1.3 ). The groove is easily located by placing the probe in an axial plane on the anterior aspect of the humeral head. The probe is then moved superiorly and inferiorly, tracing the biceps tendon from the upper part of the groove to below its upper musculotendinous junction. The normal tendon has a bright speckled appearance in the axial plane, made up of the poorly reflective tendon fibre bundles and the hyperechoic connective tissue matrix. Care must be taken to ensure that the probe is always held at 90° to the tendon to remove the effects of anisotropy. Anisotropy is an artefact whereby areas of reduced reflectivity simulating tendinopathy occur as a result of incident echoes arriving at angles other than perpendicular and being reflected away from the tendon, rather than bouncing back to the probe to help form an image.

At its upper part, the biceps tendon sheath surrounds the tendon. As is well known, this is an extension of the glenohumeral joint and a small quantity of fluid is often identified within it. Also in its upper part, the anterior portion of the subacromial subdeltoid bursa can be seen deep to the deltoid muscle and anterior to the biceps sheath. The anterior limb of the circumflex humeral artery is frequently visible around the tendon. Distally, the relationship of the musculotendinous junction with the traversing pectoralis tendon should be noted. A number of tendon variations may be identified. There are often a number of slips that pass from the upper humerus to the tendon. Occasionally a duplex tendon is encountered.
The probe is then rotated 90° so that the tendon can be examined in its long axis ( Fig. 1.4 ). Maintaining the tendon in view during this manoeuvre takes a little practice; however, if the probe falls off the tendon it is very easy to move a little medial or lateral to find it again, noting where the reflective humeral shaft drops away as the probe crosses the groove. In most individuals, the tendon travels deeper as it passes distally. This introduces an element of anisotropy, which can be easily corrected by some gentle pressure at the distal end of the probe. This manoeuvre is called ‘heel toeing’ and is used in several locations in musculoskeletal ultrasound. The long-axis image of the tendon is very useful for confirming integrity; however, as with most tendons, the internal structure is best evaluated in the axial plane.
When assessment of the long head of biceps is complete, the probe is moved medially to locate the short head of biceps. The bony margin of the coracoid process provides a very useful landmark. The short head arises from its inferior margin superficial to the insertion of the pectoralis minor and coracobrachialis tendons. The tendon of pectoralis major can be identified as a long, thin slip passing over the biceps tendon around the level of the proximal musculotendinous junction. The more detailed anatomy of the arm will be covered in a later section. The probe is then returned to the upper biceps to review the rotator interval.
Standard Position 2: Rotator Interval
Imaging Goals
- 1.
Identify ligamentous sling around biceps.
- 2.
Confirm ligaments are intact.
- 3.
Evaluate Doppler signal.
Technique
As has already been mentioned, the rotator interval is the name given to the space between the subscapularis and the supraspinatus tendons through which the long head of biceps passes as it exits the glenohumeral joint. Because the tendon undergoes a 90° turn as it enters the bicipital groove, it must be supported to ensure that it does not displace medially. Two ligaments in particular combine to create this support, which is also referred to as the rotator pulley ( Fig. 1.5 ). The two ligaments are the coracohumeral and the superior glenohumeral ligaments. The pulley is also reinforced by fibres of the subscapularis tendon passing superficially to the coracohumeral ligament and inserting on the lateral aspect of the groove. These fibres are sometimes erroneously referred to as the transverse ligament.
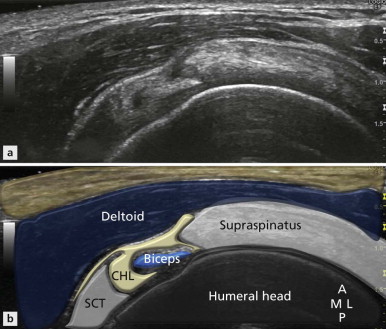
The patient position is the same as for the biceps tendon. The rotator interval is best evaluated with the probe in the axial plane, positioned just above the upper part of the biceps groove. In this position, a rim of tissue is seen around the biceps tendon, between the subscapularis medially and the supraspinatus laterally. This ‘rim’ represents the conjoined coracohumeral and superior glenohumeral ligaments and the bridging subscapularis fibres. The margins of the coracohumeral ligament can usually be identified with good-quality equipment. It measures approximately 1.5 mm in thickness and should have the striated, predominantly reflective appearance typical of ligaments elsewhere. It should have little or no Doppler activity within it.
On the medial aspect of the interval, particularly at its uppermost extent, the contribution from the superior glenohumeral ligament can be identified. This is seen as a nodule of tissue often inserting itself just underneath the biceps tendon and blending with the coracohumeral ligament, from which it is often difficult to separate. Note should be made of thickening or abnormal Doppler activity in and around the coracohumeral ligament, before moving the probe medially to assess subscapularis.
Standard Position 3: Subscapularis Tendon
Imaging Goals
- 1.
Identify tendon in long axis.
- 2.
Identify tendon in short axis.
- 3.
Note relationship of tendon with rotator interval.
Technique
Subscapularis arises, as the name suggests, from the undersurface of the scapula and is an internal rotator of the shoulder. It is a multipennate muscle forming several tendons that insert as a conjoined unit on the medial border of the bicipital groove. The tendon measures approximately 8 cm from superior to inferior. Its upper margin is adjacent to the anterior interval. The tendon must be examined in both its long and short axis, as, because of the width of the tendon, significant tears may be present in one location, yet other areas of the tendon will appear completely normal.
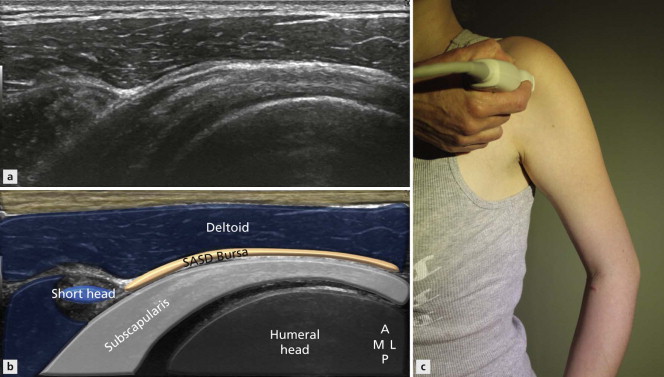
Following a successful examination of the biceps tendon and rotator interval, the patient is asked to move their elbow posteriorly, then, keeping the elbow firmly by their side, the shoulder is externally rotated by asking the patient to move their hand as far as possible laterally. This draws the subscapularis out from beneath the coracoid, making it easier to examine in its full extent ( Fig. 1.6 ). Patients with adhesive capsulitis will find it difficult to externally rotate the shoulder, an important initial clue to this diagnosis. Take care to ensure the patient doesn’t lift their arm to try and simulate external rotation.